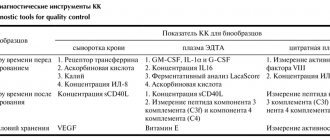
Detailed description of the study
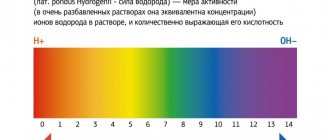
Alkaline phosphatases (ALP) are a group of enzymes that catalyze the reaction of the removal of phosphates from various molecules, usually proteins. The name of enzymes is due to the fact that they exhibit maximum biochemical activity in an alkaline environment.
Alkaline phosphatase is a collective term: in the body the enzyme is presented in the form of several fractions. The largest amount of alkaline phosphatase is found in the liver, the walls of the bile ducts and bones, and to a lesser extent in the intestinal mucosa, kidneys and placenta - an organ formed during pregnancy to connect mother and fetus. Normally, 80% of the ALP level in the blood consists of the liver and bone fractions of the enzyme.
As an enzyme, alkaline phosphatases catalyze reactions in the formation of components of cell membranes (phospholipids), carbohydrates, ATP molecules (the main source of energy in the body) and other nucleotides, as well as bone tissue structures.
Under physiological conditions, serum alkaline phosphatase levels may vary with age. In young children and adolescents, enzyme concentrations may increase as a result of bone growth and development. Adult men may have lower ALP values than women.
Also, a physiological increase in the enzyme can be observed in pregnant women, especially during the third trimester. This is due to the active production of alkaline phosphatase by the placenta. In the presence of clinical symptoms - most often itching and less often yellowing of the skin - an increase in alkaline phosphatase may indicate cholestasis in pregnancy. In this case, you need to consult your doctor as soon as possible.
Excessive levels of alkaline phosphatase in the blood can occur in pathologies of the bone and urinary systems. However, most often the indicator increases in diseases of the liver and biliary tract.
Bile is a biological fluid that is formed in the liver. Its main functions include:
- Emulsification and absorption of fats in the wall of the small intestine;
- Removal of bilirubin and cholesterol from the body.
Liver cells secrete bile, which first enters the cavity of the duodenum (small) intestine through intrahepatic and then through extrahepatic ducts. Part of the bile is stored in a special organ located on the lower surface of the liver - the gallbladder.
When the outflow of bile is disrupted, stagnation occurs (cholestasis). The causes of this pathological condition can be different - stone getting into the ducts, compression of them by a tumor, etc. Clinically, cholestasis can occur in the form of skin itching, less often jaundice (yellowness of the sclera, skin and/or mucous membranes, darkening of urine and discoloration of feces) - for due to the large amount of bilirubin entering the blood from the liver.
It has been established that with cholestasis the level of alkaline phosphatase in the serum begins to increase sharply. This is a response of the liver in response to a violation of the outflow of bile. Moreover, if the obstacle is at the level of the extrahepatic ducts, the increase in alkaline phosphatase in the blood is more pronounced.
This study is advisable to carry out when diagnosing the following diseases:
- Obstructive jaundice due to cholelithiasis, neoplasms of the liver, bile ducts, pancreas;
- Liver inflammation, cirrhosis due to infectious, autoimmune and other pathologies;
- Malignant bone tumors and bone metastases.
Cholinesterase (ChE)
An enzyme that is involved in the destruction of acetylcholine, a chemical carrier of impulses in excitable tissues (muscle, nervous).
It binds to the liver and represents the main marker of the functional activity of this organ. That is, if something happens to the liver, then, of course, its ability to synthesize something decreases, and because of this, the content of those substances in the blood that should normally be produced in large quantities decreases. Norm:
5300-12900 units/l.
Increase:
physiological (in the first trimester of pregnancy), pathological (obesity, diabetes mellitus, tetanus, breast cancer, nephrosis, arterial hypertension).
Decreased:
usually in late pregnancy, with the use of certain drugs (anabolic steroids, glucocorticoids), as well as during the period of postoperative rehabilitation.
Important:
a decrease in ChE is a sign of destructive liver diseases, acute insecticide poisoning, and myocardial infarction.
Clinical observation 3
Boy P., born 02/23/2009. Born at 36 weeks. with signs of malnutrition: height - 51 cm, weight - 2850. Subsequently, when assessing height gains, a decrease in growth rates was noted starting from 1 year. In the period from 2 to 7 years, growth rates ranged from 3.5 to 7 cm, which corresponded to the 5th percentile for the observation period. From the age of 3–4 years, periodic complaints of pain in the arms and legs at rest, fatigue during normal physiological stress, headaches at rest and after emotional stress with a frequency of 1 time in 1–2 weeks, which were relieved with the help of non-steroidal anti-inflammatory drugs, were noted. .
