Today, pharmaceutical companies have developed many antihypertensive drugs that help significantly improve the quality and life expectancy of hypertensive patients. Popular medications from the group of ACE inhibitors are drugs based on the active substance enalapril. Medicines are produced under various trade names, and have expensive and more affordable analogues. Among them, Enap and Enalapril have gained the greatest popularity among patients. Both drugs have similar pharmacological properties and practically do not differ in chemical composition. However, what is better than Enap or Enalapril in the fight against the manifestations of arterial hypertension?
Comparison of the effectiveness of Enap and Enalapril
The effectiveness of Enap is quite similar to Enalapril - this means that the ability of the drug substance to provide the maximum possible effect is similar.
For example, if the therapeutic effect of Enap is more pronounced, then using Enalapril even in large doses will not achieve this effect.
Also, the speed of therapy - an indicator of the speed of therapeutic action - is approximately the same for Enap and Enalapril. And bioavailability, that is, the amount of a drug reaching its site of action in the body, is similar. The higher the bioavailability, the less it will be lost during absorption and use by the body.
Efficacy and tolerability of enalapril and indapamide in the correction of arterial hypertension
A
Hypertension (AH) is a non-infectious pandemic that determines the structure of disability and mortality due to cardiovascular diseases in a socially significant group of the population. The development of primary hypertension is determined by many interacting factors: from genetic predisposition to social environmental conditions. Hypertension, which begins as a functional disorder, in most cases, sequentially, through various pathophysiological mechanisms, leads to specific damage to target organs (central nervous system, heart, kidneys), transforming from a risk factor into a disease.
According to various authors, hypertension in 80% or more cases is combined with various types of metabolic disorders, which are included in world clinical practice under the term “metabolic syndrome”, including dyslipidemia, impaired carbohydrate metabolism and insulin resistance (IR), abdominal obesity [1,3, 5.15].
From the standpoint of the modern understanding of the mechanisms of formation of high blood pressure numbers, prescribed antihypertensive drugs should have the following properties:
1. Effectively reduce blood pressure (achieving the target blood pressure level);
2. Prevent (reduce) damage to target organs;
3. Do not cause metabolic disorders;
4. Be safe to use and have no side effects;
5. Have a prolonged hypotensive effect (reduce the frequency of administration) [9].
According to modern WHO recommendations (1999), at the first stage of treatment of hypertension, the use of diuretics, b-blockers and angiotensin-converting enzyme inhibitors is recommended
(ACE inhibitors) with metabolically neutral properties [4,9,10].
Thiazide and thiazide-like diuretics can be divided into two generations: the first generation - derivatives of benzothiadiazine (hydrochlorothiazide, etc.) and benzenesulfonamide (chlorthalidone, etc.); second generation - chlorobenzamide derivatives (indapamide, xipamide, etc.) containing a methylindoline group.
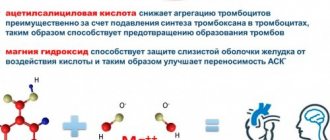
The hemodynamic effect of indapamide-like diuretics is due to their pharmacological action: inhibition of the reabsorption of Na+, Cl–, H+ and, to a lesser extent, K+ and Mg2+ in the proximal and distal tubules of the short segment of the nephron. At the same time, the discussed diuretics eliminate the excess content of Na+ ions in the vascular wall (due to their high lipophilicity), increase the synthesis of prostaglandins E2 and prostacyclin I2, inhibit the influx of Ca2+ ions into the smooth muscle cells of the vascular wall, which causes dilatation of blood vessels and reduces their sensitivity to pressor agents (catecholamines, thromboxanes). The total hemodynamic effect of indapamide is manifested as:
1. Vasodilation;
2. Decrease in total peripheral vascular resistance (TPVR);
3. Decrease in blood pressure;
4. Changes in the viscosity properties of blood due to inhibition of platelet aggregation activity.
The use of indapamide in a daily dose of 2.5 mg has a hypotensive effect without a significant effect on diuresis.
In its hypotensive activity, indapamide is 30 times superior to the action of spironolactones, 100 times superior to furosemide, and 300 times superior to chlorthalidone when used in comparable doses.
