Sudden death
Definition
. Sudden cardiac death (SCD) is defined as: “natural death due to cardiac causes, characterized by sudden loss of consciousness within one hour of the onset of symptoms; the presence of heart disease may be known, but the timing and mechanism of death is unpredictable.” The key concepts guiding the definition of sudden death are that the cause is non-traumatic and that the onset of death is immediate and unpredictable. When considering the problem of sudden death within heart diseases, the word “cardiac” was introduced into the term.
What are the causes of SCD in young athletes?
In 80% of cases, SCD occurs in athletes over 35 years of age and is due to atheromatosis of the coronary arteries. But, given the fact that in elite sports sudden death of very young athletes (<35 years old) has become increasingly common, the main focus of the study is directed specifically at them.
SCD is based on hereditary, congenital structural abnormalities, as well as abnormalities of the conduction system of the heart (electrical abnormalities).
The most common cause of sudden death in young athletes is cardiomyopathies. There are several types: hypertrophic cardiomyopathy, arrhythmogenic right ventricular hypertrophy, idiopathic left ventricular hypertrophy and dilated cardiomyopathy. Given that the first two species account for almost 50% (Bruckner et al 2013) of sudden death in young athletes reported in the literature, we will focus on them.
Hypertrophic cardiomyopathy. An inherited condition characterized by thickening of the heart muscle in the left ventricle. At maximum and submaximal loads, it disrupts the functioning of the conduction system of the heart, causing fibrillation.
Arrhythmogenic right ventricular cardiomyopathy: is also an autosomal dominant hereditary condition. This disorder predominantly affects the right ventricle, although in severe cases it may also affect the left ventricle. The condition is characterized by the replacement of myocardial cells with a connective-fatty structure, which, due to such anatomical changes, has a key effect on the conduction system of the heart and is fatal during severe chronic physical exertion.
Congenital abnormalities in the structure of the coronary arteries cause 1/5 of the incidents of sudden death among young athletes. Such abnormal connections between coronary arteries can be compressed by hypertrophied myocardium, causing acute ischemia. Sudden death in the setting of normal cardiac structure is primarily due to congenital ion channel defects and accounts for approximately 4% of sudden deaths in sports. Such conditions include long QT syndrome, Brugada syndrome, ventricular arrhythmias due to a sharp increase in catecholamines, short QT syndrome, WPW syndrome, severe electrolyte disturbances, hypothermia and hyperthermia, drugs (amphetamine, cocaine). Other causes include cardiac arrhythmias due to myocarditis due to infection.
Commodio cordis may be another cause of sudden death in young healthy people, resulting from blunt mechanical shock to the chest (in contact sports), which during the vulnerable phase of myocardial repolarization can cause fatal ventricular fibrillation.
Causes
Epidemiology
. One of the leading causes of death in the adult population of developed countries is SCD due to coronary heart disease. In patients with sudden cardiovascular collapse, the rhythm of ventricular fibrillation is most often determined on the ECG (in 75-80% of cases), while bradyarrhythmias are the cause of SCD in a minimal number of patients. In 5-10% of cases of sudden cardiac death, patients do not have coronary heart disease or congestive heart failure. According to statistical data obtained annually in Western countries, the incidence of SCD varies from 0.6 – 1.28 per 1000 people per year. These studies only include data on those killed or resuscitated by emergency medical services; thus, official data are lower than the actual number of SCD cases in the general population.
Prevention of sudden cardiac death: general population and high-risk group. Among the adult population, the incidence of SCD is 1 in 1000 per year. Prophylactic interventions to reduce the risk of sudden cardiac death in this population appear to be neither practical nor cost-effective, since the costs include the remaining 999 per 1000 people per year who are not at risk for SCD. Thus, general principles of a healthy lifestyle are recommended in the general population.
Subgroups in which the annual risk of sudden cardiac death progressively increases are relatively few. It follows from this that promoting a healthy lifestyle among the population will naturally lead to a decrease in the number of patients with coronary heart disease, which in turn will reduce the number of cases of sudden cardiac death.
Fall asleep and not wake up. Why do tragedies happen in dreams?
