Death from heart attack is extremely common in many countries around the world, so it is extremely important to think about preventing myocardial infarction as early as possible.
Despite the fact that myocardial infarction has become noticeably “younger” in recent years, older people still remain at risk. However, the development of a heart attack can be prevented if you pay due attention to your health and follow medical recommendations.
What is a heart attack
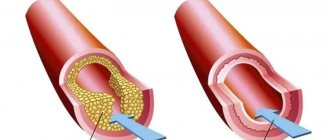
A heart attack is one of the types of coronary heart disease. The attack occurs due to insufficient or completely stopped blood supply to the myocardium. The most common cause of this effect is blood clots that form in blood vessels.
Acute pain in the heart area can be completely sudden. Depending on the degree of localization, the human body is able to return to life or coronary death occurs. As a result of the pain syndrome, the heart muscles die, which affects the further functioning of the cardiovascular system.
Those at risk are mainly elderly people, active and passive smokers. Concomitant diseases such as alcoholism, diabetes, obesity, and blood vessel diseases can also cause a heart attack. According to statistics, heart attacks most often affect men and people leading a sedentary lifestyle.
Who is at risk?
Despite the high incidence of myocardial infarction, there are groups of people whose risk of having a heart attack is higher than others. The risk group often includes:
- Males - in women, heart attacks are half as common.
- Older people - the risk of heart attack increases sharply after 50.
- Overweight people.
- Alcohol abusers.
- Smokers.
- Persons burdened by heredity: if close relatives have had a heart attack, the risk of getting sick increases.
- The presence of concomitant ailments: diabetes, rheumatism, other heart diseases.
In addition to factors that we cannot influence, such as age, gender or genetic predisposition, there are things that are completely within our power. Move more, give up alcohol and tobacco, and reconsider your eating habits - and the risk of having a heart attack will decrease significantly.
Symptoms of a heart attack
Harbingers of a heart attack can be a wide variety of pain that occurs not only in the heart area, but under the shoulder blades, in the stomach or throat. Nagging pain in the limbs may also indicate problems with the functioning of the heart.
The main symptom of a heart attack is sharp, unbearable pain in the chest. The attack may last several minutes or not go away for hours. A heart attack can be primary (spontaneous) or repeated at regular intervals.
In medicine, there are five main types of heart attack, each of which manifests itself with different symptoms. A typical form of heart attack develops with a sharp burning pain in the heart area.
In the asthmatic form, a sudden attack of suffocation occurs. The patient does not have enough air, his breathing quickens several times. The eyelids, fingers, lips and nose area acquire a rich blue tint. The underlying skin suddenly turns pale. Such a heart attack may be accompanied by hemoptysis, coughing and noisy, uneven breathing.
The arrhythmic form is directly related to changes in heart rate. The patient's pulse quickens, the heartbeat becomes visually noticeable, and blood pressure decreases several times. This form of heart attack most often leads to clinical death.
The cerebral form is accompanied by a sudden loss of consciousness. Moreover, the initial signs of a heart attack are very similar to a stroke. The patient cannot pronounce words coherently, his speech becomes incomprehensible, coordination of movements is impaired, and sharp pain occurs in the chest area.
The abdominal form of heart attack is considered the rarest. Pain in this case does not occur in the heart area, but in the abdominal cavity closer to the stomach. According to some signs, such an attack resembles an exacerbation of an ulcer or gastritis. A heart attack is accompanied by profuse sweating, rapid heartbeat, tachycardia, arrhythmia, nausea and vomiting.
Main signs of a heart attack
Close signs of an imminent heart attack are more aggressive and vivid in nature. The imminent development of acute ischemic heart pathology can be determined by the following close warning signs of a heart attack:
- by the appearance of moderate pain in the left side of the body, chest or shoulder, sensations of moderate compression or tightness in this area;
- development of severe shortness of breath without serious physical exertion, difficulty breathing;
- a drop in blood pressure below working values;
- increased sweating;
- detection of slight numbness of the limbs, which may not occur with this condition.
Sometimes short-term manifestations of a heart attack can be accompanied by a strong attack of unreasonable fear of death, panic attacks, the so-called angina attack.
Detection of such symptoms definitely requires contacting a doctor as early as possible and receiving specific treatment - treating such attacks at home is IMPOSSIBLE and can be life-threatening!
