Sodium (Na) is the major extracellular electrolyte responsible for plasma osmotic pressure. It determines the amount of almost all body fluids (circulating and deposited blood, cerebrospinal fluid, fluids of the serous cavities, etc.), and is part of the bicarbonate and phosphate buffers (regulation of ASR). Na is necessary for the transmission of nerve impulses between neurons and neuromuscular synapses. All of the above causes the development of severe disorders when the electrolyte balance is disturbed. There are no exact statistics on the prevalence of hypernatremia.
Causes of hypernatremia
This condition quite often has a multifactorial origin. Conditionally, a physiological cause (not related to any disease) can be considered intense physical activity and dietary disorders - oversalting of food, insufficient consumption of drinking water or prolonged intake of mineral water. Pathological causes of hypernatremia are:
- Fluid deficiency.
Water loss can occur through the skin (sweating), the gastrointestinal tract (nausea, vomiting), and in the urine (diabetes mellitus or diabetes insipidus, polyuric stage of acute renal failure, glomerulonephritis). Failure to drink adequate amounts of water (for example, while comatose) can also cause hypernatremia. - Excess sodium intake.
More often it is provoked by the uncontrolled administration of hypertonic solutions of NaCl, bicarbonates or other solutions containing Na. Hypernatremia is caused by drinking sea water and using dialysis fluids containing high concentrations of Na. - Reduced sodium excretion.
Sodium retention in the body occurs due to increased secretion of renin in the juxtaglomerular apparatus of the kidneys or mineralocorticoids in the adrenal glands (primary and secondary hyperaldosteronism). The causes are congestive heart failure, liver and kidney diseases, and Conn's syndrome. - Taking medications.
Hypernatremia is often potentiated by diuretics, especially those that increase blood osmotic pressure (mannitol). Hypernatremia also develops during treatment with drugs that block the effect of antidiuretic hormone on the kidneys (vaptans, demeclocycline).
ADDITIONAL INFORMATION.
Source of financing. The work was carried out within the framework of funding under the state assignment of the Ministry of Health of Russia AAAA-A17-117012610108-6 “Hormonal regulation of water-electrolyte metabolism disorders in dysnatremia syndromes, personalization of prognosis, new technologies for differential diagnosis, targeted treatment” (2017-2019).
Conflict of interest. The authors declare that there are no obvious or potential conflicts of interest related to the research conducted and the publication of this article.
Authors' participation. All authors made significant contributions to the preparation of the article and read and approved the final version before publication.
Pathogenesis
An increase in plasma sodium leads to an increase in plasma osmolarity. Due to changes in the osmotic concentration gradient, fluid moves from the cells into the extracellular space (bloodstream and interstitium). Due to dehydration, cells shrink and are destroyed. Against the background of a violation of the relationship between the intra- and extracellular content of Na ions, a change in the membrane potential occurs in the direction of lowering the excitability threshold.
These mechanisms underlie the occurrence of neuropsychiatric and neuromuscular symptoms. Sodium is a sympathetic cation, that is, it increases the sensitivity of cells to catecholamines and other vasopressor mediators. Therefore, its accumulation in vascular smooth muscle cells causes an increase in vascular tone and an increase in blood pressure.
Classification
Conventionally, hypernatremia is divided into moderate and severe, focusing on clinical symptoms, since there are no clear numerical indicators for dividing this condition by degree. Depending on the volume of circulating blood, the following types of hypernatremia are distinguished:
- Hypovolemic.
Develops with water deficiency and large losses of Na. Occurs with kidney disease, diabetes and taking osmotic diuretics. - Isovolemic.
Characterized by fluid loss without Na deficiency. Occurs with diabetes insipidus. - Hypervolemic.
Caused by excess Na and water. The main cause of this form is considered to be the administration of large volumes of hypertonic solution or bicarbonate.
According to the rate of development, hypernatremia can be:
- Acute –
lasting up to 48 hours. - Chronic –
lasting more than 48 hours.
Symptoms of hypernatremia
The clinical picture directly depends on the rate of increase in sodium concentration. With slowly developing hypernatremia, due to the inclusion of compensatory mechanisms (stimulation of the secretion of vasopressin and natriuretic peptides), an absolutely asymptomatic course can be observed. The most characteristic sign of rapidly onset hypernatremia is thirst.
