Against the background of coronavirus infection, blood oxygen saturation may drop sharply, and serious health problems will begin. In case of lack of oxygen, doctors often talk about hypoxemia. What is it?
Hypoxemia is a word derived from the ancient Greek “hypo” (a prefix denoting weakness) and the New Latin oxygenium - oxygen. In fact, this term, experts note, hides a decrease in the oxygen content in human blood. The causes of this condition can be various options - from circulatory disorders to a decrease in hemoglobin. With hypoxemia, pressure often decreases, and saturation also drops below normal values.
Why is it developing?
Doctors identify several main reasons for the development of hypoxemia, as well as a number of provoking conditions. Among the causes of lack of oxygen in the blood are:
- Atypical blood shunting - this situation can occur against the background of heart defects, when venous blood begins to flow into the aorta - in this case, hemoglobin loses its ability to attach oxygen.
- Problems with insufficient ventilation in the lungs - this happens when the frequency of exhalations and inhalations slows down, as a result of which, naturally, the supply of oxygen to the body decreases. Here they usually talk about a whole list of problems, including chest injuries, obstruction in the bronchi, inflammatory processes, such as pneumonia, collapse of part of the lung, etc.
- Anemia - when the level of hemoglobin decreases, the level of oxygen transported to the tissues begins to decrease.
- Diffusion disorders - due to increased physical activity, blood circulation begins to accelerate, as a result of which the amount of time required for hemoglobin to contact with oxygen decreases.
Also, a lack of oxygen in the blood can develop against the background of such a bad habit as smoking, with lung diseases, overweight and obesity, with changes in atmospheric pressure and with a decrease in the concentration of oxygen in the air.
How to measure blood oxygen levels at home? More details
Heart failure and hypoxemia in patients with acute myocardial infarction
Z
and over a long-term observation period,
acute heart failure retains the leading role in the structure of mortality from acute myocardial infarction (AMI), accounting for 52% of the total number of lethal complications
[1]. Acute heart failure is a consequence of myocardial necrosis and leads to a decrease in the pumping function of the heart and the development of hypoxia - an early and permanent sign of circulatory failure in acute myocardial infarction.
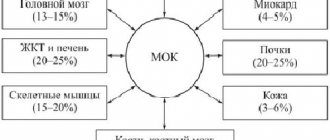
The mechanism of the circulatory element of hypoxia is that due to a decrease in cardiac output, an increase in arteriovenous extraction of oxygen occurs (a slowdown in blood flow with a constant release of O2 from hemoglobin to mitochondria). In addition, a possible mechanism of so-called shunt tissue hypoxia is a consequence of increased arteriovenous shunting, when normal or increased pO2 may occur in mixed venous blood, despite low end-capillary pO2. Low partial pressure of O2 in capillary blood leads to a decrease in the average diffusion gradient for O2 from the erythrocyte to the mitochondrion. The arteriovenous shunt in the skin can account for more than 10% of cardiac output [2]. The mechanisms of cardiogenic respiratory failure seem to be extremely important in the pathogenesis of hypoxemia and subsequent tissue hypoxia. Cardiogenic respiratory failure
is the result of involvement of the lungs in the pathological process due to failure of the pumping function of the myocardium. A physiologically significant increase in end-diastolic pressure of the left ventricle or pressure in the left atrium invariably leads to a retrograde increase in pressure in the pulmonary vessels and forms post-capillary, passive pulmonary hypertension. In accordance with the Starling equation, with an increase in hydrostatic pressure in the pulmonary circulation, the rate of fluid filtration through the microvascular endothelium into the interstitium increases. When fluid is filtered faster than it is removed by the lymphatic system, perivascular, interstitial, and then alveolar pulmonary edema develops. From a mechanical point of view, lung damage can be characterized as restrictive disorders manifested by changes in lung volumes. Heart failure is characterized by a decrease in the vital capacity of the lungs, the residual volume and functional residual capacity of the lungs are not changed or almost unchanged, the total lung capacity is less than expected [3–5]. The decrease in the total capacity of the lungs is due to a decrease in the elastic properties of the lung parenchyma: as a result of edema of the interstitium and the walls of the alveoli, the stiffness of the lungs increases and their extensibility decreases. As this process increases, the phenomenon of early expiratory closure of the airways may develop with a significant increase in residual volume and a decrease in total lung capacity [6]. A progressive decrease in lung capacity and their distensibility leads to an increase in pleural pressure necessary for inhalation, and, consequently, to an increase in the work of breathing [7].