At the age of 5 years and 3 months. We consulted a pediatric endocrinologist about short stature (height SD -2.37). Hospitalization was recommended for examination in a hospital, where primary idiopathic subclinical hypothyroidism was identified. According to laboratory data: thyroid-stimulating hormone 12 µIU/ml, free thyroxine 18.6 pmol/l. Ultrasound picture of the thyroid gland without pathology, the right lobe is 2.1 cm2, the left is 1.5 cm2, the isthmus is 1.6 mm. Therapy with sodium L-thyroxine at a dose of 25 mcg was initiated.
At 6 years and 9 months. during radiographic examination, the bone age corresponded to the biological age of 3.5 years. At 7 years of age, the growth rate is +6.4 cm/year, growth CO is -2.1. Indications for a stimulation test with clonidine were determined, but the mother refused the test.
At 6 years and 2 months. For the first time, a decrease in the level of alkaline phosphatase was registered - 88 U/l, with repeated measurements a year later - 108 U/l (normal: 150–550 U/l).
Taking into account the syndrome of short stature in combination with damage to the musculoskeletal system (pain in the extremities, poor posture, deformation of the chest), a significant delay in bone age according to radiography, and a persistent decrease in the level of alkaline phosphatase, the patient underwent a molecular genetic study and the mutation p.571 was identified. G>A in the ALPL
in a heterozygous state
.
A diagnosis was made: hypophosphatasia, childhood form.
From January 2021, after a consultation, taking into account the progressive nature of the disease, it was decided to initiate enzyme replacement therapy with the drug asfotase alfa at a dose of 2 mg per 1 kg of body weight, 3 times a week. subcutaneously
The beginning of therapy was accompanied by episodes of hyperthermia, with a reaction at the injection site (twice), however, after desensitizing therapy and following the recommendations for a hypoallergenic diet, the reactions were stopped, the patient continued to receive treatment.
During treatment, stable positive dynamics are observed: a significant increase in growth rates, an increase in muscle strength and tolerance to physical activity, and pain in the lower extremities has been relieved. The child continues the recommended treatment.
Amylase
This is the main digestive enzyme that breaks down glycogen and starch, as well as sugar, and provides the body with glucose.
It is found in large quantities in the pancreas (from which, as part of pancreatic juice, it enters the lumen of the duodenum to begin its work - digestion) and in the salivary glands (yes, the process of breaking down carbohydrates begins in the mouth). That is why if something happens to the pancreas, amylase immediately lets you know about it. There are several varieties of this enzyme: α-amylase, β-amylase, γ-amylase, but the most common and therefore most indicative is used in diagnosis - α-amylase. Norm:
20-100 units/l.
Increase:
acute pancreatitis (already 4 hours after the onset of the attack increases by 8 times), exacerbation of chronic pancreatitis (increases by 3-5 times), pancreatic tumors, stones in the ducts, alcohol intoxication, as well as infectious parotitis (mumps), ectopic pregnancy.
Decreased:
pancreatic necrosis, cystic fibrosis (hereditary disease of the enzyme system).
Lactate dehydrogenase (LDH)
An enzyme that is contained in organs responsible for processing glucose, and in an oxygen-free cycle.
Yes, to begin with, it must be said that the main path of glucose breakdown occurs with the participation of oxygen, and oxygen-free oxidation is a “backup” process, but necessary in the early stages, when the oxygen cycle has not yet “turned on.” Why is glucose breakdown needed at all? This is the main process by which we obtain energy. LDH actively manifests itself in the heart, liver, kidneys, spleen, pancreas, and muscles. It converts lactate (the product of oxygen-free oxidation of glucose) into pyruvate, which then enters the final oxidation cycle and produces the maximum possible amount of energy. Interestingly, LDH has several isoforms - from LDH1 to LDH5, and all of them are found in different organs (LDH 1.2 - in the heart, a late marker of myocardial infarction, LDH4.5 - in the liver, during the destruction of liver tissue). Norm:
140-350 units/l.
Increase:
physiological - can be caused during pregnancy, after exercise and drinking alcohol, as well as taking caffeine, aspirin, insulin, heparin, interferon, and some antibiotics.
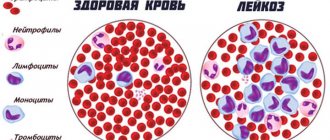
Pathological - occurs with myocardial infarction, acute or toxic hepatitis, cirrhosis and tumors in the liver, muscle injuries, acute pancreatitis, acute kidney pathologies and blood diseases (hemolytic anemia, B12-deficiency anemia, leukemia). Decrease:
in destructive kidney diseases, when the process has been going on for a long time, the function gradually decreases and the filtration of urea is impaired, which eventually appears in the blood (uremia).