Other early symptoms include decreased appetite, nausea and vomiting. The central nervous system is particularly affected. Excessive irritability, increased tendon reflexes, and impaired sense of balance occur. Confusion and panic attacks are possible. Characterized by muscle rigidity, myoclonic twitching, painful spasms.
Due to high blood pressure, a patient with hypernatremia experiences heaviness in the back of the head and possible throbbing pain. In case of significant fluid loss (hypovolemic form), blood pressure decreases, which causes dizziness, darkening of the eyes, and sometimes loss of consciousness. In the hypervolemic form, swelling of the lower extremities is often observed.
Complications
Hypernatremia has a very high incidence of adverse effects, including fatal ones. These include cerebral edema, thrombosis of cranial vessels, coma. Complications are also possible due to improper treatment, since with chronic hypernatremia, organic osmotically active substances (osmolytes) begin to accumulate in neurons as a compensatory mechanism.
When hypotonic solutions are administered too quickly, osmolytes do not have time to leave the neurons, as a result, water rushes into the cells and brain edema develops. Sometimes, with a long course, electrolyte-steroid cardiomyopathy with necrosis is observed. Arterial hypertension increases the risk of complications such as myocardial infarction and stroke. Isolated cases of rhabdomyolysis followed by acute renal failure in patients with hypernatremia have been described.
Diagnostics
Patients with this condition are supervised by resuscitators together with specialized specialists (endocrinologist). During examination, pay attention to hyperreflexia, muscle tone, and clarity of consciousness. It is important to determine the type of hypernatremia, since the course of different types of pathology is different. They focus on symptoms such as signs of dehydration (dry skin and mucous membranes, decreased turgor) or peripheral edema and pressure indicators.
Before obtaining laboratory results, differentiation of hypernatremia is carried out primarily from hyponatremia due to very similar clinical symptoms. To confirm the diagnosis and establish the cause of the condition, the following techniques are used:
- Laboratory research.
Serum sodium concentration and osmolarity are measured. In a biochemical blood test, the levels of glucose, urea, creatinine and liver transaminases (ALT, AST) are assessed. If primary hyperaldosteronism is suspected, the renin-aldosterone ratio is examined. The specific gravity, osmolarity of urine, the content of sodium, protein and glucose in it are studied. - Instrumental research.
Determining the volume of the vascular bed by measuring central venous pressure in the subclavian veins provides invaluable assistance in clarifying the type of hypernatremia. To diagnose diseases that could cause the pathology, an abdominal CT scan and echocardiography are performed.
RESULTS
How often should you order a blood test for sodium?
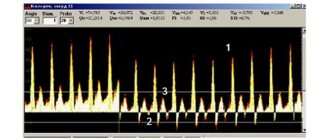
Among 353 specialists who took part in an online survey on hypo- and hypernatremia in clinical practice, there was a wide variation in responses regarding the frequency of ordering determination of sodium concentration when prescribing a biochemical blood test (Fig. 1). At the same time, the curve of the dependence of the number of specialists’ answers on the frequency of sodium in the blood was U-shaped, with an almost equal probability of opposite answers. Only 38.2% of respondents responded that they actively prescribe sodium determination in more than half of the cases.
Figure 1. Histogram of the distribution of specialists’ answers to the question about prescribing a biochemical blood test for sodium (n=353)
Almost half of the surveyed specialists (47%) prescribe determination of the level of sodium in the blood only if the patient has a disease with a possible disorder, and 33.1% - only if sodium is included in a standard biochemical blood test. Only a third of respondents (31.2%) always prescribe a test for sodium levels in the blood, while 11.9% of respondents never prescribe it (Fig. 2).
Figure 2. Results of a survey of specialists regarding the determination of sodium levels in a biochemical blood test (n=353)
Spearman correlation analysis among endocrinologists shows that the frequency of sodium prescription is related to the number of patients treated in the hospital (R=0.36, p<0.0000001) or outpatient (R=0.31, p<0.0000001) per month, which may reflect, incl. clinical experience of a doctor.
When detailing the clinical situations associated with dysnatremia, in which doctors prescribe a determination of sodium in the blood, the data shown in Figure 3 was obtained. In more than 50% of cases with adrenal insufficiency, diabetes insipidus, edema syndrome, renal failure, arterial hypertension, taking diuretics, In cases of hypopituitarism, diabetes mellitus and heart failure, doctors prescribe determination of blood sodium levels.