On the other hand, if there is an excessively large fluctuation in inspiratory (negative) pressure in the pleural cavities due to upper airway obstruction or low lung compliance, cardiac output may be reduced due to a significant increase in left ventricular afterload. In addition, such low pleural, and therefore pulmonary interstitial pressure, can increase the extravascular water content in the lungs and thereby aggravate restrictive and diffusion disorders [8]. The patient compensates for the increased work of breathing by decreasing tidal volume and increasing respiratory rate.
Pulmonary congestion has been shown to influence resistance in the distal airways [9]. Thus, the mechanical factor leads to impaired ventilation due to the development of airway obstruction and decreased compliance of the lung tissue. In case of left ventricular failure, interregional and intraregional inhomogeneity of the lungs leads to the development of regional alveolar hypoxia [10]. An increase in pulmonary artery wedge pressure leads to a pathological distribution of perfusion with a reversal of the apical-basal gradient [11–13]. The presence of obstructive and restrictive respiratory failure, uneven perfusion-ventilation relationships, and increased work of breathing determine the possibility of using respiratory support methods in patients with acute myocardial infarction complicated by left ventricular failure and, consequently, cardiogenic respiratory failure.
The simplest and most logical method of correcting hypoxemia in this situation seems to be inhalation of pure oxygen or a gas mixture with increased oxygen content, but their negative effect on pressure in the pulmonary circulation, systemic vascular resistance and cardiac output in patients with congestive heart failure has been shown [14] , which limits the possibilities of using the method and forces us to consider the possibility of mechanical respiratory support.
Materials and methods
23 patients with acute myocardial infarction complicated by heart failure were examined. Of these: men – 17, women – 6, patients with primary myocardial infarction – 3, with repeated myocardial infarction – 20. The average age of patients is 62.4±2.4. According to the location of myocardial damage, patients were distributed as follows: anterior myocardial infarction - 18, posterior myocardial infarction - 3, myocardial infarction of the lower wall of the left ventricle - 2. The diagnosis of myocardial infarction was confirmed by the totality of the clinical picture, changes in the electrocardiogram, and the dynamics of cardiac-specific enzymes. The diagnosis of heart failure was based on the clinical picture: shortness of breath at rest, the presence of moist, soft rales in the lungs, decreased oxygenation of arterial blood according to pulse oximetry. All patients received standard therapy for acute myocardial infarction and maximum drug therapy for left ventricular failure (intravenous morphine, nitrates under blood pressure control, diuretics, if necessary, dopamine or dobutamine in doses of 1 to 10 mcg/kg/min, cardiac glycosides). All patients underwent measurement of central hemodynamic parameters and determination of cardiac output using the thermodilution method using an AS 3 device from DATEX with calculation of derivative hemodynamic values, determination of the gas composition of arterial and mixed venous blood, followed by calculation of oxygen transport indicators. In addition, standard monitoring was carried out, including ECG, respiratory rate and pulse oximetry. After the initial examination, the patients received respiratory support using a Puritan Bennett 7200 device in CPAP mode with a CPAP (continuous positive airway pressure) setting of 4.2 ± 2.7 cm H2O or PS (pressure support) 17.6 ± 5.7 cm H2O, after which a similar examination was carried out again.
results
The research results were processed in the standard Excel statistical program (two-sample t-test with different variances). Good and satisfactory tolerability of non-invasive positive pressure ventilation (NIPPV) was observed in 92% of patients. Among the complications, we note the following: pressure of the mask on the face, difficulty exhaling (with PEEP more than 8 cm H2O), decreased blood pressure (with an initial PAWP of 5 mm Hg), bedsores from the pressure of the mask on the face (with a ventilation duration of 7 days).
Clinical improvement was recorded in 87% of patients within the first 20–30 minutes. carrying out NIPPV and was expressed in a decrease in respiratory rate and heart rate, an improvement in the psycho-emotional state, a decrease in cyanosis and acrocyanosis, and a significant decrease in the amount of moist congestive rales in the lungs.
