Absolute contraindications
Anamnestic
- Serious head injury or stroke in the previous three months.
- Previous intracranial hemorrhage (hemorrhagic stroke, subarachnoid hemorrhage, traumatic hematoma).
- Intracranial neoplasm; arteriovenous malformation or cerebral aneurysm.
- Intracranial or intraspinal intervention in the last 6 months.
- Puncture of a noncompressible artery in the last 7 days.
Clinical
- Symptoms indicating subarachnoid hemorrhage.
- Persistent increase in blood pressure (systolic ≥185 mm Hg or diastolic ≥110 mm Hg).
- Blood glucose <2.8 mmol/l.
- Ongoing internal bleeding.
- Acute bleeding diathesis, including, but not limited to, conditions defined as "hematological".
Hematological
- Platelets <100 G/L*.
- Currently taking anticoagulants with INR >1.7 or PT (prothrombin time) >15 seconds*.
- Administration of heparin in the previous 48 hours in combination with an increase in aPTT*.
- Taking direct thrombin inhibitors or direct inhibitors of coagulation factor Xa in combination with signs of their anticoagulant effect according to laboratory tests such as APTT, INR, ECT, TV or an adequate assessment of Xa activity.
CT scan of the brain
- Signs of hemorrhage.
- Signs of involvement of multiple lobes of the brain, decreased X-ray density extending to >33 percent of the cerebral hemisphere.
Thrombolytic therapy (thrombolysis)
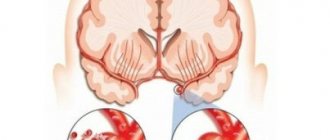
Thrombolytic therapy is a highly effective treatment for ischemic stroke, which allows you to restore blood flow in the affected vessel and prevent irreversible changes in brain tissue.
Currently, for thrombolysis in ischemic stroke, preference is given to alteplase (Actilyse) - the drug has undergone clinical trials and has proven itself well in randomized trials. How it works: Recombinant tissue plasminogen activator (Actilyse) directly activates the conversion of plasminogen to plasmin. After intravenous administration, alteplase remains relatively inactive in the circulation. It is activated by binding to fibrin, which causes the conversion of plasminogen to plasmin and leads to the dissolution of the fibrin clot (the main component of the blood clot).
Thrombolysis is performed in patients with stroke in the first 3-4.5 hours from the onset of neurological symptoms. Only in a hospital, after determining the criteria for indications/contraindications and conducting a number of necessary studies.
Today, VTT is a standard method of treating patients in the most acute period of IS in the absence of contraindications. The method is applicable in most neurological hospitals and does not require lengthy or complex preparation. To make a decision on starting VTT, a relatively small amount of clinical, instrumental and laboratory studies is required. At the same time, due to a significant number of contraindications, only about 5–10% of patients with acute ischemic cerebrovascular accident (ACVA) can potentially be selected for this type of treatment, and the narrow “therapeutic window” (4.5 hours) presents high requirements for the speed of transportation and examination of the patient. The effectiveness of the drug of choice, recombinant tissue plasminogen activator, depends on the level of serum plasminogen, the volume and duration of the thrombus.
However, there are contraindications:
- Bleeding of various localizations. During TLT, all blood clots are dissolved in the vessels, and those that form as a result of bleeding are not excluded.
- Possible aortic dissection.
- Arterial hypertension.
- Intracranial tumors.
- Hemorrhagic stroke (hemorrhage caused by rupture of the walls of cerebral vessels).
- Liver diseases.
- Pregnancy.
- Brain surgeries.
Thrombolytic therapy for ischemic stroke should be carried out in an intensive care unit. According to international recommendations, the time from the patient’s admission to the hospital to the start of thrombolytic therapy should not exceed 60 minutes (door-to-needle time). During this time, it is necessary to determine the indications and exclude contraindications to thrombolytic therapy. Required: 1. Examination by a neurologist and collection of anamnesis, assessment of vital functions and neurological status. An examination using the NIHSS stroke scale is necessary. Thrombolytic therapy is indicated for NIHSS scores between 5 and 25. 2. Immediate CT scan of the brain. 3. Changes in blood pressure levels in both arms. 4. Installation of a cubital peripheral venous catheter. 5. Measuring serum glucose levels. 6. Taking blood and performing the following laboratory tests: a) platelet count; b) APTT; c) INR. 7. Provide monitoring for at least 24 hours: 1) blood pressure levels; 2) heart rate; 3) frequency of respiratory movements; 4) body temperature; 5) oxygen saturation.
