Complexes with this research
Women's check-up No. 1 38 studies for an annual preventive examination 11,530 ₽ Composition
Men's check-up No. 1 39 studies for an annual preventive examination 10,930 ₽ Composition
Examination during pregnancy. 3rd trimester 5 360 ₽ Composition
IN OTHER COMPLEXES
- Pregnancy planning. Clinical indicators RUB 3,620
- Biochemistry of blood. 8 indicators 990 ₽
- Female infertility RUB 9,310
- Causes of hair loss RUB 1,840
- Joining IVF RUB 14,350
Suitability of biological material for research in various fields
Blood serum
Hemolysis.
You can check for Hb contamination and ensure that the sample is suitable for proteomic or miRNA-based analysis using ELISA or spectrophotometry. If the Hb concentration is above 50 mg/l, hemolysis has occurred, and the sample is considered contaminated with Hb [9].
Inflammation.
You can check for the presence of an inflammatory marker in a sample by measuring the concentration of C-reactive protein (CRP) using ELISA or nephelometry. If the concentration is above 10 mg/L, the sample indicates the presence of inflammation [9].
Suitability for cardiovascular disease research.
To establish suitability for research, it is necessary to measure:
a) level of BNP, NT-proBNP, using ELISA;
b) ANFPTL3 level using ELISA or electrochemiluminescent immunoassay;
c) level of CK-MB and ET-1 using ELISA;
d) MMP-3 and MMP-9 level using ELISA;
e) troponin I and troponin T levels using ELISA or electrochemiluminescence immunoassay.
These proteins must be detected in order for the sample to be used in cardiovascular disease research [9].
Suitability for liver disease research.
Alanine aminotransferase (ALT) levels should be measured using a fluoroimmunoassay. ALT must be detectable for the sample to be suitable for liver disease testing [9].
Suitability
for the purpose of autoimmunity research.
For research, it is necessary to determine the level of tumor necrosis factor-α (TNF-α) using a sensitive ELISA. TNF-α must be detectable for a sample to meet the criteria for autoimmunity testing [9].
Suitability for research
in endocrinology and diabetes.
Insulin C peptide and insulin growth factor II precursor levels should be measured using ELISA, fluoroimmunoassay, or radioimmunoassay; Aldosterone and somatomedin C levels using ELISA. These proteins must be detected for the sample to be relevant for endocrinology research [9].
Suitable for inflammation
and immunology research.
Complement C levels should be measured using nepholometry or an enzyme immunoassay; ICAM-1 and TNF-α levels by enzymatic immunoassay. These proteins must be detected for the sample to be relevant for inflammation and immunology studies [9].
Suitability
for research purposes in oncology.
To check you need to: use ELISA M65 EpiDeath; measure VCAM-1 levels using ELISA. These proteins must be detectable for the sample to be relevant for oncology research [9].
Suitability for research purposes
in the field of musculoskeletal diseases.
MID-osteocalcin, osteocalcin and calcitonin levels, as well as C-terminal telopeptide and collagen type 1, intact parathyroid hormone (PTH) should be measured using ELISA or electrochemiluminescence immunoassay. These proteins must be detected in order for the sample to be used in research in the field of musculoskeletal diseases [9].
Suitability for
nutrition .
Vitamin B12 levels should be measured using an electrochemiluminescence immunoassay. Vitamin B12 must be detectable for a sample to meet nutritional study criteria [9].
Suitability for research into neurodegenerative diseases.
To establish eligibility for such studies, amyloid Aβ42 levels must be measured by ELISA; neuron-specific enolase levels using the Kryptor immunoassay, ELISA, or electrochemiluminescent immunoassay. These proteins must be detectable for the sample to be relevant for research into neurodegenerative diseases [9].
Blood plasma (EDTA
and
citrate)
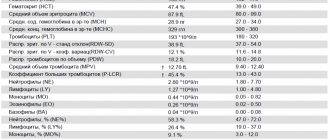
Platelet contamination.
You can check for platelets and ensure that the sample is suitable for microparticle or ccfRNA analysis by performing a cell count. If the platelet concentration is below 104/ml, it is considered that there is no significant contamination of the plasma sample with platelets [9].