Cardiovascular diseases are the scourge of modern society. In world statistics, this is the most common cause of death. In Russia alone, about two hundred thousand people a year die from sudden cardiac arrest. The most difficult thing to comprehend is the loss if the person felt well the day before, but did not wake up in the morning.
We talked about the causes of the tragedy and ways to prevent it with cardiologist Tatyana Mikhailovna Kolomeytseva.
— Tatyana Mikhailovna, what can cause a person’s heart to suddenly stop?
As a rule, this is a consequence of existing diseases: coronary heart disease, hereditary cardiomyopathies, congenital heart defects and conduction system. The cause is also thrombosis, spasm of the coronary vessels.
In Russia alone, about two hundred thousand people a year die from sudden cardiac arrest.
— Can a tragedy happen to an absolutely healthy person whose cardiovascular system has never failed?
An absolutely healthy person is not at risk of dying from a heart attack. However, heart disease (in particular, coronary artery disease) can be asymptomatic. In this case, the tragedy becomes the result of an undiagnosed pathology.
“Chronic heart failure (one of the forms of coronary artery disease) is present in 7% of the country’s population.” Quote from the material: “Coronary heart disease: diagnosis and treatment”
— People who are far from medicine associate heart disease with stress or physical activity. But in a dream a person is absolutely calm. Are there any risk factors specific to sleep?
No. The dangers come from the pathologies already listed: both in sleep and while awake.
— Could sleep quality indicate an increased risk of sudden death?
Obstructive sleep apnea is especially dangerous. Its main manifestation is snoring. A person suffering from apnea often does not get enough sleep, does not have time to regain strength during the night, suffers from drowsiness during the daytime, and is also susceptible to increased blood pressure upon awakening.
— Diseases not directly related to the cardiovascular system can become an additional risk factor?
Of course they can. These conditions include diabetes mellitus, obesity, kidney pathology and neurological diseases.
— What age is the most dangerous for cardiac arrest?
The incidence of cardiac disorders increases with age. Therefore, the older the person, the higher the risk.
- When should you be wary? Are there symptoms that allow us to foresee such a dangerous condition in advance?
Warning signs may appear two weeks before cardiac arrest. These are fatigue, shortness of breath, arrhythmia. The most threatening symptom is fainting. They cannot be ignored.
The most threatening symptom is fainting. They can't be ignored
Statistics show that in three out of four cases sudden death was preceded by corresponding symptoms. Therefore, it is important to pay attention to your well-being.
— Not everyone is used to taking care of their health. When a person himself does not talk about his health, can loved ones guess that help is needed? What external manifestations should cause alarm?
From the outside, it is more difficult to predict the impending disaster. But if a person suddenly reduces the pace of activity and cannot cope with his usual workload, this is an alarming symptom. Gait slows down and endurance decreases. It is worth consulting a doctor if your friend or relative does not keep up with you while walking, although you are walking at the speed that is usual for both of you.
Another noticeable symptom is snoring. This is a marker of obstructive apnea.
— Can genetic tests help identify predisposition to heart disease?
Only in the case of hereditary cardiomyopathies. It is not the leading cause of sudden cardiac death. It occupies no more than 20% of the total. To judge the hereditary nature of cardiomyopathy, it is necessary to examine three generations of the same family.
“The main danger is the possibility of sudden cardiac arrest. Therefore, patients with new-onset atrial fibrillation are immediately hospitalized.” Quote from the material “Recognizing the enemy of the heart. What is arrhythmia?
— Recently, fitness bracelets have become widespread. They are worn to control their motor activity. How accurately do they measure the pulse and can they help suspect problems in the cardiovascular system?
It is impossible to talk about fitness bracelets as a full-fledged diagnostic tool. They only measure the pulse, this is not enough to make final conclusions. But they can warn of impending danger. You should be wary if the bracelet detects rhythm disturbances. Simpler models for arrhythmia may simply malfunction - this is also a reason to see a doctor.