Figure 3. Frequency (%) of prescription for determining the level of sodium in the blood under various conditions pathogenetically associated with the development of hyponatremia (n=353)
Features of laboratory determination of sodium
The detection of dysnatremia directly depends on the reference interval used, established by the laboratory. During the survey, specialists, according to the questionnaire, indicated the upper and lower limits of the reference interval of the laboratory they used. The obtained data are presented in Figure 4 and Table 2.
Figure 4. Representation of laboratory reference intervals indicated by respondents relative to generally accepted physiological blood sodium limits
Table 2. Values of the upper and lower limits of the reference interval, as well as their width of the range of normal values, obtained during the survey (n=353)
| Parameter | Meaning Me [Q1; Q3] min-max |
| Lower limit of the reference interval for sodium in blood serum, mmol/l | 135,0 [135;136] 110-141 |
| Upper limit of the reference interval for sodium in blood serum, mmol/l | 145,0 [145;150] 124-169 |
| Width of the normal range of reference intervals used by the laboratory for serum sodium levels, mmol/l | 10 [9;16] 4-40 |
Temporary availability of blood sodium determination
Sodium determination in an accelerated mode (with a result in less than 15 minutes) is available within 24 hours from 6-7% of surveyed endocrinologists, which possibly reflects the presence of an acid-base composition (ALB) and electrolyte analyzer in the department working on whole blood (Fig. 5).
Figure 5. Availability and speed of determining blood sodium levels at different time intervals (n=353)
The time period for obtaining an analysis result of 15-60 minutes reflects the time for standard sample preparation (centrifugation) and conducting research on an automatic analyzer. With this speed, the majority of doctors surveyed (91%) can obtain the result, but only during daytime working hours from 9:00 to 17:00; in the evening and at night, the possibility of performing the analysis decreases to 53-58%.
Identification and correction of dysnatremia by endocrinologists
In 81.6% of cases, endocrinologists surveyed (n=288) encountered patients with changes in sodium levels in the blood. During the year, on average, physicians encountered 12 cases of hypernatremia (Me [Q1; Q3]; 2 [0, 5]) and 7 cases of hyponatremia (Me [Q1; Q3]; 2 [0, 5]).
It was noted that the lower and upper limits of the reference interval of the laboratory used are not significantly associated with the identification of hypo- or hypernatremia by doctors. Spearman correlation analysis did not show a significant dependence of the number of identified patients with dysnatremia on the lower limit of the reference interval for sodium level in the blood (R= -0.14, p=0.03) and the upper limit of the reference interval (R= -0.10, p=0.12).
In 36% of cases, the cause of hyponatremia was not determined. Most often, doctors encountered hyponatremia due to adrenal insufficiency (25.4%), taking diuretics (9%) and due to the syndrome of inappropriate secretion of antidiuretic hormone (6.1%), less often with central diabetes insipidus, brain diseases and decompensation of diabetes mellitus (3.5% each) (Fig. 6).
Figure 6. Causes of hyponatremia according to endocrinologists (n=288)
About 31% of endocrinologists encountered pseudohyponatremia due to disorders of lipid, protein or carbohydrate metabolism, and 54.2% encountered hyponatremia caused by drugs.
Endocrinologists named the main causes of drug-induced hyponatremia:
- 84.1% - diuretics;
- 38.6% - antihypertensive drugs;
- 31.8% - desmopressin;
- 13.7% - chemotherapy drugs;
- 9% - antipsychotics;
- 5.2% - antidepressants;
- 1.2% - inhibitors of sodium-glucose cotransporter type 2 (SGLT2 inhibitors);
- 0.4% each included drugs - non-steroidal anti-inflammatory drugs, glucocorticoids, intravenous saline.
Only 17 of 288 (6%) endocrinologists surveyed considered themselves experts or specialists competent in treating patients with dysnatremia. At the same time, 46.2% of endocrinologists manage patients independently when identifying dysnatremia (Fig. 7). 38% of endocrinologists have a hypertonic solution (3%) of sodium chloride in their medical institutions.
Figure 7. Options for the management of patients with dysnatremia according to a survey of endocrinologists (n=288) (Section other includes responses to obtaining consultations from other general practitioners/cardiologists/nephrologists)
Treatment of hypernatremia
All patients with acute conditions are transferred to the intensive care unit. Patients with chronic hypernatremia can be treated in a general ward. The main condition for successful therapy is constant monitoring of water balance (taking into account the amount of fluid injected and excreted) and the concentration of blood electrolytes. Treatment includes the following main areas:
- Replenishment of fluid deficiency.