Patient Reminder
o The threat of a recurrent heart attack is increased by four main factors: atherosclerosis, high blood pressure, increased blood clotting and carbohydrate metabolism disorders.
These risk factors can only be controlled with the help of properly selected drug therapy.
o To slow down the further development of atherosclerosis, it is important to prevent the formation of fatty plaques in the vessels.
For this purpose, drugs from the statin group are prescribed. Beta blockers help the heart work more calmly. So-called angiotensin-converting enzyme inhibitors reduce the effect of the vasoconstrictor angiotensin and normalize blood pressure.
o You cannot change the dosage of medications at your own discretion.
If any problems arise, the doctor will adjust the course of treatment.
for recovery after a heart attack :
minimum fat, nothing fried or spicy, more fiber, dairy products, fruits, vegetables, fish.
We will have to give up sausages and sausages, ready-made semi-finished products
(dumplings, cutlets...) - they contain a lot of hidden fats that increase cholesterol levels.
For the same reason, pates, liver dishes, offal, and caviar are prohibited.
Milk fat is also dangerous: you will have to exclude butter; fatty cottage cheese, cheese, milk, kefir, sour cream, cream. When cooking chicken or turkey, all fat and skin must be removed from the carcass.
And of course, a minimum of salt
.
Vodka, cognac and other strong drinks are canceled.
But
you can afford a glass of natural dry red wine
; this is a good prevention of atherosclerosis.
You'll have to change some habits too. If you used to smoke, cigarettes are now completely taboo
.
To restore the functioning of the heart muscle, it is important to engage in physical therapy. Walking is a great restorative.
After just one and a half to two months of training, you can walk at a pace of up to 80 steps per minute without shortness of breath or weakness. And over time, switch to very fast walking - up to 120 steps per minute.
Useful: climbing stairs, cycling, swimming. Dancing
2-3 times a week for 30-40 minutes.
However , make sure that your heart rate during exercise does not exceed more than 70% of the threshold.
How to calculate this? From 220 you need to subtract your own age - this is the maximum heart rate. Then we calculate the percentages. For example, for a 60-year-old person, the threshold load is calculated as follows: 220–60 = 160 heart beats per minute, and 70% will be 112. This figure should be a guideline. But, if unpleasant sensations appear at this frequency, the load needs to be reduced.
Attention!
After a heart attack, lifting heavy objects is strictly contraindicated.
Typical course
To be able to avoid the most severe complications of a heart attack, it is advisable to know and remember the classic symptoms of the development of this pathology.
These symptoms usually include:
- sudden development of acute chest pain, with a burning, often pressing or squeezing character;
- irradiation of pain to the pericardial region (irradiation to the left side of the chest, left arm or under the left shoulder blade);
- situations when the described pain is accompanied by a panic attack, acute fear of death.
It is important to remember that the slightest suspicion of the development of myocardial infarction should force the patient to urgently consult a doctor to receive specialized treatment aimed at opening a narrowed, closed (stenotic) vessel to prevent the development of extensive necrosis of the heart muscles.
Although a heart attack is always an unexpected heart attack, it is not difficult to recognize. Its symptoms cannot be confused with any other disease. Do not forget that a heart attack is life-threatening. Timely help can save a person, but its absence will lead to death. An ambulance must be called as quickly as possible.
Clinical picture of atypical cases
Unfortunately, sometimes a heart attack develops in a non-standard way, complicating its diagnosis and early detection.
For example, some patients may experience the following hidden symptoms of narrowing of the coronary arteries:
- sensations of pain in the lower jaw, left arm or even leg, left side;
- the occurrence of pain in the epigastric region, with the addition of nausea, bloating, vomiting;
- some patients may simply not have enough air, in the absence of other symptoms.
Somewhat less frequently, during the attacks in question, symptoms similar to manifestations of completely different ailments may occur:
- an attack of the asthmatic type with the development of bronchospasm, pulmonary edema, severe shortness of breath, etc.;
- an attack similar to an exacerbation of pancreatitis - with the occurrence of nausea, profuse vomiting, general weakness, and abdominal pain;
- an attack of a neurological type, with the development of neurosis, a panic attack, with disorders of consciousness, vision, with the appearance of dizziness, headaches.
The described clinical picture should also force the patient to urgently call an ambulance - independent treatment in such cases is prohibited!