Thrombolysis can be:
- Systemic;
- Local.
Methods of thrombolytic therapy
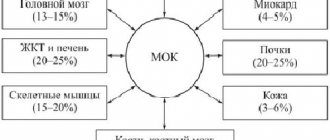
The first method is advantageous in that the medicine can be injected into a vein without having any idea where the blood clot is hidden. With the bloodstream, the drug is carried throughout the entire blood circulation, where on its way it encounters an obstacle in the form of a blood clot and dissolves it. But systemic thrombolysis has a significant drawback: an increased dose of medication is required, and this is an additional burden on the entire circulatory system.
INDICATIONS FOR THROMBOLYSIS IN ACUTE ISCHEMIC STROKE: • severe neurological deficit associated with acute ischemic stroke and, apparently, caused by occlusion of a large artery (basilar, vertebral, internal carotid): a form of movement disorder, speech disorder, facial paresis, level of consciousness disorder. Using special scales (NIHS scale), a neurologist assesses the level of neurological deficit. • absence of hemorrhage according to computed tomography • development time from the beginning of the clinic to 3 hours (up to 6 hours with selective thrombolysis, up to 12 hours with infarction in the main artery basin) THROMBOLYSIS CONTRAINDICATION: ABSOLUTE CONTRAINDICATIONS: 1) minor and rapidly regressing neurological deficit 2) hemorrhage, clearly visible extensive acute cerebral infarction or other CT data that are contraindications (tumor, abscess, etc.) 3) convincing evidence of the presence of a vascular malformation or tumor of the central nervous system in the patient 4) bacterial endocarditis RELATIVE CONTRAINDICATIONS: 1) severe trauma or stroke in within the past 3 months 2) history of intracranial bleeding or suspected diagnosis of subarachnoid hemorrhage 3) major surgery within the past 2 weeks 4) minor surgery within the past 14 days, including liver or kidney biopsy, thoracentesis and lumbar puncture 5) arterial puncture within the past 2 weeks 6) pregnancy (ten days after birth) and breastfeeding 7) acute gastrointestinal bleeding, urological or pulmonary bleeding in the last three weeks, history of hemorrhagic diathesis (including renal and liver failure) 9) peritoneal or hemodialysis 10) changes in coagulogram ( PTT more than 40 seconds, prothrombin time more than 15 (INR more than 1.7), platelets less than 100,000) 11) convulsive seizure as the onset of a stroke (careful differential diagnosis is required) 12) changes in blood glucose levels (hypo or hyperglycemia) ADMINISTRATION OF THE DRUG: Non-selective thrombolysis is more often carried out. To carry it out, after a minimal examination of the patient (examination by a neurologist, computed tomography to exclude hemorrhage), a general blood test with platelet levels, blood biochemistry (glucose level), coagulogram, if possible), 100 mg of the drug akilyse is administered intravenously: 10 mg is administered as a bolus, the rest 90 mg – intravenous drip on physical therapy. solution 0.9% 400.0 for 1 hour. COMPLICATIONS OF THROMBOLYSIS: The main complications are the risk of bleeding (nasal, gastrointestinal, renal) and the risk of transformation of the ischemic focus into hemorrhage in the brain. Thrombolytic therapy makes it possible to witness a truly dramatic improvement in the patient’s condition, when severe neurological disorders literally disappear “on the needle”, and he not only survives, but also recovers, which was previously almost impossible.