The therapeutic efficacy of indapamide diuretics has been demonstrated in a number of large randomized studies [6,11,14]. Their ability to prevent the development of coronary artery disease by reducing myocardial mass in hypertension has been noted. This property, atypical for other classes of diuretics, makes indapamide a unique drug with cardioprotective effects.
, the severity of which is not inferior to b-blockers and ACE inhibitors.
Particular attention is drawn to the fact that indapamide-like diuretics do not have a withdrawal syndrome and do not cause adverse metabolic disorders: they do not have a negative effect on glucose metabolism and the level of atherogenic blood lipids. In recent years, studies have shown that indapamide helps normalize glucose levels in type II diabetics, preventing diabetic nephropathy [10,15]. Indapamide, improving microcirculation in the kidney, eliminates microalbuminuria, which is a marker of generalized vascular damage and a predictor of cardiovascular complications. A similar pattern was noted when studying the metabolism of cholesterol (C) and triglycerides (TG) in patients with dyslipoproteinemia. Indapamide reduces the level of atherogenic low-density lipoprotein cholesterol (LDL) and TG, while increasing the concentration of high-density lipoprotein (HDL).
Thus, indapamide
, combining all the positive pharmacodynamic, pharmacokinetic and economic advantages, in the absence of side effects of other diuretics,
is a first-line drug for the treatment of patients with hypertension and chronic heart failure
.
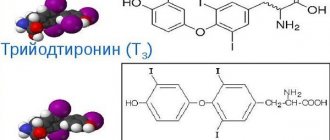
Currently, ACE inhibitors, despite their large number, according to the chemical structure responsible for the binding of systemic and tissue ACE, comprise three groups:
1. Containing a sulfhydryl group (captopril);
2. Containing a carboxyl group - carboxyalkyl dipeptides ( Enalapril
, quinapril, lisinopril, ramipril, perindopril, celazapril, benazapril);
3. Containing a phosphyl group (fosinopril).
Captopril acts as an active drug and is excreted by the kidneys, which limits its use in cases of impaired renal function and requires a minimum of twice daily use.
Enalapril
is metabolized in the body and acts due to its active metabolites, surpasses captopril in duration and potency of action, which allows its single daily use and in smaller doses compared to captopril, it is excreted through the kidneys.
Fosinopril acts through metabolites, is used once a day and has two routes of elimination - the kidneys and the gastrointestinal tract.
All ACE inhibitors have cardio-, vaso-, nephro-protective and metabolic effects:
1. Cardioprotective effects:
restoring the balance between the need and supply of myocardium O2, reducing pre- and afterload on the LV, reducing LV volume and mass, slowing down LV remodeling, reducing sympathetic stimulation, antiarrhythmic effect;
2. Vasoprotective effects:
direct antiatherogenic effect, antiproliferative and antimigration effect on smooth muscle cells, neutrophils and monocytes; improvement and restoration of endothelial function; antiplatelet effect, increased endogenous fibrinolysis, improved arterial compliance and decreased tone;
3. Nephroprotective effects:
decrease in intraglomerular hypertension, increase in glomerular filtration rate, increase in Na+-cut and decrease in K+-cut, decrease in proteinuria, increase in diuresis;
4. Metabolic effects:
increased breakdown of very low density lipoproteins and decreased TG synthesis, increased HDL synthesis, increased sensitivity of cellular receptors to insulin and increased glucose consumption.
Summarizing the above, it can be argued that today ACEIs are a promising group of drugs in the treatment of hypertension; their multidisciplinary action allows them to be called the “gold standard in the treatment of cardiovascular diseases.”
.
The purpose of this work is to study the effectiveness and tolerability of the thiazide diuretic, indapamide, and the ACE inhibitor, enalapril, in patients with hypertension.
Materials and research methods
We examined 51 patients with stage 1–2 hypertension. according to WHO classification [4]: 10 men and 41 women aged 60–78 years (mean age 66.1±3.7 years). Criteria for inclusion in the study of patients with hypertension: systolic blood pressure from 140 to 180 mm Hg, diastolic blood pressure from 90 to 110 mm Hg. The average duration of hypertension for the entire group of patients was 12.3±4.5 years.