We obtained the following data on changes in central hemodynamics and blood gas composition (Table 1).
As can be seen from the data presented in the table, under the influence of NIPPV there was a significant decrease in respiratory rate, heart rate (HR), a decrease in the average pressure in the pulmonary artery (Avg.PAP), pulmonary artery wedge pressure (PAWP), and an increase in the index of shock work of the left ventricle (LVSI) without a significant decrease in the right ventricular stroke index (RVSI). There was an increase in the partial pressure of oxygen in arterial (pO2A) and mixed venous blood (pO2LA). Blood shunt (Qs/Qt) decreased.
Thus, the method of pressure support and constantly increased pressure in the airways, without having a negative effect on central hemodynamics, allows you to correct hypoxemia, transport and oxygen consumption in patients with cardiogenic respiratory failure
caused by acute myocardial infarction.
Non-invasiveness, good tolerability, effectiveness, and lack of need for sedation make methods of non-invasive respiratory support in patients with symptoms of acute heart failure complicating acute myocardial infarction an important component in treatment.
conclusions
- Noninvasive ventilation is well tolerated by patients with AMI complicated by acute left ventricular failure.
- Under the influence of NIPPV, these patients experienced a significant decrease in hydrostatic pulmonary capillary pressure without inhibiting the pumping function of the heart.
- Noninvasive ventilation made it possible to significantly reduce the degree of hypoxemia and reduce the percentage of blood shunting in the lungs without increasing the fraction of inspired oxygen.
- Against the background of non-invasive ventilation, there was a rapid clinical improvement in the patients' condition due to the relief or reduction of the degree of pulmonary edema.
Literature:
1. Golikov A.P. Achievements and prospects for scientific research in the field of emergency cardiology. Cardiology. Volume 41. 09. 2001. pp. 47–50.
2. Ole Siggaard–Andersen, Niels Fogh–Andersen, Ivar H.Gothen, Vagn Hojkjaer Larsen //Oxygen status of arterial and mixed venous blood.–Critical Care Medicine.–1995.vol.25.No.7.
3. Frank. NR. Lyons, H.A. Siebens. A.A., and Nealon. TF: Pulmonary compliance in patients with cardiac disease. Am. J. Med. 22:516, 1957;
4. Wood, T. E., McLeod, P., Anthonisen, N. R., and Macklem. PT: Mechanics of breathing in mitral stenosis. Am. Rev. Resp. Dis. 104:52, 1971.
5. Saxton, G. A., Jr., Rabinowitz, M., Dexter, L., and Haynes, F.: The relationship of pulmonary compliance to pulmonary vascular pressures in patients with heart disease. J. Clin. Invest. 35:611, 1965.
6. Collins JV, Clark. TJH, and Brown DJ Airway function in healthy subjects and in patients with left heart disease. Clin. Sci. Molec. Med. 49:217, 1975.
7. Marshall R., McRoy MB, and Christie RV: The work of breathing in mitral stenosis. Clin. Sci. 13:137, 1954.
8. Perel A., Pizov R. Cardiovascular effects of mechanical ventilation. In: Mechanical ventilatory support. Perel A., Stok M.Ch. (Ed.), Baltimore, Williams & Williams, 1994, 308.
9. Collins JV, Clark. TJH, and Brown DJ Airway function in healthy subjects and in patients with left heart disease. Clin. Sci. Molec. Med. 49:217, 1975.
10. Raine, J., and Bishop, JM: The distribution of alveolar ventilation in mitral stenosis at rest and after exercise. Clin. Sci. 24:63, 1963.
11. James, AE, Jr., Cooper, M., White, RI, and Wagner, HN, Jr.: Perfusion changes on lungs in patients with congestive heart taillires. Radiology 100:99, 1971.
12. Giuntini, C., Mariani, M., Barsotti, A., Fazio, F., and Santolicandro. A.,: Factors affecting regional pulmonary blood flow in left heart valvular disease. Am. J. Med. 57:421, 1974.
13. Pain, M. C. F., Bucens, D., Cade, J. F., and Sloman, J. G.: Regional lung function in patients with mitral stenosis. Aust. NZJ Med. :228, 1972.