First aid
In order to promptly independently determine the possible development of the pathology in question, it is very important to pay attention to:
- intensity and nature of pain. a heart attack is characterized by squeezing, pressing, burning sensations;
- localization of pain. location of pain in the left side of the body, just behind the sternum, in the area of the shoulders, shoulder blades;
- irradiation of pain to the arm, side, neck.
But in order to really help a patient with an angina attack, the first thing that is very important to do is, of course, to call a medical team. The sooner doctors have the opportunity to begin their work, the greater the patient’s chances of surviving and avoiding the sad complications of the primary problem.
The first pre-medical treatment or simply assistance to the patient should be as follows:
- It is important for the patient to take a comfortable body position; he can be laid down or seated comfortably, allowed to lean back on the pillow;
- unbutton tight clothes;
- provide air flow, open windows;
- You can give the patient one tablet of nitroglycerin or aspirin.
Further actions should be carried out by the resuscitation team. Unfortunately, it is extremely difficult to teach people without medical education to perform chest compressions and artificial respiration, which may also be urgently needed by patients in such situations.
Prevention of heart attack in men and women: eating habits
A properly adjusted diet will help prevent the development of a heart attack. The following recommendations will help strengthen the heart and blood vessels in old age:
- Include fresh vegetables, fruits, and healthy root vegetables in your diet.
- Eat more poultry, veal, fish and seafood.
- Eat fresh, raw fruits more often.
- Reduce the level of fat and salt in your food.
- Increase your intake of foods rich in magnesium, potassium and calcium.
This diet will help lower cholesterol levels, while you will get the necessary vitamins and minerals. To develop an individual nutrition plan, you should consult your doctor.
Diagnostics
After the ambulance arrives, the patient, as a rule, undergoes an urgent electrocardiogram, according to the readings of which the development of a heart attack can be determined. At the same time, doctors collect anamnesis, analyzing the time of onset of the attack, its duration, pain intensity, its localization, irradiation, etc.
The following changes can be considered electrocardiographic criteria for the development of an attack:
- damage or arched growth of the st segment, which can merge with a positive t wave or even turn into a negative t wave;
- the appearance of a pathologically altered q wave with a decrease in the amplitude of the r wave. sometimes there may be a complete disappearance of the r wave with the formation of qs;
- the appearance of a negative, often symmetrically located T wave.
In addition, acutely occurring bundle branch block may be indirect signs of the development of a heart attack. Also, the diagnosis of myocardial infarction is based on the detection of markers of damage to the muscle tissue of the heart.
Today, the most convincing (obvious) marker of this type can be considered the troponin level in the blood, which will be significantly increased when the described pathology occurs.
Troponin levels may rise sharply in the first five hours after a heart attack and may remain elevated for up to twelve days. In addition, to detect the pathology in question, doctors can prescribe echocardiography.
Modern approaches to the treatment of acute myocardial infarction
Today, myocardial infarction (MI) remains as serious a disease as it was several decades ago.
Here is just one example that proves the severity of this disease: about 50% of patients die before they have time to meet with a doctor.
At the same time, it is clear that the risk of MI for life and health has become significantly lower. After the basic principles of intensive care wards for coronary patients were developed 35 years ago and these wards began to actually work in healthcare practice, the effectiveness of treatment and prevention of cardiac arrhythmias and conduction disorders in patients with myocardial infarction significantly increased and hospital mortality decreased. In the 70s, it was more than 20%, but in the last 15 years, after the role of thrombosis in the pathogenesis of acute MI was proven and the beneficial effect of thrombolytic therapy was shown, in a number of clinics the mortality rate has decreased by 2 times or more.
It must be said that the basic principles and recommendations for the treatment of acute MI, however, as for most other serious pathologies, are based not only on the experience and knowledge of individual clinics, areas, schools, but also on the results of large multicenter studies, sometimes carried out simultaneously in many hundreds of hospitals around the world. Of course, this allows the doctor to quickly find the right solution in standard clinical situations.
The main objectives of treatment of acute MI can be called the following: relief of a painful attack, limiting the size of the primary focus of myocardial damage and, finally, prevention and treatment of complications. A typical anginal attack, which develops in the vast majority of patients with MI, is associated with myocardial ischemia and continues until necrosis occurs of those cardiomyocytes that should die.