“The symmetry of the pulse is affected by a decrease in the lumen of one of the arteries, its incorrect location.” Quote from the material “What should an adult’s pulse be: normal and pathological”
— If cardiac arrest does occur in a dream, can the person be helped somehow?
Most often in this case the person is left without help because there are no witnesses. But if you managed to notice it in time, you need to call an ambulance as quickly as possible.
- What is dangerous for our heart? How to reduce the risk of cardiovascular diseases?
The cardiovascular system suffers from bad habits (in particular, smoking) and chronic emotional overload. Poor nutrition also poses a danger: irregular, with a lot of fat.
To preserve your heart, you need to lead a healthy lifestyle. Give yourself feasible and regular physical activity.
If cardiac pathologies have already been detected, it is important to regularly visit a doctor and follow all recommendations.
“If it was not possible to prevent the tragedy, people can only hope that their loved one at least did not experience pain and fear.” But is there any reason for such hope?
Of course, no research has been done. But it is known that with fatal arrhythmias, consciousness fades very quickly. The parts of the brain responsible for the perception of pain do not function. Therefore, a person does not experience torment.
Other materials on topics:
How to keep your heart healthy?
Serious question: what happens to the heart during an angina attack?
Heart, why don't you want peace? What causes tachycardia?
For reference:
Kolomeytseva Tatyana Mikhailovna
In 2008 she graduated from the Moscow Medical Academy named after. THEM. Sechenov with a degree in medical and preventive care.
In 2009 – professional retraining at the Moscow Medical Academy named after. THEM. Sechenov with a degree in General Medicine. He has professional retraining at the Russian State Medical University of Roszdrav in the specialty “Cardiology”. Completed professional development on the topic “Pulmonary hypertension: clinical workshop” at the European Health Center in Otwock (Poland)
In 2015 – advanced training at the National Medical and Chemical Center named after. N.I. Pirogov “Anticoagulants for atrial fibrillation.” In 2021 – professional development on the topic “Complex issues in the diagnosis and treatment of pulmonary hypertension” on the basis of the RKNPK named after. Myasnikova
In 2017-2018 – advanced training at the First Moscow State Medical University named after. THEM. Sechenov “Modern aspects of diagnosis and treatment of chronic heart failure.”
Member of the Russian Society of Cardiologists.
Has a certificate of a specialist in the specialties “Therapy”, “Cardiology”
Currently working as a cardiologist at Clinic Expert Tula LLC. Receives at the address: st. Boldina, 74
Risk factors for sudden cardiac death in the population
| Non-modifiable risk factors | Modifiable risk factors |
| Age | Smoking |
| Male | Hypertension |
| Family history of coronary heart disease | Elevated LDL levels |
| Genetic factors | Diabetes |
| Obesity |
Prevention of SCD: recommendations of the European Society of Cardiology
The European Society of Cardiology Specialist Group on Sudden Cardiac Death presents recommendations aimed at reducing the incidence of SCD. The recommendations are presented in tables and distributed as follows:
Class I:
Reliable evidence and/or consensus among experts that a given procedure or treatment is appropriate, beneficial and effective.
Class II:
Conflicting evidence and/or differences in expert opinion about the benefit/effectiveness of a procedure or treatment.
Class IIa:
evidence and/or expert opinion for benefit/effectiveness predominates.
Class IIb
: Benefit/effectiveness is not well supported by evidence and/or expert opinion.
In these guidelines, the terms “primary” and “secondary” prevention are used primarily in the context of ventricular arrhythmia. Therapy prescribed to prevent the development of sustained ventricular arrhythmias in patients without a history of episodes of life-threatening ventricular arrhythmias, but classified as at high risk for their development, refers to “primary” prevention. The therapy recommended for patients with cardiac arrest and syncope/hypotension secondary to paroxysmal ventricular tachycardia is “secondary” prevention.
What are the markers of SCD, what should you pay attention to?
- Sudden fainting (syncope) dizziness during exercise.
- Hypertrophic cardiomyopathy in relatives or a history of sudden death of relatives under 50 years of age.
- Severe left ventricular hypertrophy (>30mm).
- Unsustained ventricular tachycardia.
- Reduced blood pressure as a response to physical activity.