14. Wasim A. Haque, MD, Joohn Boehmer, Barry S. Clemson, Urs A. Hemodinamic Effects of Supplemental Oxygen Administration in Congestive Heart Failure. JACC Vol.27, No.2 February 1996,353–357.
How to recognize the problem?
Hypoxemia is represented by a number of symptoms that you should definitely pay attention to in order to consult a doctor in time. After all, a lack of oxygen can be an extremely dangerous condition that leads to an imbalance in the body as a whole.
So, hypoxemia will be indicated:
- increased heart rate and breathing;
- drowsiness;
- change in skin color towards pallor;
- weakness in general;
- dizziness.
If you ignore such signals from the body, later manifestations may develop, fraught with serious complications. For example, disruptions in the functioning of the heart, the development of severe swelling, problems with the functioning of the brain, as it does not receive enough nutrition. The skin may also take on a bluish tint. A person may experience anxiety, forgetfulness, and sleep problems. Potential complications include decreased blood pressure, stroke conditions, risks of developing pulmonary edema, convulsive effects, and heart rhythm disturbances.
Clinical symptoms
The insidiousness of the disease is that it does not manifest itself immediately. At the very beginning, when the body is still actively fighting, the following appears:
- Slight tachycardia
- Skin becomes slightly pale
- Blood pressure increases by several points
If measures are not taken, the disease begins to progress. And then its late signs appear:
- Cyanosis, that is, pronounced blueness of the skin, first on the earlobes, around the lips and fingertips, and then throughout the body
- The sweat becomes very sticky and cold
- The patient experiences persistent dizziness
- Motor restlessness, which gives way to stupor
- Serious neurological disorders
The outcome depends on the severity of the disease, on existing pathologies, and most importantly, on timely therapy. If hypoxemia is acute, its prognosis is very unfavorable. The list of complications includes:
- Severe arrhythmias, rapid drop in blood pressure, significant decrease in contractility of the heart muscle
- Strokes and encephalopathy
- Shortness of breath, disturbances in respiratory rhythm, pulmonary edema
How to identify the problem?
To identify heart problems, you should undergo a thorough examination by a specialist. He will take a medical history and conduct an examination. It is also recommended to use pulse oximetry to check the level of oxygen in the blood - today it is not a problem to carry it out even at home using a portable device. In addition, X-rays of the lungs and ultrasound of the heart are prescribed to exclude pathologies that can lead to a state of hypoxemia. It is recommended to take a blood test to check for a sufficient amount of hemoglobin and the absence of anemia.
How often should healthy people check their saturation? More details
Oxygen starvation in newborns
In newborns, breathing rhythm disturbances and short-term apnea are also sometimes observed during sleep. In mild cases, the pause lasts from 10 to 15 seconds, and then the child begins to breathe on his own. In more severe situations, there is no breathing for more than 20 seconds, which is very dangerous for the baby’s life.
In severe cases, signs of sleep apnea in children include blueness of the skin, lips and nails; these symptoms are associated with deterioration of cardiac function. Repeated, prolonged episodes of apnea lead to mental retardation. The violation threatens to increase the risk of sudden neonatal death syndrome and therefore requires immediate treatment.
Treatment of hypoxemia
Therapy for this condition depends on the root cause - after all, it is necessary to deal with it first. Also, if necessary, specialized therapy can be prescribed aimed at restoring redox reactions in the body, thinning the blood if necessary, reducing pressure in the corresponding circulatory system, etc. Naturally, it is performed exclusively as prescribed by a doctor based on existing symptoms and after assessing the patient's condition. Sometimes additional oxygen therapy is added.
Preventive actions
There are also a number of preventive measures that will reduce the risk of developing hypoxemia and prevent the development of serious complications. At the same time, they are quite simple and accessible to everyone. So, on the list of preventive measures:
- walks in the fresh air every day;
- physical activity, which should be moderate;
- practice breathing exercises (in consultation with a doctor);
- using vitamins and minerals in your diet;
- timely examinations by specialists to identify risks of developing cardiovascular and pulmonary diseases;
- rejection of bad habits.
Doctors note that hypoxemia is a preventable condition. The main thing is not to ignore signals from the body and correctly build your daily schedule.
There are contraindications, you should consult your doctor