Platelet activation.
You can also test platelet activation and ensure that the sample is suitable for testing biomarkers affected by platelet activation by measuring the concentration of β-thromboglobulin (βTG) using ELISA. If the concentration is above 200 ng/ml, platelet activation occurs [9].
Hemolysis.
You can check for Hb contamination and ensure that the sample is suitable for proteomic or miRNA analysis by performing ELISA or spectrophotometry. If the Hb concentration is above 20 mg/L, hemolysis has occurred and the sample is considered contaminated with Hb [9].
Inflammation.
You can check the severity of inflammation in a sample by measuring the concentration of CRP using ELISA or nephelometry. Concentrations above 10 mg/l indicate inflammation [9].
Suitability for cardiovascular disease research.
To establish eligibility for research, troponin I and troponin T levels must be measured using ELISA or electrochemiluminescence immunoassay; vasoactive intestinal peptide (VIP) level using ELISA.
These proteins must be detected for the sample to be relevant for cardiovascular disease research [9].
Suitability for studying lipid metabolism.
To test, levels of CETP transporter protein activity can be measured using a fluoroimmunoassay. CETP must be detectable for a sample to qualify for lipid metabolism/lipidomics testing [9].
Suitability for autoimmunity research.
For this study, TNF-α can be measured using a sensitive ELISA. TNF-α must be detectable for a sample to meet the criteria for autoimmunity testing [9].
Suitability for research purposes
in the field of endocrinology, including diabetes.
To assess suitability, glucagon-like peptide 1 levels can be measured using ELISA or radioimmunoassay; adenocorticotropic hormone levels using electrochemiluminescence immunoassay or radioimmunoassay; aldosterone and somatomedin C levels using ELISA.
These proteins must be detected for the sample to be relevant for endocrinology research, including diabetes mellitus [9].
Suitable for inflammation
and immunology research.
To check, you can measure: complement C levels using nepholometry or enzymatic immunoassay; ICAM-1 level by enzymatic immunoassay. These proteins must be detected for the sample to be suitable for inflammation and immunology studies [9].
Suitability for research purposes in musculoskeletal disorders.
C-terminal telopeptide and type I collagen levels should be measured using ELISA or electrochemiluminescent immunoassay. These proteins must be detectable in order for the sample to be used for research in the field of musculoskeletal diseases [9].
Suitability for research into neurodegenerative diseases.
To establish eligibility for research, amyloid Aβ42 levels can be measured using an ELISA. Aβ42 must be detectable for the sample to be suitable for the study of neurodegenerative diseases [9].
Suitability for coagulation studies
(for citrate plasma only). Antifactor Xa and fibrinogen levels can be measured to check; prothrombin fragments 1 and 2 and plasminogen activator inhibitor type 1 activity or antigen using ELISA; analysis of thrombin generation using fluoroimmunoassay; TRA antigen using ELISA. These proteins must be detectable for the sample to be of the required quality to study the coagulation process [9].
Detailed description of the study
Serum iron is a microelement that is not produced in the human body independently, but comes only from the outside with food.
Iron is included in:
- Hemoglobin, which is the main carrier of oxygen from the lungs to tissues and organs;
- Myoglobin, which is located in the muscles and is responsible for creating an oxygen reserve.
Iron also participates in cellular metabolism, in the functioning of the immune system, is part of some enzymes, ensuring the normal occurrence of metabolic reactions in them, and also participates in DNA synthesis.
In total, the body contains no more than 5 g of iron. It comes from food from animal and plant sources. This is the so-called heme (found in meat products, as part of hemoglobin) and non-heme (enzymes and proteins of plant foods) iron. Of the total amount of iron that enters the body, only about 10% is absorbed. The absorption process occurs in the duodenum.