All patients before treatment and 24 weeks after treatment underwent 24-hour blood pressure monitoring (ABPM) on the AVRM-04 complex (Hungary), registration of a standard ECG on a six-channel electrocardiograph "Kenz" (Japan), echocardiography in M and V modes on a Toshiba device – 104A” (Japan) with calculation of LV myocardial mass (LVMM) according to the formula proposed by Devereux R. and Reichek N. [8] and the LVMM index: LVMI = LVMM/body surface area. At the same time, a study of serum electrolytes (Na, K, Ca) and biochemical blood parameters was carried out: glucose content and glucose tolerance according to the standard method by collecting blood 120 minutes after a 75 g glucose load; lipid level (total cholesterol - TC, TG, HDL).
Depending on the treatment program, patients with hypertension were randomly divided into two groups: A – 26 patients received indapamide in a dosage of 1.5 to 3 mg/day; group B – 25 patients whose basic antihypertensive therapy was Enalapril
from 10 to 40 mg/day.
At the beginning of the study, patients with hypertension were prescribed one of the 2 study drugs as monotherapy in a minimal dose once a day in the morning. After the first dose of drugs, patients were under medical supervision for 2–4 hours for timely recognition of “first dose hypotension.” A control study was carried out after 4 weeks. If, according to ABPM, blood pressure reached normal values (average daily blood pressure 140/90 mm Hg or less, and average night blood pressure 125/80 mm Hg or less), the dose of the drug remained unchanged until the end of the study, i.e. up to 24 weeks. If after 4 weeks, according to ABPM results, blood pressure remained elevated (average daily blood pressure > 140/90 mm Hg and/or average night blood pressure > 125/80 mm Hg), the dose of the drug was increased. At the same time, with an average daily blood pressure equal to or more than 140/90 mm Hg, and an average night blood pressure of 125/80 mm Hg. and increased the morning dose less. When the average nightly blood pressure was 125/80 or more, regardless of the level of the average daytime blood pressure, a second (evening) dose of the drug was added. If ABPM did not show normalization of blood pressure both during the day and at night, the dose of the drug was increased again. The final dose was considered to be the maximum dose of the drug, when taken by the patient no side effects occurred, or the dose of the drug at which normal blood pressure was achieved (average daily blood pressure 140/90 mm Hg or less, and average night blood pressure 125/80 mm Hg. Art. or less). Once the final dose of the drug was reached, it remained unchanged until the end of the study, i.e. until the 24th week of treatment. At the 24th week of the study, during the last visit of the patient, ABPM and laboratory tests were repeated.
Statistical processing of the obtained data was performed using the Microsoft Excel spreadsheet software package. To establish the relationship between signs, multivariate correlation analysis was used using Pearson and Spearman tests. When processing the results and identifying correlations, the significance (probability) of deviations p<0.05 or less was used.
Treatment results
Criteria for assessing antihypertensive effectiveness
were assessed according to the following parameters:
good
– with normalization of the average blood pressure level: a decrease in SBP below 140 mm Hg.
during the day and 125 mm Hg. at night, DBP below 90 mmHg. during the day and 75 mm Hg. at night; satisfactory
– with a decrease in average blood pressure by more than 10 mm Hg.
from the initial level without its normalization; unsatisfactory
- with a decrease in average blood pressure by less than 10 mmHg.
without normalizing it. Side effects were recorded at all stages of the study. Tolerability of treatment
was assessed according to the following criteria: absence of side effects – “
excellent
”, mild side effects that do not require dose adjustment – “
good
”, side effects that resolve after dose adjustment – “
satisfactory
” and severe side effects requiring discontinuation of the drug – “
unsatisfactory
."
Figure 1 shows the results of antihypertensive effectiveness at the end of the study program in patients with hypertension, depending on the treatment program.
Rice. 1. Diagrams of the effectiveness of treatment of patients with hypertension
In group A, good effectiveness of the prescribed therapy was in 16 patients (61.5%), satisfactory – in 6 patients (23%), unsatisfactory – in 4 patients (15%); in group B, good treatment effectiveness was recorded in 14 patients (56%), satisfactory – in 9 patients (36%), unsatisfactory – in 3 patients (12%).