In the hypovolemic form of hypernatremia, it is necessary to restore the proper level of free water in the body. Conscious patients are given oral hydration. For vomiting, mental disorders, and coma, intravenous administration of a hypotonic NaCl solution (0.5%) is used, which also reduces the concentration of sodium in the blood. - Active decrease in plasma Na .
To enhance sodium excretion, loop diuretics (furosemide) are indicated. Additionally, a 5% solution of dextrose or glucose with insulin is used. The sodium level is reduced gradually (in the acute form - no more than 1 mmol/hour, in the chronic form - no more than 8 mmol/day), since a high rate of correction is associated with the risk of cerebral edema. - Treatment of the underlying disease.
Particular attention is paid to hypernatremia that has developed against the background of diabetes insipidus (central, nephrogenic or drug-induced), since if there is a deficiency of antidiuretic hormone without replacement therapy, treatment will be ineffective. Synthetic analogues of ADH (desmopressin) are recommended.
DISCUSSION
Hypo- and hypernatremia syndromes are characterized by a high frequency of up to 57 and 63%, respectively, by the presence of a pathogenetic connection with various diseases, which is mostly mediated through hormonal influences [5]. Dysnatremic conditions are associated with a multiple increase in mortality, severe imbalances, and the risk of fractures [6]. At the same time, the clinical manifestations of dysnatremia are nonspecific, reflect an osmotically mediated decrease in brain function, and therefore can often be missed in clinical practice. Thus, the determination of blood sodium, rather than clinical symptoms, is of paramount importance in the diagnosis of dysnatremia [6].
The survey data showed that there are several negative factors in the diagnosis of dysnatremic conditions. First of all, this is a relatively low frequency of determination of this electrolyte in the blood (Fig. 2), which is also due to doctors’ failure to recognize conditions potentially associated with a high risk of developing hypo- or hypernatremia (Fig. 3). A large number of endocrine diseases are associated with a predisposition to the development of hypo- or hypernatremia syndromes, but determination of blood sodium levels is prescribed quite rarely, which may also predispose to a decrease in the detection of cases of dysnatremia and have an unfavorable clinical significance. Less than half of the doctors (48%) who took part in the survey prescribe sodium levels when examining patients in the intensive care unit, although the severity of the condition, massive infusion therapy, artificial ventilation, the use of a large number of medications, etc. are predisposing factors to the development of dysnatremic conditions [14, 15].
The second factor is that the survey data revealed significant fluctuations for the lower and upper limits of the reference interval for sodium in the blood serum, relative to the generally accepted physiological norm [16, 17], with variability from -18.5% to +4.4% for the lower boundaries of the reference interval and from -15.2% to +16.6% for its upper limit. The width of the ranges of normal values was also completely different for the reference interval used by the laboratory for the concentration of sodium level in the blood serum - from 4 to 40 mmol/l, which also indicates the variability of the width of the reference intervals, which may not be acceptable for such a homeostatic indicator as the level blood sodium.
Discrepancy between the lower limit of normal 135-136 mmol/l was observed in 22% (62/278), discrepancy with the upper limit of normal 145-146 mmol/l - in 47% (131/278) of laboratories, and in 33% (41/278) laboratories used by doctors showed discrepancies at both ends of the reference interval. Thus, in 55% of laboratories, the boundaries of the reference interval, even if it is permissible to expand it by 1 mmol/l in each direction, do not correspond to physiology and can be a source of over- or underdiagnosis of dysnatremic conditions.
The third factor is the availability of determination of blood sodium, which seems to be a very important aspect in the timely diagnosis of its deviations, as well as correction of the therapy. Modern clinical guidelines for the treatment of hyponatremia suggest monitoring blood sodium every 2-3 hours to ensure the safety of the rate of correction [6, 15]. The survey data demonstrated good accessibility of the study, incl. 24 hours a day. Of course, 24-hour monitoring of sodium levels is not important for all diseases, but given the high incidence of dysnatremia, in the absence of specific clinical symptoms and potentially serious consequences, the ability to determine blood sodium with a result within an hour is extremely important.
The survey, limited to endocrinologists, revealed that the vast majority of endocrinologists (82%) in their clinical practice encounter patients with abnormal blood sodium levels, but only 6% have the competence to manage patients with dysnatremia, which undoubtedly raises questions about inclusion in educational programs at all levels of medical education modules on the basics of water-electrolyte metabolism and its correction.