In human blood plasma, most of the iron is in the oxidized trivalent state, bound to the protein transferrin. Transferrin transports iron to tissues and organs. Most of the incoming iron goes into the formation of hemoglobin, and the rest is deposited (stored). The main depot of iron in the body is the special protein complexes “ferritin” and “hemosiderin”. From here, iron is consumed if it decreases in the blood serum. The restoration of iron in the blood serum depends on the degree of depot filling. With prolonged iron deficiency, iron reserves are depleted, which can lead to anemia. This regulatory mechanism ensures self-preservation.
Serum iron concentration is an important biochemical indicator, changes in which may indicate possible problems in the metabolism of this microelement.
Iron deficiency is more common than iron excess. As a rule, a person does not notice that he is developing anemia - a pathological decrease in the concentration of hemoglobin in the blood. This usually becomes noticeable when the hemoglobin concentration drops below 100 g/l. Then the person may complain of increased fatigue, dizziness, hair loss, pale skin and brittle nails. In some cases, people report a tingling and burning sensation on the tip of the tongue.
If you do not take any action aimed at restoring the iron depot, shortness of breath, absent-mindedness, and rapid heartbeat (tachycardia) further develop.
Similar conditions are observed in cancer (especially if the intestines are affected), iron deficiency anemia, jaundice, acute and chronic infections, peptic ulcers and ulcerative colitis. Iron deficiency can often be caused by chronic blood loss from hemorrhoids. In case of celiac disease, Crohn's disease and in the postoperative period, anemia is also diagnosed. Iron concentrations in women vary depending on the phase of the menstrual cycle.
There is also the so-called “anemia of pregnancy” - a condition in which the concentration of serum iron in pregnant women decreases. As a rule, in the second trimester, when the fetal iron depot is formed. This condition also requires special monitoring.
Iron overload is less common and is characterized by the following symptoms: abdominal and joint pain, heart rhythm disturbances, and fatigue, similar to anemia.
For the normal functioning of all organs and systems, it is necessary that at least 1 mg of iron be supplied with food per day. Foods rich in this microelement: meat and offal (pork liver), legumes (lentils, beans), greens (spinach, celery), fruits (pomegranate, apples). Ascorbic acid improves the absorption of iron, so it is recommended to use it together with iron-containing foods. Dairy products and caffeine can interfere with iron absorption.
Importance of sample quality control
Quality control (QC) of biospecimens used for scientific research is of fundamental importance to ensure the reliability of the data obtained. Uniformity of biospecimen collection, transport, and storage procedures is critical to ensure the quality of multicenter research studies.
An important and effective tool for such standardization and preservation of a large number of biological samples is the creation of a biobank. A biobank is a structure for the collection, storage and delivery of biological samples and associated data that follows standard operating procedures and provides materials for scientific use [2].
All biospecimens are subject to collection, transportation, sample preparation and storage procedures. Procedures in the biobank are performed strictly according to accepted standards, otherwise the quality of biosamples may decrease. The collection of biomaterial is carried out by medical personnel according to standard methods in accordance with clause 3.2 of GOST 53079.4 - 2008 [3]. Next, the biomaterial, along with the necessary documents, is transported to the biobank, where sample preparation and registration of the resulting biomaterial is carried out (Fig. 1).
Rice. 1. “Life cycle” of biospecimens.
Table 1. QC diagnostic tools
Table 2. Suitability of biological material for research in various fields
Blood sample preparation includes centrifugation and further aliquoting of serum or plasma. In accordance with the standard, it is necessary to perform blood centrifugation no later than 1 hour after collection. Then the aliquoted biomaterial is stored in freezers at a temperature of –80 °C.
QC procedures are designed to evaluate data and biospecimens used in scientific research. QC of data includes control of demographic, clinical information, accuracy of data processing, while QC of biological samples includes analyzes for the authenticity, integrity and identity of samples [1]. QC of biological samples is necessary to ensure accurate characterization and categorization of samples, and to avoid errors in subsequent studies due to inherent heterogeneity within samples.
QC procedures may be carried out by the biobank, end user or subcontracted laboratory and should be performed in compliance with GLP (Good Laboratory Practice) rules or ISO 15189:2012 (Medical laboratories - specific requirements for quality and competence), ISO 17025:2005 or CLIA (Clinical laboratory improvements) [4-6].