Table 1 shows the dynamics of the blood pressure profile, which characterizes the circadian rhythm, disturbances of which are most often found in patients with type II diabetes mellitus, with carbohydrate tolerance, with symptomatic hypertension (pheochromacytoma, hypertension of renal origin, chronic renal failure), and in the elderly.
As can be seen from the table, in group A, where indapamide was included in the treatment program, before treatment,
non-dippers
and
night-peakers
totaled 53.8%, and in group B (enalapril treatment) - 61%, respectively.
The presence of pathological non-dipper
and
night-peaker
types of daily blood pressure profile in patients suffering from hypertension can be considered an unfavorable prognostic sign.
It is well known that a “monotonic” daily rhythm of blood pressure often occurs in patients with impaired carbohydrate metabolism and is considered as one of the manifestations of insulin resistance syndrome (IR) [2]. The similar nature of disturbances in the biphasic rhythm of blood pressure in patients of the two groups suggests that these changes are markers of carbohydrate metabolism disorders. As a result of treatment with indapamide and enalapril, after 24 weeks in both groups, the number of patients with nocturnal hypertension ( night-peakers
) and insufficient nocturnal reduction in blood pressure (
non-dippers
) decreased and in group A amounted to 34.6% (almost doubled), in group B – 44%, respectively (p<0.01).
When analyzing the results of EchoCG (Table 2), after 24 weeks of treatment with enalapril, a significant decrease in the LVMM index (on average by 19%), a decrease in the thickness of the walls of the left ventricle (by an average of 12.3%) was established. Studying the Echo-CG indicators after 24 weeks of treatment with indapamide, a significant decrease in the LVMM index (on average by 29%), a decrease in the thickness of the walls of the left ventricle (by an average of 15%) was established. The differences compared to the original data are significant according to the second threshold of the probability of error-free predictions (p<0.01).
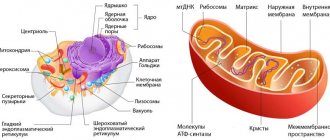
Thus, in patients receiving indapamide and enalapril, the degree of reduction in LV wall thickness was comparable. However, during therapy with indapamide, the decrease in the LVMM index was more pronounced (almost 30%), which exceeded the corresponding values (about 19.1%) for enalapril. The data obtained on the regression of LV myocardial hypertrophy coincide with the conclusions of other authors [14,16,17]. One of the possible explanations for this fact may be a progressive decrease in the number of functioning nephrons with age, due to glomerulosclerosis, with a decrease in the number of cells of the juxtaglomerular apparatus that produces circulating renin, which is a substrate for the synthesis of angiotensin, i.e. reducing the contribution of the renin-angiotensin-aldosterone system (the point of application for ACE inhibitors) in the formation of high blood pressure numbers and in the development of LVMH [7].
When analyzing the ECG, no significant changes in the PQ and QRS intervals were detected after 24 weeks of treatment with indapamide and enalapril.
According to biochemical blood parameters (Table 3), during treatment with indapamide and enalapril, a statistically unreliable moderate increase in plasma glucose was noted by an average of 2.3% (p>0.05). According to various authors, non-thiazide diuretics and ACE inhibitors do not increase the likelihood of developing type II diabetes mellitus (DM) [2,12,15].
During treatment with indapamide and enalapril, there were also no statistically significant dynamics (of different directions) in the blood lipid spectrum (p>0.05 for all indicators). The cholesterol level during indapamide therapy increased insignificantly by 0.75% (from 5.35±0.39 mmol/l to 5.39±0.49 mmol/l). As a result of treatment with enalapril, there was an unreliable but clear trend towards a decrease in total cholesterol by 5.51% (from 5.26±0.75 mmol/l to 4.97±0.52 mmol/l). Similar data were obtained when assessing influence of drugs on plasma TG. Thus, indapamide reduced the TG level by 2.4% (from 1.499±0.41 mmol/l to 1.463±0.35 mmol/l), while enalapril by 2.86% (from 1.40±0.33 mmol /l to 1.36±0.32 mmol/l), however, these changes were not significant (p>0.05). The absence of a negative effect of indapamide and enalapril on lipid metabolism has been noted in a number of studies [2,13,14,15,17,18].