How to return alkaline phosphatase to normal?
The level of alkaline phosphatase in the blood will return to normal on its own as soon as you eliminate the cause of the deviation. Those. It is necessary to influence not the ALP itself, but the factors that led to its increase or decrease.
Minor abnormalities should not be a cause for concern because enzyme levels fluctuate throughout the day and vary from person to person.
If a patient has an acute deficiency of vitamins and minerals, he should enrich his diet with the following foods:
- fresh fruits and vegetables, especially citrus fruits and dark leafy greens
- red meat and fatty fish
- unrefined vegetable oil (olive, sesame, camelina, flaxseed, corn, etc.)
- whole grain cereals
- natural probiotics (yogurt, kefir, kimchi and sauerkraut)
If there are liver problems, you should eat according to the recommendations of the classic therapeutic diet Table No. 5. The patient will also need to normalize their weight and increase physical activity. Drug support traditionally includes ursodeoxycholic acid (UDCA), a drug for the hepatobiliary system with a high degree of evidence. It protects liver cells from damage, reduces the load on the organ, allowing it to recover faster. In case of serious pathologies (cirrhosis, cancer, viral hepatitis), antiviral therapy and surgical intervention may be required.
A patient with a gallbladder is first monitored dynamically. If the situation worsens, despite the use of UDCA, cholecystectomy is prescribed - removal of the bladder.
Interpretation:
- Paget's disease, physiological bone growth, malabsorption syndrome, nutritional deficiency (D-dependent rickets), vitamin D-resistant rickets, iatrogenic rickets (anticonvulsants), osteoporosis, osteomalacia, including in hyperparathyroidism, osteosarcoma, healing of bone fractures, metastatic prostate or breast cancer with osteoblastic bone formation, lymphoma, leukemia, storage diseases (Gaucher disease, Niemann-Pick disease), uremic bone disease
- Osteopenia (with genetic hypophosphatasemia), hypothyroidism, chronic nutritional deficiency (lack of magnesium, zinc, vitamin B12), pernicious anemia, scurvy
Sample result (PDF)
Lipase
Another digestive enzyme, the “homeland” of which is the pancreas.
It participates in the breakdown of fats, “biting off” long fatty acids from triglycerides. Just like amylase, it is part of pancreatic juice and increases in the blood during pancreatic diseases. However, it is more specific because it remains within the normal range for ectopic pregnancy, acute appendicitis, infectious mumps and liver diseases. Also, its activity in acute pancreatitis may increase earlier than amylase activity, and this is associated with greater diagnostic value. Norm:
13-60 units/ml.
Increased:
acute pancreatitis, malignant neoplasms of the pancreas, cholestasis, metabolic diseases (gout, obesity, diabetes), taking certain medications (indomethacin, barbiturate sleeping pills, heparin, narcotic painkillers).
Decreased:
hereditary lipid pathologies (triglyceridemia), unhealthy diet with a lot of fat, removed pancreas, tumors of any location except the pancreas.
Tags:
- Blood
To leave a comment you must be an authorized user
Introduction
Hypophosphatasia (HPP) is a multisystem progressive hereditary metabolic disease, often leading to life-threatening conditions and disability in patients [1]. HPP develops as a result of mutations in the ALPL
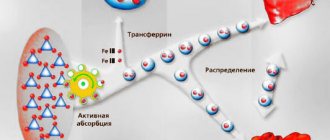
, which encodes the enzyme - tissue-specific alkaline phosphatase (ALP), which is actively involved in the mineralization of bone tissue and the metabolism of vitamin B6 in the central nervous system. Inheritance of mutations can occur either in an autosomal dominant or an autosomal recessive manner [2]. The presence of a pathogenic mutation leads to a decrease in the activity of tissue-nonspecific ALP and extracellular accumulation of enzyme substrates: mainly inorganic pyrophosphate (an inhibitor of the formation of hydroxyapatite crystals and bone mineralization) and pyridoxal-5'-phosphate (the main circulating form of vitamin B6, which cannot overcome the activity of ALP). blood-brain barrier) [1, 3].
Disturbances in the process of bone tissue mineralization and vitamin B6 metabolism in the central nervous system determine the clinical picture of the disease. GFF is characterized by defects in the formation and development of the musculoskeletal system - shortening, all kinds of deformities of the limbs, chest, and skull. Typically, children experience low body weight and growth retardation. With age, the risk of pathological, poorly consolidating fractures requiring surgical treatment increases. Due to muscle and bone pain, patients experience gait disturbances and progressive limitation of mobility with the need to use crutches and wheelchairs [1, 3].