Retrospective QC can be applied either to randomly selected samples or to samples whose quality is most in doubt. The first approach allows comparison of different collection sites, while the second allows targeted assessment of samples with the “highest risk” [2].
References
- Federal clinical guidelines for the diagnosis and treatment of iron deficiency anemia, 2015. - 58 p.
- Klochkova-Abelyants, S.A., Surzhikova, G.S. Iron deficiency anemia and anemia of chronic diseases: some aspects of pathogenesis and prospects for differential diagnosis. — Medicine in Kuzbass, 2021. — No. 3. — P.25-28.
- Tiglis, M., Neagu, T., Niculae, A. et al. Incidence of Iron Deficiency and the Role of Intravenous Iron Use in the Perioperative Period, 2021. - Vol. 56(10). - P. 528.
Indications
The main indications for a blood test for allergens is the presence of the reaction itself. It can be expressed by a number of symptoms:
- hyperemia of the skin and mucous membranes;
- peeling or cracking of the skin;
- obsessive itching and burning of the skin and mucous membranes;
- lacrimation;
- runny nose;
- dry cough or shortness of breath.
In addition to acute conditions with allergies, a history of diseases becomes a reason for blood tests for antigens to allergens:
- bronchial asthma;
- rhinitis of allergic origin;
- hay fever;
- conjunctivitis of unknown origin;
- urticaria and dermatitis, including atopic;
- Quincke's edema.
Since blood tests for allergens are more expensive than diagnostics using other methods, for example, skin testing, they are carried out when the latter are ineffective or due to the impossibility of their implementation. Such situations include:
- exacerbation of allergic dermatitis with rashes in the forearms or back (the places where tests are most often done);
- exacerbation of skin diseases of an inflammatory and infectious nature;
- exacerbation of diseases in which it is necessary to take antihistamines that affect the accuracy of the results of contact tests;
- history of anaphylactic shock.
Blood tests for allergens are also prescribed if skin tests give a positive result for several types of irritants.
Decoding the results
The purpose of a blood test for allergies and a marker confirming its presence is specific immunoglobulin E or IgE. The body synthesizes them in response to irritating substances, and by their amount per ml of blood (or serum), an allergist can determine the severity of the allergic reaction, that is, its class. There are six in total in each allergen panel:
- Zero class - the content of IgE immunoglobulins per ml of blood is less than 0.35 units. With this result, there is no allergy to the irritant.
- The first class is the IgE content per ml of blood in the range from 0.35 to 0.7 units. There is a high probability of an allergy to the product, but the reaction will be extremely mild, without significant symptoms.
- The second class is the content of immunoglobulins E up to 3.5 per 1 ml of blood. This result indicates an allergy that is mild and cannot cause life-threatening complications.
- Third class - the IgE content per ml of blood reaches 17.5 units. A pronounced allergy with visually distinguishable signs and striking respiratory, dermatological, food and other symptoms.
- The fourth class is the content of immunoglobulins up to 50 units. This result indicates an obvious allergy, accompanied by severe symptoms that reduce the patient's quality of life.
- Fifth class - the blood contains up to 100 IgE immunoglobulins. Indicates a strong allergic reaction with the development of complications in the form of an asthma attack, Quincke's edema.
- Sixth class - more than 100 type E immunoglobulins per 1 ml are detected in the blood. Indicates severe forms of allergies, which require constant monitoring and strict limitation of contact with irritants. During an exacerbation, patients with class 6 allergies require emergency medical care.
The interpretation of the results is provided in the form of a table indicating the allergens and the values of immunoglobulins for them.
Preparing for analysis
Despite the high sensitivity and specificity, preparation is recommended to obtain reliable results from blood tests for allergens. The accuracy of the result will depend on compliance with the recommendation. The following are considered mandatory preparation points for a blood test for allergens:
- abstaining from eating for 8 hours before collecting materials;
- reducing the allergenic load on the body 3 days before donating blood - excluding citrus fruits, eggs, honey, chocolate, foods with dyes and flavors, and nuts from the diet;
- limiting physical activity the day before blood sampling;
- limiting stressful situations a day before collecting materials for analysis;
- quit smoking at least 2-3 hours before the test.