The level of uric acid (UA) increased during treatment with indapamide by 2.51% (from 234.00±29.09 µmol/l to 239.88±35.95 µmol/l) and decreased by 0.89% (from 224 .30±35.93 µmol/l to 222.30±25.07 µmol/l) during treatment with enalapril. However, these changes were unreliable. In some studies [6], the level of sUA increased significantly when taking indapamide; however, P. Weidmann [18] revealed an increase in sUA with short-term therapy, and with prolonged use, the amount of sUA in the blood decreases to initial values. According to a number of authors [7], enalapril can increase the level of sUA in the blood, however, there are reports of a neutral effect of the drug [12,13]. In addition, indapamide decreased the level of urea by 3.83%, while enalapril increased it by 3.04%, but these changes were not significant (p>0.05).
During a 24-week cycle of therapy with both drugs (indapamide and enalapril), along with a decrease in blood pressure, all patients noted a noticeable improvement in their general condition, manifested by a decrease or disappearance of headache, tinnitus, and dizziness. The majority of patients improved their ability to work and tolerate daily physical activity. Of the 26 patients in the indapamide group, all patients completed the full course of treatment. Among patients in this group, 22% of patients reported no side effects - excellent tolerability. Good tolerability was found in more than half of the patients (59%). Severe side effects requiring discontinuation of the drug (poor tolerability) were not identified. The most common were dry mouth - in 8 people (30.8%), orthostatic hypotension and dizziness - in 4 people (15.4%), headaches and constipation - in 2 patients (7.7%), itching and parasthesia - in 2 people (7.7%), nausea, skin rash, lack of coordination were noted in isolated cases (3.8%).
In the enalapril group, approximately a quarter of patients (21%) reported no side effects - excellent tolerability. Good tolerability was found in more than half of the patients (52%). Severe side effects (severe dry cough) requiring discontinuation of the drug (unsatisfactory tolerability) were recorded in 4 people (16%), myalgia, dizziness, skin rash were noted in isolated cases (4%).
The discussion of the results
As is known, the level of blood pressure in the body is determined by two physiological parameters: MO (minute volume) and total peripheral vascular resistance (TPVR). This dependence can be represented as the following formula:
BP = MO x OPSS
With a sudden increase in blood pressure (increased activity of the sympathetic nervous system), the body, through the functioning of the baroreflex compensatory mechanism, reduces peripheral vascular resistance, “quenches” the effect of the increased blood pressure and helps maintain blood pressure within normal limits.
However, some individuals experience inadequate baroreflex control, which will make it difficult for the body to adequately respond to blood pressure fluctuations and contribute to the “stabilization” of high blood pressure numbers.
Thus, the main pathophysiological essence of hypertension is determined by the imbalance of vasodilating and vasoconstrictor systems
, which is aggravated by impaired metabolism of glucose and lipoproteins responsible for atherogenesis.
Figure 2 shows a diagram of the main vasoconstrictor systems and their relationship with the surface of the smooth muscle cell of the vascular bed and the sympathetic nerve ending.
Rice. 2. Scheme of the main vasoconstrictor systems and the site of action of ACE inhibitors
Norepinephrine (NA) released from the terminal endings of the neuron through postsynaptic a2-adrenergic receptors located on the surface of the muscle cell causes vasoconstriction by acting on calcium channels and increasing the concentration of ionized Ca2+ on contractile intracellular structures (actin-myosin) of smooth muscle. At the same time, released NA limits its release through stimulation of the presynaptic α2-adrenergic receptor, limiting the prolongation of the vasoconstrictor effect.
Angiotensin II (AT II), which is formed as a result of the activity of the circulating and local (tissue) RAAS, exerts its vasoconstrictor effect through several mechanisms:
– direct effect on AT1 receptors located on the surface of the muscle cell (postsynaptic receptors);
– increased release of NA from the neuron through stimulation of AT1 receptors (presynaptic) located at the nerve endings;
– increased secretion by endothelial cells of another powerful vasoconstrictor – endothelin-1;
– an increase in the entry of ionized Ca2+ into the cell (opening of slow calcium channels).