I. Myocardial infarction and heart failure
A. Risk stratification
Both non-invasive and invasive tests are used to determine the risk of SCD in patients with a history of myocardial infarction.
Risk stratification in patients who have had myocardial infarction
with/without development of HF
| Class | I | IIa | IIb |
| Demographic variability LVEF HR or BR sensitivity LV volume | ES unstable VT resting heart rate | Late potentials EPI Dynamics h. T Patency of the infarct-dependent artery |
LVEF – left ventricular ejection fraction; HR – rhythm variability
BR – baroreflex; ES – extrasystole; VT – ventricular tachycardia
HR – heart rate; h. T – T wave
B. Primary and secondary prevention of SCD in patients with a history of MI
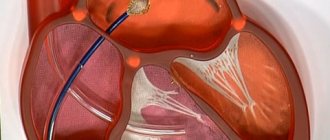
Sudden cardiac death occurs most often among patients who have had a myocardial infarction. In this group, primary prevention includes drug treatment with beta blockers, aspirin, ACE inhibitors and cholesterol-lowering drugs. In patients with documented sustained VT or VF, the alternative is an implantable cardioverter-defibrillator (ICD) or amiodarone, and in selected cases, ablation or surgery. In patients with a history of myocardial infarction, a decrease in LVEF less than or equal to 40% (less than or equal to 5%) and clinically symptomatic paroxysms of non-sustained VT, or induced sustained or non-sustained VT by programmed electrical stimulation (EPS), the recommended treatment is CD implantation. For secondary prevention of SCD, the use of CD is recommended for those resuscitated after VF and patients with hemodynamically symptomatic VT paroxysms.
Primary prevention in patients who have had a myocardial infarction with/without the development of HF
| Class | I | IIa | IIb |
| History of MI | Beta blockers ACE inhibitors Cholesterol-lowering drugs Aspirin | Polyunsaturated fatty acids Amiodarone | |
| MI + LV dysfunction | Beta blockers ACE inhibitors Aldosterone receptor blockers | Amiodarone | |
| Hemodynamically asymptomatic VTs | Amiodarone Beta blockers | CD Ablation Surgical treatment | |
| LVEF less than or equal to 40% + paroxysms of non-sustained VT + inducible sustained VT with EPI | KD |
Secondary prevention in patients who have had a myocardial infarction with/without the development of HF
| Class | I | IIa | IIb |
| VF | KD | ||
| Hemodynamically symptomatic sustained VT | KD | Amiodarone Beta blockers |
Sudden cardiac death in chronic heart failure - SCD-HeFT study
Description: The purpose of the study was to evaluate the effectiveness of amiodarone or implantable cardioverter defibrillator (ICD) therapy with placebo in patients with New York Heart Association (NYHA) classes II and III congestive heart failure and reduced left ventricular ejection fraction. (LVEF) ≤35%.
Study design
Number of patients: 2,521
NYHA class: 70%; NYHA class II and 30% class III
Average follow-up: average follow-up 45.5 months
Average age of patients: 60 years
Female: 23%
Base average EF: 25%
Patient Populations:
1) 18 years and older.
2) Heart failure for at least 3 months and treatment with a vasodilator.
3) Symptomatic CHF (NYHA class II and III) due to ischemic or non-ischemic dilated cardiomyopathy.
4) LVEF ≤35% within 3 months of enrollment.
5) All patients are encouraged, but not required, to have a coronary angiogram to document the nature of their disease. The definition of ischemic cardiomyopathy would be LV systolic dysfunction in the presence of ≤75% luminal coronary artery disease or mild coronary artery disease with overt evidence of myocardial infarction (MI).
6) Patients with chronic atrial fibrillation should be anticoagulated with warfarin, with documented international reference ratios of at least 2.0, for ≥21 days before randomization.
Exceptions:
1) Symptomatic ventricular arrhythmia.
2) LVEF >35% or asymptomatic LV dysfunction.
3) NYHA class IV CHF.