One of the proofs of precisely this origin of pain is its rapid disappearance when coronary blood flow is restored (for example, against the background of thrombolytic therapy).
Relieving a pain attack
Pain itself, acting on the sympathetic nervous system, can significantly increase heart rate, blood pressure (BP), and heart function. It is these factors that determine the need to stop a painful attack as quickly as possible. It is advisable to give the patient nitroglycerin under the tongue.
This may relieve pain if the patient has not previously received nitroglycerin for this attack. Nitroglycerin can be in tablet or aerosol form. There is no need to resort to its use if systolic blood pressure is below 90 mm Hg.
Morphine is used all over the world to relieve pain.
which is administered intravenously in fractional doses from 2 to 5 mg every 5–30 minutes as needed until complete (if possible) pain relief.
The maximum dose is 2–3 mg per 1 kg of patient body weight. Intramuscular administration of morphine should be avoided, since the result in this case is unpredictable.
Side effects are extremely rare (mainly hypotension, bradycardia) and are quite easily controlled by elevating the legs, administering atropine, and sometimes plasma replacement fluid.
In elderly people, depression of the respiratory center is uncommon, so morphine should be administered in a reduced (even half) dose and with caution. The antagonist of morphine is naloxone
, which is also administered intravenously, it relieves all side effects, including respiratory depression caused by opiates.
The use of other narcotic analgesics, for example promedol and other drugs of this series, is not excluded. The suggestion that neuroleptanalgesia (a combination of fentanyl and droperidol) has a number of benefits has not been clinically confirmed. Attempts to replace morphine with a combination of non-narcotic analgesics and antipsychotics in this situation are unjustified. Thrombolytic therapy
The main pathogenetic method of treating MI is to restore the patency of the occluded coronary artery. Most often, to achieve this, either thrombolytic therapy or mechanical destruction of the thrombus is used during transluminal coronary angioplasty. For most clinics in our country, the most realistic option today is to use the first method.
The process of necrosis develops extremely quickly in humans and generally ends, as a rule, within 6–12 hours from the onset of an anginal attack, therefore, the faster and more fully it is possible to restore blood flow through the thrombosed artery, the more preserved will be the functional ability of the left ventricular myocardium and ultimately resulting in less mortality. It is considered optimal to start administering thrombolytic drugs 2–4 hours after the onset of the disease.
The success of treatment will be greater if it is possible to reduce the period of time before the start of thrombolytic therapy, which can be done in two ways: the first is early detection and hospitalization of patients in the hospital and rapid decision-making on appropriate treatment, the second is the start of therapy at the prehospital stage.
Our studies have shown that starting thrombolytic therapy at the prehospital stage allows for a gain in time, on average about 2.5 hours.
This method of thrombolytic therapy, if carried out by doctors of a specialized cardiac care team, is relatively safe.
In the absence of contraindications, thrombolytic therapy is advisable for all patients in the first 12 hours of illness. The effectiveness of thrombolytic therapy is higher (42–47% reduction in mortality) if it is started within 1 hour of illness. For periods longer than 12 hours, the use of thrombolytic drugs is problematic and should be decided taking into account the real clinical situation.
Thrombolytic therapy is especially indicated for elderly people, patients with anterior MI, and also in cases where it is started early enough.
A prerequisite for starting thrombolytic therapy is the presence of ST segment elevations on the ECG or signs of bundle branch block.
Thrombolytic therapy is not indicated if
ST
, regardless of how the final phase
of the QRS
on the ECG looks - depressed, negative
T-waves
, or the absence of any changes.
Early initiation of thrombolytic therapy can save up to 30 patients out of 1000 treated.
Today, the main route of administration of thrombolytic drugs is intravenous. All drugs used, first generation thrombolytics
, such as streptokinase (1,500,000 units for 1 hour) - urokinase (3,000,000 units for 1 hour),
second generation
- tissue plasminogen activator (100 mg bolus plus infusion), prourokinase (80 mg bolus plus infusion 1 hour ) – are highly effective thrombolytics.
The risk of thrombolytic therapy is well known - this is the occurrence of bleeding, the most dangerous being cerebral hemorrhage.
The frequency of hemorrhagic complications is low, for example, the number of strokes when using streptokinase does not exceed 0.5%, and when using tissue plasminogen activator - 0.7–0.8%.