ACE inhibitors, by blocking the activity of the RAAS, reduce the versatility of the constrictor effect of hypertension II, which underlies the protective effect of ACE inhibitors for the heart, blood vessels and kidneys. By indirectly reducing the production of NA and the entry of Ca2+ into the cell (the main intracellular component of contraction), ACE inhibitors repeat the mechanism of action of such antihypertensive drugs as Ca antagonists and a2-blockers.
Indapamide-like diuretics (in particular indapamide
) the hypotensive effect is realized through the removal of Na+ from the vascular wall (reduced sensitivity of smooth muscle to the sympathetic impulse), a decrease in the concentration of Ca2+ in the myoplasm of the executive cell, a decrease in the aggregation activity of platelets and the production of thromboxane (a powerful vasoconstrictor) through the calcium mechanism, maintaining a normal level of Mg2+ concentration inside the cell – a natural, physiological antagonist of Ca.
The hypotensive effect of indapamide and enalapril in combination with metabolic neutrality (does not have a negative effect on the metabolism of glucose and lipids), confirmed by data from our studies and other authors [6,11,14,16,17], distinguishes them favorably from other antihypertensive drugs (thiazide diuretics, beta-blockers of the first and second generation) and are placed in the first line of the treatment program for hypertension.
Thus, the drugs indapamide and enalapril (ACEIs), having good antihypertensive effectiveness in combination with metabolic neutrality of glucose and lipid metabolism, have a low percentage of side effects compared to other antihypertensive drugs, they can be recommended as first-line drugs in the treatment of hypertension.
Literature:
1. Butrova S. A. Metabolic syndrome: pathogenesis, clinical picture, diagnosis, approaches to treatment. Russian Medical Journal 2001; 2: 56 – 60.
2. Kobalava Zh. D., Kotovskaya Yu. V., Shkolnikova E. E. Dynamics of daily monitoring of blood pressure and quality of life in patients with systolic hypertension during monotherapy with Arifon. Therapeutic Archives 1998; 9: 67 – 69.
3. Oganov R. G., Aleksandrov A. A. Hyperinsulinemia and arterial hypertension: returning to the findings of the United Kingdom Prospective Diabetes Study. Russian Medical Journal 2002; 10; 11: 486 – 491.
4. Recommendations of the World Health Organization and the International Society of Hypertension. 1999.
5. Shestakova M. V., Chugunova L. A., Shamkhalova M. Sh. Cardiovascular risk factors in elderly patients with type 2 diabetes mellitus and methods of their correction. Russian Medical Journal 2002; 10; 11: 480 – 485.
6. Achimastos A., Liberopoulos E., Nikas S. et al. The effects of the addition of micronised fenofibrate on uric acid metabolism in patients receiving indapamide. Curr Med Res Opin 2002; 18(2): 59–63.
7. De Rosa ML, Cardace P, Rossi M et al. Comparative effects of chronic ACE inhibition and AT1 receptor blocked losartan on cardiac hypertrophy and renal function in hypertensive patients. J Hum Hypertens 2002; 16(2): 133–140
8. Devereux R., Reicher N. Echocardiographic assessment of left ventricular mass in man. Circulation 1977; 55:613–618
9. Guidelines Subcommittee. 1999 World Health Organization: International Society of Hypertension guidelines for the management of hypertension. J Hypertens 1999; 17; 2: 151–183.
10. Kuo SW, Pei–Dee, Hung YJ et al. Effect of indapamide SR in the treatment of hypertensive patients with type 2 diabetes. Am J Hypertens 2003 Aug;16(8):623–8
11. Lacourciere Y., Belanger A., Godin C. Long–term comparison of losartan and enalapril on kidney function in hypertensive type 2 diabetics with early nephropathy. Kidney Int 2000; 58(2): 762–769.
12. Mancia G., Omboni S., Agabiti-Rosei E. et al. Antihypertensive efficacy of manidipine and enalapril in hypertensive diabetic patients. J Cardiovasc Pharmacol 2000; 35(6):926–931.
13. . Nikas S., Rizos E., Milionis H. The effects of the addition of losartan on uric acid metabolism in patients receiving indapamide. J Renin Angiotensin Aldosterone Syst 2000;1(3):289–291.