4) History of cardiac arrest or spontaneous episode of sustained ventricular tachycardia (VT) (≥30 seconds at a rate >100 beats per minute) not associated with an acute Q-wave infarction. (Sustained VT or cardiac arrest within 48 hours of MI is not an exclusion criterion).
5) Any non-cardiac disease that is likely to cause death within 12 months.
6) Women who are pregnant or of childbearing potential and are not using reliable contraceptive methods.
7) A history of restrictive, infiltrative or hypertrophic cardiomyopathy; constrictive pericarditis; acute myocarditis; Congenital heart defect; surgically correctable valve disease; and/or inoperable obstructive valvular disease.
 A history of mechanical prosthetic heart valves.
A history of mechanical prosthetic heart valves.
9) History of serious mental disorder, active alcohol/drug abuse or non-compliance.
10) Contraindication for taking amiodarone for any reason or currently taking amiodarone.
11) Indications for the use of antiarrhythmic drugs.
12) Atrial fibrillation requiring catheter ablation of the atrioventricular conduction system or amiodarone for rate control.
13) Unexplained fainting over the past five years.
14) Patients cannot place an ICD in the left subclavian region.
15) Expected to undergo a heart transplant within 12 months.
16) Permanent pacemaker.
17) Liver function tests (>2.5 times normal or serum creatinine >2.5 mg/dL).
18) Currently receiving antibiotics.
Primary endpoints:
Mortality from all causes
Secondary endpoints:
1) Arrhythmic cardiac mortality.
2) Non-arrhythmic cardiac mortality.
3) The combination of mortality from all causes and readmission for CHF.
4) Health-related quality of life.
5) Cost of maintenance and calculation of additional cost-effectiveness ratios.
Medicines/procedures used:
Patients were randomized in a double-blind manner to 1) conventional CHF therapy and placebo, 2) conventional CHF therapy plus amiodarone, or 3) conventional CHF therapy plus conservatively programmed single-lead CAD. Amiodarone was administered at 800 mg for the first week, 400 mg for weeks 2–4, and chronically at 200 mg/day if <150 lbs, 300 mg/day if 150–200 lbs, and 400 mg/day. if >200lbs,
The ICDs were programmed to treat ventricular fibrillation (VF) only. Patients underwent a six-minute walking test and Holter monitoring.
Main conclusions:
At the end of follow-up, medication use included 72% angiotensin-converting enzyme inhibitors, 78% beta blockers, 80% loop diuretics, and 55% aspirin. The baseline average six-minute walk was 1,130 feet. Previous duration of CHF was 24.5 months at baseline.
There was no difference in all-cause mortality between amiodarone and the placebo group (28% vs 29%, hazard ratio [HR] 1.06, 97.5% confidence interval [CI] 0.86–1.30, p= 0.53), but mortality was lower in the ICD arm compared with placebo (22% vs. 29%, HR 0.77, 97.5% CI 0.62–0.96, p = 0.007). Subgroup analyzes showed similar results comparing amiodarone with placebo in prespecified subgroups, with the exception of NYHA class III, which had increased mortality in the amiodarone group (HR 1.44, 97.5% CI 1.05-1.97; n= 497).
Long-term follow-up: Median follow-up was 11 years, available for approximately 90% of patients. The overall conversion rate to the ICD group was approximately 57%. Ten-year mortality with ICD and placebo: 52.5% vs 57.2% (HR 0.87, 95% CI 0.76-0.98; p = 0.028); for amiodarone versus placebo: 52.7% versus 57.2% (HR 0.96, 95% CI 0.85–1.09; p = 0.54). When treatment benefit was considered as a function of time from randomization, a decrease in ICD benefit was observed after 6 years (p for interaction = 0.0015). For ICDs and placebo, the greatest benefit was seen in patients with ischemic cardiomyopathy and in patients with NYHA class II. Ischemic HF: HR 0.81, 95% CI 0.69-0.95; p = 0.009; non-ischemic HF: HR 0.97, 95% CI 0.79-1.20; p = 0.80. NYHA functional class II: HR 0.76, 95% CI 0.65-0.90; p = 0.001; NYHA functional class III: HR 1.06, 95% CI 0.86-1.31; p = 0.58.