One of the important methods of treating symptomatic hyponatremia is the administration of hypertonic (3%) sodium chloride solution [6, 15]. Due to the fact that this solution is not usually used parenterally outside of hyponatremic conditions, and its external use for the treatment of purulent wounds has been replaced by more specialized drugs, its availability in clinics has recently decreased sharply. The survey showed that the drug was available in only 38% of clinics, which is undoubtedly a low figure.
Prognosis and prevention
Hypernatremia is a severe electrolyte disorder with a poor prognosis. Death occurs in 50% of cases in the acute form and in 10-15% in the chronic form. In children, the mortality rate is much higher - about 65-70%. Approximately 2/3 of surviving patients have residual effects in the form of neurological deficit to varying degrees.
Prevention consists of proper treatment of diseases against which hypernatremia may develop (diabetes mellitus, diabetes insipidus, aldosteroma). The occurrence of this disorder in patients receiving hypotonic solutions or osmotic diuretics can be prevented by regular monitoring of sodium levels.
METHODS
Study design
A single-stage sociological uncontrolled study was conducted on the basis of the Federal State Budgetary Institution "National Medical Research Center of Endocrinology" of the Russian Ministry of Health. The study was conducted in the form of a survey of doctors on the issues of hypo- and hypernatremia using the online questionnaire “Questionnaire on hypo- and hypernatremia in clinical practice” created on the Google forms platform. An invitation to fill out the questionnaire was sent to addresses included in the database of the Russian Association of Endocrinologists (n=9325). A total of 353 completed questionnaires were received. Experts from 64 regions of Russia took part in the survey. The characteristics of the respondents are shown in Table 1.
Table 1. Characteristics of respondents who took part in the survey (n=353)
| Characteristic | Index, % |
| Gender (n= 353): | |
| male | 13% |
| female | 87% |
| Age (n= 353): | |
| up to 25 years | 1,7% |
| 25-30 years | 17,8% |
| 31-35 years old | 17,6% |
| 36-40 years old | 17,8% |
| 41-45 years old | 16,4% |
| 46-50 years | 12,7% |
| 51-56 years old | 7,1% |
| 56-60 years | 5,4% |
| over 60 years old | 3,4% |
| Specialty (n= 353): | |
| endocrinology | 81,6% |
| therapy | 4,5% |
| nephrology | 4,0% |
| pediatric endocrinology | 2,5% |
| obstetrics-gynecology | 2,0% |
| surgery | 1,2% |
| neurosurgery | 0,9% |
| cardiology | 0,6% |
| anesthesiology-resuscitation | 0,6% |
| pediatrics | 0,6% |
| gastroenterology | 0,3% |
| Ultrasound | 0,3% |
| neurology | 0,3% |
| general practice | 0,3% |
| rheumatology | 0,3% |
| Work experience (n= 353): | |
| less than 5 years | 19,8% |
| 5-9 years | 19% |
| 10-19 years | 34,8% |
| 20-29 years old | 18,1% |
| more than 30 years | 8,2% |
| The main place of work is (n= 353): | |
| in the city | 97,5% |
| in the village | 1,4% |
| in a village | 1,1% |
| Management of patients in hospital (n= 353): | |
| Yes | 44,2% |
| No | 58,8% |
| Number of hours per month devoted to the management of inpatients , hours per month (n=152) | 104 [30;160] |
| Carrying out outpatient appointments with patients: | |
| Yes | 85% |
| No | 15% |
| Number of hours per month devoted to the management of outpatients , hours per month (n=288) | 172 [30;138] |
Eligibility Criteria
The study included all data from completed questionnaires. The questionnaire was loaded into the general table only after the respondent filled out all required fields.
Duration of the study
The study was conducted in August-September 2021.
Ethical review
The study was approved by the Local Ethics Committee of the Federal State Budgetary Institution “National Medical Research Center of Endocrinology” of the Ministry of Health of Russia (protocol No. 11 of October 23, 2013).
Statistical analysis
Principles for sample size calculation : The sample size was not pre-calculated.
Methods of statistical data analysis : Statistical processing of the obtained data was carried out using the application package Statistica for Windows v.10 (StatSoft inc., USA).
Distributions of quantitative characteristics are given in the form of medians and quartiles (1st and 3rd quartiles) – Ме [Q1; Q3], in some cases the minimum and maximum values of the indicator and percentage are also indicated. Correlation analysis was carried out using the Spearman method. The critical level of significance when testing statistical hypotheses was taken equal to 0.05.