14. Ocon J, Mora J. Twenty-four-hour blood pressure monitoring and effects of indapamide. Am J Cardiol. 1990 May 2;65(17):58H–61H
15. Resnick LM Ionic basis of hypertension, insulin resistance, vascular disease and related disorders. The mechanism of "syndrome X". Am J Hypertens 1993; 6:123S–134S.
16. Tan KW, Frise SA Efficacy and tolerance of doxazosin versus enalapril in the treatment of patients with mild–to–moderate hypertension. Clin Ther 1997; 19(3): 459–470.
17. Verdecchia P., Schillaci G., Reboldi GP Long–term effects of losartan and enalapril, alone or with a diuretic, on ambulatory blood pressure and cardiac performance in hypertension: a case–control study. Blood Press Monit. 2000; 5(3): 187–193.
18. Weidmann P. Metabolic profile of indapamide sustained-release in patients with hypertension: data from three randomized double-blind studies. Drug Saf 2001; 24(15): 1155–1165.
Comparison of the safety of Enap and Enalapril
The safety of a drug includes many factors.
At the same time, in Enap it is quite similar to Enalapril. It is important where the drug is metabolized: drugs are excreted from the body either unchanged or in the form of products of their biochemical transformations. Metabolism occurs spontaneously, but most often involves major organs such as the liver, kidneys, lungs, skin, brain and others. When assessing the metabolism of Enap, as well as Enalapril, we look at which organ is the metabolizing organ and how critical the effect on it is.
The risk-benefit ratio is when the prescription of a drug is undesirable, but justified under certain conditions and circumstances, with the obligatory observance of caution in use. At the same time, Enap does not have any risks when used, just like Enalapril.
Also, when calculating safety, it is taken into account whether only allergic reactions occur or possible dysfunction of the main organs. In other matters, as well as the reversibility of the consequences of using Enap and Enalapril.
Are there differences between medications?
As a rule, the main difference between drugs lies in the pricing policy and the dosage of the active substance. Thus, Enap is a leader among patients who are prescribed minimal doses of the drug in a concentration of 2.5 mg. This category includes patients with renal and heart failure, as well as the elderly, who are recommended to take a dose of less than 5 mg per day.
Enam can be used for diabetic nephropathy
The main advantage of using Enap is its combined effect on the body, since the combination of a diuretic and an ACE inhibitor allows the drug to be used in minimal doses. The presence of an injectable form of Enap allows you to stop an acute increase in blood pressure; an ampoule of the drug must be administered every 6 hours. The duration of therapy is 48 hours, however, the use of this method of administration is possible only in a hospital setting under the supervision of specialists, which makes the analogue less popular among patients.
Monotherapy with Enalapril requires a higher dosage, which causes negative effects in the form of a nonproductive cough. It is advisable to prescribe tablets for further stabilization of the patient after a hypertensive crisis.
Thus, both medications are highly effective, and therefore are able to qualitatively stabilize blood pressure levels, restore damaged myocardial tissue, and reduce the risk of developing pathological changes in the heart and blood vessels. When choosing the best medicine, the main attention should be paid to the manufacturer, on whom the quality of the tablets and their therapeutic effect on the body depend.
Comparison of addiction between Enap and Enalapril
Like safety, addiction also involves many factors that must be considered when evaluating a drug.
So, the totality of the values of such parameters as “o syndrome” in Enap is quite similar to the similar values in Enalapril. Withdrawal syndrome is a pathological condition that occurs after the cessation of intake of addictive or dependent substances into the body. And resistance is understood as initial immunity to a drug; in this it differs from addiction, when immunity to a drug develops over a certain period of time. The presence of resistance can only be stated if an attempt has been made to increase the dose of the drug to the maximum possible. At the same time, Enap has quite a small amount of “syndrome”, however, the same as Enalapril.
Video on the topic
What's best to drink for blood pressure? Review of the most effective medications in the video:
To summarize, we can confidently say that Enalapril and Enap are prominent representatives of effective antihypertensive drugs that gently lower blood pressure, normalize cardiac activity and prevent the development of heart failure.