Conclusions:
Among patients with NYHA class II or III CHF and reduced LVEF, treatment with an ICD was associated with a reduction in all-cause mortality compared with placebo, but there was no difference between amiodarone and placebo. The ICD was programmed to treat VF only.
With long-term follow-up, there may potentially be some reduction in benefit after 6 years, although the conversion rate to the ICD group was >50%. The benefit was greatest among patients with ischemic cardiomyopathy and NYHA class II symptoms.
II. Cardiomyopathies
Hypertrophic cardiomyopathy (HCM)
HCM is a relatively common cardiac disorder (incidence in adults approximately 1:500) in which sudden cardiac death is the most likely outcome at any age, but is most common in young, often asymptomatic patients. Implantation of a CD for the prevention of sudden cardiac death is strongly justified in patients who survive cardiac arrest (secondary prevention). Prophylactic use of KD is also possible in patients with two or more risk factors.
Hypertrophic cardiomyopathy
| Class | I | IIa | IIb |
| Risk stratification | Sustained VT VF | Family history of SCD Syncope LV hypertrophy (VSD greater than cm) Unsustained VT Hypotension during exercise stress test | High risk of mutations |
| Primary prevention | KD | Amiodarone | |
| Secondary prevention | KD |
VSD – thickness of the interventricular septum
Arrhythmogenic right ventricular dysplasia (ARVD)
ARVD is one of the main causes of sudden cardiac death in the “pre-coronary” age group. Although the predisposing factors for SCD have not yet been sufficiently studied in large prospective studies, sudden cardiac death occurs more often in patients with significant changes in the right ventricle, as well as in those with LV involvement. In those resuscitated after SCD (secondary prevention), in patients with sustained VT and ineffective antiarrhythmic therapy, and in high-risk patients with documented paroxysms of VT, the most adequate treatment is CD implantation.
Arrhythmogenic right ventricular dysplasia
| Class | I | IIa | IIb |
| Risk stratification | Sustained VT/VF Dilation of the RV RV dysfunction Inducible VT/VF with EPI | Family history of SCD Late potentials + LV dysfunction VT Inducible VT/VF with EPS | |
| Primary prevention | KD | Antiarrhythmic drugs | |
| Secondary prevention | KD |
RV – right ventricle; EPI – electrophysiological study
Dilated cardiomyopathy (DCM)
SCD is one of the most common mechanisms of death in DCM, especially in the early stages of the disease. Ejection fraction (EF) has been shown to be the most accurate predictor of outcome for both sudden cardiac death and death in advanced HF. The frequency of syncopal episodes is also considered one of the reliable risk factors for sudden cardiac death.
General therapeutic strategies aimed at reducing the risk of SCD in patients with DCM include the use of ACE inhibitors, beta blockers and aldosterone receptor antagonists, while amiodarone and CD implantation are used in individual cases. Several studies examining the role of antiarrhythmic drugs in patients with DCM have provided evidence (not statistically proven) that drug treatment recommended for patients who have had an MI with development of HF is equally effective in patients with DCM. The use of CDs for secondary prevention is considered acceptable; implantation of CDs is also recommended in high-risk patients for the primary prevention of sudden cardiac death.
Dilated cardiomyopathy
Class
| I | IIa | IIb | |
| Risk stratification | Sustained VT VF | Syncopations | Decreased EF Unsustained VT |
| Primary prevention | ACE inhibitors Beta blockers | KD Aldosterone receptor blockers | Amiodarone |
| Secondary prevention | KD ACE inhibitors Beta blockers | Aldosterone receptor blockers | Amiodarone |
Prevention of sudden death in patients with CHF
Oksana Mikhailovna Drapkina , professor, doctor of medical sciences:
- Well, now I already see my friend, our friend - Professor Alexey Nikolaevich Turov. I would like to say that we are starting a new project - “Presentation of therapeutic basic schools in Russia.” And today, at the 33rd Internet session under the leadership of Professor Turov, we present... Well, in general, this school does not even need an introduction, but nevertheless. This is the Novosibirsk Research Institute of Circulatory Pathology named after Academician Meshalkin, which was created in 1957. The founder and first long-term leader was Academician Evgeniy Nikolaevich Meshalkin. In 2012, surgical high-tech treatment was carried out on 20 thousand patients. More than 70 thousand people were consulted. The bulk of the interventions were carried out using federal budget funds. And this institute is the largest executor of the state federal task in the profile of cardiovascular surgery.