Using special scales (NIHS scale), a neurologist assesses the level of neurological deficit. • absence of hemorrhage according to computed tomography • development time from the beginning of the clinic to 3 hours (up to 6 hours with selective thrombolysis, up to 12 hours with infarction in the main artery basin) THROMBOLYSIS CONTRAINDICATION: ABSOLUTE CONTRAINDICATIONS: 1) minor and rapidly regressing neurological deficit 2) hemorrhage, clearly visible extensive acute cerebral infarction or other CT data that are contraindications (tumor, abscess, etc.) 3) convincing evidence of the presence of a vascular malformation or tumor of the central nervous system in the patient 4) bacterial endocarditis RELATIVE CONTRAINDICATIONS: 1) severe trauma or stroke in within the past 3 months 2) history of intracranial bleeding or suspected diagnosis of subarachnoid hemorrhage 3) major surgery within the past 2 weeks 4) minor surgery within the past 14 days, including liver or kidney biopsy, thoracentesis and lumbar puncture 5) arterial puncture within the past 2 weeks 6) pregnancy (ten days after birth) and breastfeeding 7) acute gastrointestinal bleeding, urological or pulmonary bleeding in the last three weeks, history of hemorrhagic diathesis (including renal and liver failure) 9) peritoneal or hemodialysis 10) changes in coagulogram ( PTT more than 40 seconds, prothrombin time more than 15 (INR more than 1.7), platelets less than 100,000) 11) convulsive seizure as the onset of a stroke (careful differential diagnosis is required) 12) changes in blood glucose levels (hypo or hyperglycemia) ADMINISTRATION OF THE DRUG: Non-selective thrombolysis is more often carried out. To carry it out, after a minimal examination of the patient (examination by a neurologist, computed tomography to exclude hemorrhage), a general blood test with platelet levels, blood biochemistry (glucose level), coagulogram, if possible), 100 mg of the drug akilyse is administered intravenously: 10 mg is administered as a bolus, the rest 90 mg – intravenous drip on physical therapy. solution 0.9% 400.0 for 1 hour. COMPLICATIONS OF THROMBOLYSIS: The main complications are the risk of bleeding (nasal, gastrointestinal, renal) and the risk of transformation of the ischemic focus into hemorrhage in the brain. Thrombolytic therapy makes it possible to witness a truly dramatic improvement in the patient’s condition, when severe neurological disorders literally disappear “on the needle”, and he not only survives, but also recovers, which was previously almost impossible.
Local thrombolysis: During local thrombolysis, the drug is injected directly into the location of the thrombus. The drug is supplied through a catheter, which is why the method is called catheter thrombolysis. However, this method is more difficult to implement than the first and is associated with a certain danger. During the procedure, the doctor monitors the movement of the catheter using x-rays. The advantage of this method is its low invasiveness. It is used even if the patient has a large number of chronic diseases.
Own results
Below is data describing the experience of one doctor. The counting of thrombolytic procedures used began in June 2021 (Fig. 1). In total, from June to December 2021, 44 TLT procedures were performed, from January to July 2021 - 37, thus, in total, during the period under review, this procedure was performed 81 times.
An analysis of the possibilities of use and effectiveness of TLT was carried out on the basis of data obtained for the period from January to July 2021.
Note that we were able to use TLT to help patients with IS only in 30% of cases. What factors have limited the use of TLT?
According to researchers of this problem [3], such factors are:
time of initiation of therapy;
the presence and size of a brain region with potentially reversible changes;
features of systemic and local hemodynamics;
hemostasis factors;
sensitivity of the brain substance to ischemia;
the degree of damage to the blood-brain barrier [3].
The time factor, which comes first in this list, is determined by the presence/absence of a window of therapeutic opportunity (4.5 hours from the onset of stroke). Our observations confirm its significance among all the obstacles limiting the use of TLT: out of 103 patients hospitalized by us with a diagnosis of IS, 52 (50.5%) were outside the therapeutic window (Table 1). However, in most cases, even with a window of therapeutic opportunity, we had to act under deadline conditions, since in real conditions we are often faced with the simultaneous admission of several patients requiring immediate examination and diagnostic procedures. The objective difficulties associated with this lead to inevitable losses of already strictly limited time. The speed and coherence of the actions of the medical staff involved in the TLT procedure and the uninterrupted operation of diagnostic equipment are of great, often decisive importance. Table 1 provides data illustrating the relationship between the time factor and other factors that impede TLT. Thus, the impossibility of performing thrombolysis in 17.5% of cases was associated with the presence of such contraindications in patients as uncontrolled arterial hypertension, trophic disorders in joints and limbs, and blood clotting problems. In approximately 2% of cases, we encountered patients refusing TLT.