As a rule, in case of serious hemorrhages, fresh frozen plasma is administered
and, of course, the administration of the thrombolytic is stopped.
Streptokinase can cause allergic reactions
, which, as a rule, can be prevented by prophylactic administration of corticosteroids - prednisolone or hydrocortisone.
Another complication is hypotension
, which is more often observed when using drugs based on streptokinase; it is often accompanied by bradycardia.
Usually this complication can be stopped after stopping the thrombolytic infusion and administering atropine and adrenaline; sometimes the use of plasma expanders and inotropes is required. Today, suspected aortic dissection, active bleeding, and previous hemorrhagic stroke are considered absolute contraindications to thrombolytic therapy.
On average, only one third of patients with MI receive thrombolytic drugs, and in our country this figure is significantly lower.
Thrombolytics are not administered mainly due to the late admission of patients, the presence of contraindications, or the uncertainty of changes on the ECG. Mortality among patients not receiving thrombolytics remains high and ranges from 15 to 30%. β-blockers
On the 1st day after MI, sympathetic activity increases, therefore the use of β-blockers
, which reduce oxygen consumption by the myocardium, reduce heart function and ventricular wall tension, became the rationale for their use in this category of patients.
A number of large multicenter studies that examined the effectiveness of intravenous b-blockers on the 1st day of MI showed that they reduce mortality in the 1st week by approximately 13–15%. The effect is somewhat higher if treatment begins in the first hours of the disease, and is absent if these drugs are used from the 2-3rd day of the disease. b-blockers also reduce the number of recurrent heart attacks by an average of 15–18%. The mechanism by which b-blockers influence mortality is a reduction in the incidence of ventricular fibrillation and cardiac rupture.
Treatment with b-blockers begins with intravenous administration (metoprolol, atenolol, propranolol) - 2-3 times or as long as necessary to optimally reduce the heart rate. Subsequently, they switch to taking drugs orally: metoprolol 50 mg every 6 hours in the first 2 days, atenolol 50 mg every 12 hours during the day, and then select the dose individually for each patient. The main indications for the use of b-blockers are signs of sympathetic hyperactivity, such as tachycardia in the absence of signs of heart failure, hypertension, pain, and the presence of myocardial ischemia.
b-Blockers, despite the presence of contraindications to their use, for example, bradycardia (heart rate less than 50 per minute), hypotension (systolic blood pressure below 100 mm Hg), the presence of heart block and pulmonary edema, as well as bronchospasm, are used nevertheless, in the overwhelming majority of patients with MI.
However, the ability of drugs to reduce mortality does not extend to the group of b-blockers with their own sympathomimetic activity. If the patient has begun treatment with b-blockers, the drug should be continued until serious contraindications appear. Use of antiplatelet agents and anticoagulants
antiplatelet in acute MI
, in particular
acetylsalicylic acid
, helps reduce thrombosis, and the maximum effect of the drug is achieved quite quickly after taking an initial dose of 300 mg and is stably maintained with daily intake of acetylsalicylic acid in small doses - from 100 to 250 mg / day.
In studies conducted on many thousands of patients, it was found that the use of acetylsalicylic acid reduces 35-day mortality by 23%. Acetylsalicylic acid is contraindicated in case of exacerbation of peptic ulcer disease, with its intolerance, as well as with bronchial asthma provoked by this drug.
Long-term use of the drug significantly reduces the frequency of recurrent heart attacks - up to 25%, so taking acetylsalicylic acid is recommended for an indefinite period.
Another group of drugs that affect platelets are platelet glycoprotein IIB/IIIA blockers. Currently, the effectiveness of the use of two representatives of this class is known and proven - abciximab
and
tiropheban
.
According to the mechanism of action, these drugs compare favorably with acetylsalicylic acid, since they block most of the known pathways of platelet activation. The drugs prevent the formation of a primary platelet thrombus, and their effect is sometimes quite long - up to six months. Worldwide experience is still limited; in our country, work with these drugs is just beginning. heparin
is still widely used , which is mainly prescribed for the prevention of recurrent heart attacks, to prevent thrombosis and thromboembolism. Schemes and doses of its administration are well known. The dose is selected so that the partial thromboplastin time increases by 2 times compared to the norm. The average dose is 1000 IU/hour for 2–3 days; subcutaneous administration of heparin is recommended when patients are slowly mobilized.