Aleksey Nikolaevich is generally an innovator, a very passionate and enthusiastic person about medicine. You'll see it now. He represents the program, today he shaped it. Therefore, all the pros, all the cons – everything goes to him. I want to say that Alexey Nikolaevich is a Doctor of Medical Sciences, Associate Professor of the Department of Internal Medicine, Faculty of Medicine, Novosibirsk University, leading researcher at the Center for Surgical Arrhythmology at the Meshalkin Research Institute of Circulatory Pathology; popularizer of catheter technologies for heart rate correction, author of many electroanatomical mapping techniques, co-author of a new direction in the treatment of atrial fibrillation, ablation of the ganglion plexuses of the left atrium. And he was the initiator of the creation of the electrophysiological society.
Well, Alexey Nikolaevich, it’s almost 20 o’clock for you, and we’re listening to you with impatience, as usual.
Alexey Nikolaevich Turov , associate professor, doctor of medical sciences:
– Good afternoon, dear colleagues. Thank you very much for such a flattering introduction. And today we will begin to talk about the problem of sudden cardiac death. Today I would like to talk about this problem in relation to a very narrow category of patients, namely patients with heart failure.
Of course, there is no need to talk about how pressing the problem of sudden death is. The United States has the greatest statistics. And we see that in this country, sudden death is the number one killer. That is, it claims more than 450 thousand lives annually. And this is much more than the four leading causes of death combined: strokes, lung cancer, breast cancer and HIV infection. That is, this is really currently the number one problem not only in cardiology.
If we look at the structure of sudden cardiac death, we will see that 88% are still life-threatening arrhythmias, that is, sudden cardiac death can rightfully be equated in terminology to sudden arrhythmic death. If we now look at the structure of life-threatening arrhythmias, we will see that primary ventricular fibrillation develops very rarely. Bradyrhythmic death is also a fairly rare situation. Torsade de pointes tachycardias are rarely a cause of death. And the most common situation is rapid ventricular tachycardia, which, having begun, then transforms into ventricular flutter, then into large-wave ventricular fibrillation, then into small-wave ventricular fibrillation, and everything ends with secondary asystole.
We see that this entire process takes only a few minutes. And we also know that the success of resuscitation efforts is determined by time. Every minute the chances of saving a patient's life decrease by 10%. Therefore, if we started resuscitation measures by the ninth minute, then this probability is no more than 10%, and if we started resuscitation measures within the first minute, then this is the greatest chance of saving the patient. This is why resuscitators talk about the so-called “golden” first minute. Naturally, during the history of the development of cardiology, there were a lot of social aspects, social events, the task of which was precisely to bring medical care as close as possible, so that resuscitation was provided to the patient within the first minute.
Here are some of these social strategies. First of all, this is the territorial concentration of patients with cardiac pathology. This concept has been developed in some capitals, in some countries, where patients with severe cardiac pathology have benefits for settling in certain areas, which, as they say, are stuffed with specialized cardiological institutions. Then specialized help arrives within a few minutes.
Then, there are specialized highways on which the passage of cardiac intensive care vehicles is allowed, which are devoid of speed limits and traffic lights, and can reach speeds of more than 100 kilometers per hour. Again, in a matter of minutes a doctor can be in any area of the city. The so-called air medicine service, cardiological medicine, solves the problem of traffic jams even more.