It is not recommended to donate blood for allergy tests during exacerbation of any diseases, including allergic ones. If seasonal allergies are suspected, research is carried out in the autumn-winter period, when plants do not bloom.
The essence of the method, types and features
To understand the essence of blood tests for allergens, it is important to understand the mechanism of the occurrence of atypical immune reactions to certain substances. So, when they enter the body, the immune system reacts by releasing antibodies, which can:
- cause severe tissue swelling and destroy cell membranes, as a result of which their functioning changes;
- initiates the formation of proteins capable of destroying the walls of blood vessels;
- initiates the synthesis of sensitized lymphocytes, which trigger the process of purulent or pus-like processes.
All these phenomena are in one way or another associated with the synthesis by the immune system of IgE - immunoglobulins that quickly respond to the arrival of an irritant, or IgG - immunoglobulins that form slowly and are detected in the blood several hours after contact with allergens. Each of them is characterized by a specific structure, according to which they can be correlated with specific stimuli. It is these immunoglobulins that are detected in blood tests for allergens.
There are two types of blood tests for allergens:
- Enzyme-linked immunosorbent test (ELISA or ELISA technology).
- Blood test for eosinophils.
Blood analysis using ELISA technology (from the English enzyme-linked immunosorbent assay) allows you to determine the quantity and quality of specific low-molecular compounds, macromolecular structures, proteins, including antigens, antibodies, viruses. To carry out the analysis, enzymes are used, which act as a kind of marker of the body’s specific reaction to certain substances.
Key features of the method:
- high accuracy of results - errors in the diagnosis of allergic reactions are excluded;
- high sensitivity - the analysis allows you to determine an atypical reaction of the body even with an ultra-low content of immunoglobulins in the blood;
- high specificity of the analysis - it determines with 100% accuracy which stimulus the immune system reacts to in an atypical manner;
- a wide range of reagents for determining a variety of allergens, including rare ones;
- safety of tests - the analysis does not involve the risk of a violent reaction of the body to irritants, and is approved for use even in patients with a tendency to develop anaphylactic shock.
Allergen blood tests are designed to detect groups of antigens and antibodies associated with specific foods or substances. To determine them, several allergen panels are used:
- Food Panel, IgE for food allergens, which contains reagents that allow you to determine hypersensitivity to food products - citrus fruits, apples, bananas, peaches, several types of nuts, seafood, flour (wheat, rye and others), animal proteins (meat, milk, eggs), seafood and fish, soybeans and crabs;
- Respiratory Panel, IgE for respiratory allergens, which contains reagents for detecting antigens and antibodies to substances that cause allergic rhinitis, hay fever, sinusitis or other types of allergic reactions provoked by substances received during inhalation - dust and dust mites, tree pollen and flowers, meadow and cultivated grasses, epithelium and animal hair (horse, guinea pig, dog and cat, rodents), fungi and mold;
- Pediatric Panel, IgE for irritants that cause allergic reactions in young children - house dust, pet epithelium, pollen of common trees and grasses, cow's milk and its proteins, eggs, vegetables, nuts, flour products;
- a medicinal panel containing irritants from the group of antibiotics, as well as drugs based on animal proteins;
- ImmunoCAP ISAC, an allergy chip with 112 components that provoke common and rare forms of reactions - the main household allergens (dust, wool), animal hair, food, pollen and animal proteins, nuts, flour products, vegetables and fruits, etc.
There are also less extensive panels containing no more than 12-20 allergens, grouped according to a certain criterion: by the origin of the allergens, by the risks of encountering them in specific conditions, etc. The survey results contain information on each allergen, so this analysis is good for a comprehensive diagnostics and identification of all potentially dangerous irritants.
A blood test for eosinophil levels is often used before an enzyme immunoassay for allergens. It shows the presence of specific proteins in the blood - eosinophils - indicating a developing allergic reaction. This analysis is cheaper and is available even for small laboratories. However, it only confirms the fact that the cause of the ailment was an allergy, and does not determine the type of irritant and the degree of its destructive effect on the body.