Currently there is evidence on the use of low molecular weight heparins
, in particular
enoxyparin
and
fragmin.
Their main advantages are that they actually do not require laboratory monitoring of blood clotting parameters and special equipment, such as infusion pumps, for their administration, and most importantly, they are significantly more effective than unfractionated heparins.
The use of indirect anticoagulants has not lost its importance, especially in cases of venous thrombosis, severe heart failure, and the presence of a blood clot in the left ventricle. Calcium antagonists
Calcium are used as standard therapy for MI
at present, they are actually not used, since they do not have a beneficial effect on the prognosis, and their use from a scientific point of view is unfounded.
Nitrates
Intravenous administration of nitrates during MI in the first 12 hours of the disease reduces the size of the necrosis focus and affects the main complications of MI, including deaths and the incidence of cardiogenic shock.
Their use reduces mortality to 30% in the first 7 days of illness, this is most obvious in anterior localization of infarctions.
Taking nitrates orally starting from the 1st day of the disease does not lead to either an improvement or a worsening of the prognosis by the 30th day of the disease. Intravenous nitrates should be standard therapy for all patients admitted in the early hours of illness with anterior MI and systolic blood pressure greater than 100 mm Hg. Introduce nitroglycerin at a low rate, for example 5 mcg/min, and gradually increase it, achieving a decrease in systolic pressure by 15 mmHg. In patients with arterial hypertension, blood pressure can be reduced to 130–140 mmHg. As a rule, nitrate therapy is carried out within 24 hours unless there is a need to continue this therapy, in particular if pain associated with myocardial ischemia persists or signs of heart failure. ACE inhibitors
angiotensin-converting enzyme
inhibitors have firmly taken their place in the treatment of patients with MI .
This is primarily determined by the fact that these drugs are able to stop the expansion, dilatation of the left ventricle, and thinning of the myocardium, i.e.
influence the processes leading to remodeling of the left ventricular myocardium and accompanied by a serious deterioration in myocardial contractile function and prognosis. As a rule, treatment with ACE inhibitors begins 24–48 hours after the onset of myocardial infarction to reduce the likelihood of arterial hypertension.
Depending on the initially impaired left ventricular function, therapy can last from several months to many years. It was found that treatment with captopril
at a dose of 150 mg/day in patients without clinical signs of circulatory failure, but with an ejection fraction below 40%, significantly improved the prognosis.
In the treated group, mortality was 19% lower, and there were 22% fewer cases of heart failure requiring hospital treatment. Thus, ACEs (captopril 150 mg/day, ramipril 10 mg/day, lisinopril 10 mg/day, etc.)
are advisable to prescribe to most patients with MI, regardless of its location and the presence or absence of heart failure.
However, this therapy is more effective when clinical signs of heart failure and instrumental studies (low ejection fraction) are combined.
In this case, the risk of death is reduced by 27%, i.e. this prevents deaths in every 40 out of 1000 patients treated during the year.
Already during the patient’s stay in the hospital, it is advisable to study his lipid spectrum in detail.
Acute MI itself somewhat reduces the content of free cholesterol in the blood.
If there is data on significant changes in this indicator, for example, when the level of total cholesterol is above 5.5 mmol/l, it is advisable to recommend the patient not only a lipid-lowering diet, but also taking medications, primarily statins.
Thus, currently the doctor has a significant arsenal of tools to help a patient with MI and minimize the risk of complications.
Of course, the main way to achieve this goal is the use of thrombolytic drugs, but at the same time, the use of b-blockers, aspirin, ACE and nitrates can significantly affect the prognosis and outcome of the disease. Enalapril: Ednit
(Gedeon Richter)
Enap
(KRKA)
| Applications to the article |
| The main objectives of the treatment of acute myocardial infarction: 1) relief of a painful attack 2) limiting the size of the primary myocardial lesion 3) prevention and treatment of complications |
| In the absence of contraindications, thrombolytic therapy is advisable for all patients in the first 12 hours of illness. |
| Intravenous nitrates should be therapy for all patients with anterior myocardial infarction and systolic blood pressure greater than 100 mm Hg. |
| TREATMENT SCHEME FOR ACUTE MYOCARDIAL INFARCTION |