In addition to the time factor, the presence of contraindications, the consent of the patient and his relatives when performing TLT, it is important to take into account the age of the patients. According to the instructions for use of the drug alteplase, the recommendations of the European Stroke Organization, and the Russian clinical guidelines for thrombolytic therapy for ischemic stroke [5], patients under 18 years of age should not undergo TLT, and patients over 80 years of age —
carry out with extreme caution. Most researchers agree that TLT in people over 80 years of age is not associated with an increase in complications, such as hemorrhagic transformation of the brain lesion, and, therefore, does not lead to an increase in mortality [6]. A good degree of recovery of impaired neurological functions (26–30%) serves as evidence that thrombolysis in patients aged 80–89 years and 90–99 years is equally safe and effective [6].
Regarding young patients (up to 45 years), data are provided indicating a more favorable outcome of the disease with a low incidence of symptomatic hemorrhagic transformation and a better degree of restoration of impaired neurological functions [6]. On this basis, it is concluded that TLT is effective and safe in all age groups. However, the older the patients, the higher the number of functionally unfavorable outcomes and deaths [6].
Further in our work, we tried to trace the relationship between the effectiveness and safety of TLT and the gender and age of patients. The results of TLT were assessed as follows:
positive dynamics—regression of neurological deficit with successful recanalization and reperfusion;
lack of dynamics - no changes are observed due to the lack of recanalization and/or the development of irreversible damage to the brain substance in the lesion;
negative dynamics - clinical deterioration (manifested by the development of complications, primarily hemorrhagic, reocclusion or re-embolism, or an increase in cerebral edema in case of insignificant effect of TLT).
Table 2 presents data that allows us to trace the relationship between the effectiveness of TLT and the gender and age of patients. We divided our patients into 6 age groups: 1st (20–49 years), 2nd (50–59 years), 3rd (60–69 years), 4th (70–79 years); 5th (80–89 years), 6th (90 or more years). The effectiveness and safety of TLT (positive dynamics, no dynamics, negative dynamics, absence/presence of allergic reactions) was assessed based on the results of daily observation. According to Russian clinical guidelines for thrombolytic therapy for ischemic stroke, it is necessary to monitor the dynamics of the neurological status during the day; Positive dynamics during the first 24 hours after TLT, as a rule, predict subsequent good recovery [5].
Summarizing our observations, we can provide the following data.
The total number of patients who underwent the TLT procedure was 37. There were no cases of an allergic reaction.
The number of men and women among our patients turned out to be almost equal (19 and 18 people, respectively).
The oldest age group (90–99 years) is represented by a single patient - a 92-year-old woman, who, as a result of TLT, showed positive dynamics (restoration of facial expression and speech disorders).
The largest group (10 people) are patients aged 60–69 years, the number of men and women is the same. The results of TLT in each of the subgroups were the same: in 4 men and 4 women, complete or partial restoration of impaired functions was noted (positive dynamics); in 1 man and 1 woman there was no dynamics (no changes occurred); the TLT effectiveness rate in this group is the highest - 82%; No negative dynamics were observed among representatives of this group.
According to the effectiveness of the thrombolytic procedure, age groups can be ranked as follows:
60–69 years old - 82%;
20–49 years old - 80%;
50–59 years old - 75%;
70–79 years old - 43%;
80–89 years old - 33%.
(The group of 90–99 years old, consisting of 1 person, is not included in the rating.)
Cases of negative dynamics with a fatal outcome were noted in 2 groups (70–79 years old and 80–89 years old): a 79-year-old woman and an 84-year-old man. However, in both cases, according to the pathological and anatomical study, a direct connection between the death and the TLT procedure was not established. In the age group of 80–89 years, there was 1 case of hemorrhagic transformation (in an 88-year-old man).
The total number of women who experienced complete or partial recovery of impaired functions after TLT (14 people, 58%) exceeds the number of men with positive dynamics (10 people, 42%).
The overall effectiveness of TLT is quite high and amounts to 64.9% (24 people out of 37) against 8.1% (3 people) of cases of negative effect and 27% (10 people) of the absence of any effect of this procedure.