Changes in the structure of the ribs and the shape of the chest lead to impaired breathing, secondary pulmonary hypoplasia and severe respiratory disorders with the need to use methods of artificial pulmonary ventilation (ALV) [4].
Hypercalcemia, caused by impaired calcium-phosphorus metabolism, is often accompanied by the development of foci of ectopic calcification, and primarily nephrocalcinosis with the development of progressive kidney damage. For the same reason, rheumatological manifestations in the form of arthritis and pseudogout are possible in adult patients [3, 4].
Neurological symptoms include: vitamin B6-dependent seizures, intracranial hemorrhages, muscle hypotonia, delayed psychomotor development. Disruption of the formation of cranial bones can lead to craniosynostosis with increased intracranial pressure, which may require emergency surgical correction [5].
One of the characteristic signs of HFF is the premature loss of primary or permanent teeth, most often with an intact root, due to disruption of the mineralization process of the organic matrix of dentin and cement in the dental alveoli [6].
The classification of GFF is based on the age of onset of the first symptoms; there are 4 main forms: perinatal - when signs are detected in utero or immediately at birth; infantile - from 0 to 6 months; children's room - from 6 months. up to 18 years old; adults - after 18 years. In case of isolated dental damage, odontohypophosphatasia is separately distinguished [3].
The most severe clinical symptoms appear in early forms of HFF, perinatal and infantile, where respiratory and neurological disorders come to the fore, which are the main cause of death. The pediatric form is more characterized by progressive skeletal damage with increasing rickets-like deformities, limited mobility and severe disability [1, 4].
Diagnosis of HFF
is established based on a combination of clinical symptoms with low alkaline phosphatase activity (taking into account the age and gender of the patients), hypercalcemia/hyperphosphatemia and a characteristic x-ray picture. X-rays of long tubular bones reveal various deformations, osteoporosis, areas of hypomineralization alternating with osteosclerosis, as well as expansion and erosion of growth zones; in the metaphyses, the so-called “tongues of flame” are identified - areas of clearing that extend from the growth zone in the direction of the diaphysis. In early forms, a typical sign of HFF is the presence of osteochondral outgrowths on the diaphysis (Bowdler spurs). In all children, as a rule, bone age lags behind passport age [3].
If necessary, to definitively confirm the diagnosis, an additional molecular genetic study is performed to identify a mutation in the ALPL gene.
Until recently, treatment with HFF
was exclusively symptomatic: a diet with a low calcium content, prescription of vitamin D for its deficiency, vitamin B6 for seizures, surgical assistance for fractures or the development of craniostenosis, physiotherapy and therapeutic exercises to strengthen the musculoskeletal system [3, 7].
Attempts have been made to treat HPF with high-dose vitamin D, bisphosphonates, or teriparatide. However, none of these approaches led to the desired results. Vitamin D may exacerbate pre-existing hypercalcemia, especially in young children; bisphosphonates, being, in fact, an analogue of inorganic pyrophosphate, a natural substrate of alkaline phosphatase, inhibit the mineralization process, worsening the course of the disease; teriparatide (recombinant human parathyroid hormone) in studies on rats in high doses induced the development of osteosarcoma in bone growth areas and is contraindicated for use in children [7].
In 2021, a drug for enzyme replacement therapy of GFF was registered in the Russian Federation - recombinant human ALP. International nonproprietary name - asfotase alfa.
In the State Budgetary Institution of Children's Clinical Hospital in Krasnodar, 3 patients are observed with a diagnosis of HFF with perinatal and pediatric clinical forms. We present our experience of diagnosis and first treatment results in these clinical observations.
Creatine phosphokinase (CPK)
An enzyme that provides energy to muscles, mainly striated muscles (skeletal and cardiac).
It is located inside muscle cells and is responsible for the transfer of phosphoric acid residue to creatine and the resulting activation of energy metabolism. We have already mentioned many times above that intracellular enzymes, increasing in the blood, indicate that destruction of a specific tissue is occurring somewhere. In the case of CC, this tissue is muscle. This is the earliest and most specific marker of myocardial infarction; its activation can be detected within two hours after the occurrence of a focus of necrosis in the heart muscle. Norm:
up to 190 units/l for men, up to 167 units/l for women.
Increased:
myocardial infarction, myocarditis, myocardial dystrophy, heart failure, tachycardia, hypothyroidism, malignant tumors and some diseases of the central nervous system (schizophrenia, psychoses, epilespy, head injury).
It can also increase after operations and diagnostic manipulations on the heart, after physical activity. Decrease:
sedentary lifestyle, severe decrease in muscle mass, cachexia (exhaustion).