It is important to remember that these drugs should not be taken without consulting a specialist who will prescribe the patient adequate dosages of the medication, taking into account the degree of complexity of his illness, the presence of contraindications to use and complications from other organs.
Comparison of side effects of Enap and Enalapril
Side effects or adverse events are any adverse medical event that occurs in a subject after administration of a drug.
Enap's side effects are almost the same as Enalapril's. They both have few side effects. This implies that the frequency of their occurrence is low, that is, the indicator of how many cases of an undesirable effect of treatment are possible and registered is low. The undesirable effect on the body, the strength of influence and the toxic effect of Enap are similar to Enalapril: how quickly the body recovers after taking it and whether it recovers at all.
Contraindications and side effects
Before prescribing drugs from the group of ACE inhibitors, contraindications should be carefully studied to eliminate the risk of developing side effects from therapy in each specific case.
The drugs should not be used in patients diagnosed with:
- individual intolerance to medication components;
- tendency to develop angioedema and other forms of immediate allergic reactions;
- porphyria;
- bilateral renal artery stenosis;
- period of pregnancy and breastfeeding.
Often, ACE inhibitors cause adverse reactions, including migraine pain, a persistent decrease in blood pressure, general weakness and nausea, dizziness, and anxiety.
You should not take Enap or Enalapril without a doctor's prescription, since such actions can aggravate the condition of a sick person and provoke the development of acute variants of coronary heart disease or rhythm disturbances.
Comparison of ease of use of Enap and Enalapril
This includes dose selection taking into account various conditions and frequency of doses. At the same time, it is important not to forget about the release form of the drug; it is also important to take it into account when making an assessment.
The ease of use of Enap is approximately the same as Enalapril. However, they are not convenient enough to use.
The drug ratings were compiled by experienced pharmacists who studied international research. The report is generated automatically.
Last update date: 2020-12-04 13:42:31
Reviews from doctors
Ekaterina Gromova, general practitioner, Nizhny Novgorod: “I prescribe Enap for hypertension and ischemia as a prevention of heart attack. I recommend enalapril for unstable angina in complex treatment. Patients do not always follow doctor's instructions. Arriving at the pharmacy, they buy the cheaper drug Enalapril. There are almost no complaints about side effects. Both drugs are well tolerated if the dosage is not violated.”
We recommend reading: Meloxicam and Diclofenac: which is better?
Svetlana Kartashova, general practitioner, Rostov-on-Don: “I consider Enap a more effective remedy than Enalapril, but many patients prefer inexpensive drugs. I prescribe medication for grade 1-2 hypertension. If the disease is severe, I prescribe several medications. One of the side effects I can mention is a dry cough. In this case, I reduce the dosage or select another drug.”
Patient reviews
Valery Kravtsov, 53 years old, Krasnodar: “As soon as I turned 50 years old, many ailments appeared, incl. The pressure began to rise. I had to undergo an examination, after which the doctor diagnosed arterial hypertension and prescribed Enap. The medicine is not cheap, but I bought it and started taking it. The condition improved after about a month.
I decided to look for analogues and came across Enalapril, which is much cheaper. I bought it and started taking it in the same dosage that the doctor prescribed. There were no side effects, both drugs were equally effective, so I settled on the cheaper one.”
Irina Romanova, 47 years old, Sochi: “Enalapril was prescribed by a therapist after he diagnosed stage 2 hypertension. Due to problems with the thyroid gland, the doctor recommended the minimum dosage. There were no side effects, so the dosage was gradually increased to 10 mg. I began to feel much better, but after a few months the drug stopped working.
I went to the doctor and told about my problems. He prescribed another drug - Enap, warning that this medicine was more expensive. I started taking it. This medicine is gentler and more effective. It’s helping for now, but I don’t know what will happen in a year.”
Nina Kruglitskaya, 54 years old, Khabarovsk: “I’ve been taking Enalapril for about a year. The pressure remains normal. When I started taking the medicine, I suffered from a dry cough. I thought it was bronchitis and went to the doctor. But the doctor said that this is a side effect that often happens when taking this medication. He suggested replacing it with something else, but the cough went away, so she continued taking Enalapril. I feel good so far.”
We recommend reading: What is the difference between the drugs Betaserc and Betahistine?