Finally, in the United States in the late 1980s, so-called Early Defibrillation programs were actively developed. They were aimed at ensuring that the first person who saw another person fall would begin resuscitation using external automatic defibrillators. These are, as they say, smart devices that are able to independently recognize the state of the patient’s rhythm. And if this condition is life-threatening, they will perform cardioversion using special technology, according to a special algorithm. This program included awareness of the general population, mass placement of external automatic defibrillators in those places where the maximum outburst of emotions occurs: stadiums, airports, railway stations, film holdings, casinos, and so on; and a video surveillance system. All these social programs, of course, bring some great benefits. But nevertheless, we must not forget that all of them are designed for first aid to others so that the surrounding people detect a cardiac catastrophe. At the same time, we know that 40% of all sudden deaths occur without any witnesses. And 80% of all cases of sudden death occur not in society, but at home. And besides this, we also know that the time for defibrillation and the time for resuscitation still could not be reduced to this first, so-called “golden” minute.
If we use modern ambulance teams in large cities, then on average help begins at the 24th minute. If medical towns are the sixth minute. Specialized highways - the fifth minute, helicopters - the fourth minute. The Early Defibrillation program still begins to operate, starting from the second minute after the patient falls. And please note that only an implantable cardioverter-defibrillator, a fully automatically implanted device, allows you to deliver this first life-giving shock, the first shock, within the first 30 seconds. Therefore, they naturally have no alternative, not in terms of other social activities, not in terms of medications.
Therefore, nothing more can be said about implantable cardioverter defibrillators other than that they are a life-saving device. Currently, these devices have shrunk in size to virtually the size of pacemakers. And here we see an example of a printout from this device, when this device detected a dangerous, life-threatening arrhythmia, ventricular flutter. Delivered a 10 joule shock and restored sinus rhythm. Please note that all of this took only seven seconds. That is, a life-threatening, dangerous situation passed within seven seconds. Of course, we can no longer talk about any other alternative in terms of preventing sudden death, sudden arrhythmic death.
Which patients are at greatest risk for sudden death? Let's look at the most common Bigger risk stratification. Bigger divided the risk of sudden death into three classes. These are benign situations, potentially malignant situations and malignant situations. Please note that the basis was based on three factors. This is a lesion of the heart, this is the structure of the arrhythmia and the clinical picture that the patient has. Moreover, Bigger gave primary importance to the degree of heart damage. If it is absent, this is a benign class; if there is gross cardiac pathology, this is the second class. And if there is a complicated, severe cardiac pathology, reduced ejection fraction, severe hypertrophy, left ventricular aneurysm - this is the third class.
The structure of arrhythmia is of secondary importance. Thus, if a patient has sustained ventricular tachycardia, but at the same time he has a completely anatomically healthy heart, there is no cardiac pathology, then this patient still ends up in first class. That is, in the benign class for the risk of sudden death. And on the contrary, if the patient has only ventricular extrasystoles, single extrasystoles, but at the same time a low ejection fraction - below 40% - he nevertheless finds himself in the third class, that is, he has a malignant class for the risk of sudden death.
Thus, dear colleagues, it is the ejection fraction that is the main, most important risk factor for sudden death, in which all other other factors are already dissolved. And an ejection fraction below 30% increases the risk of sudden death by more than eight times.
We know that there are many cardiac drugs available. We know of numerous studies in which these drugs showed a decrease in mortality in patients with cardiac pathology: beta blockers, aspirin, statins, ACE inhibitors. But please look, despite the reduction in overall mortality, in all these studies the rate of sudden death is high. Half of the patients in these studies died suddenly. Therefore, it is no secret that, of course, there were studies in which cardioverter-defibrillators were studied in patients with heart failure, where the main target was not ventricular arrhythmia, but rather low systolic function of the left ventricle.
And the first such study was the Madit study. It involved 196 patients. All of these patients had previously suffered a myocardial infarction. Please note that they had non-sustained ventricular tachycardia. Unsustained ventricular tachycardia is an arrhythmia that exists for no more than 20 seconds. That is, this is an arrhythmia that was accidentally detected during daily monitoring. All patients had low ejection fraction. And these patients underwent an intracardiac electrophysiological study, during which monomorphic ventricular tachycardia was induced. And she was refractory to intravenous procainamide, a powerful antiarrhythmic drug.
It was clear that if such a malignant situation, then, of course, cardioverters should have a powerful preventive effect in terms of sudden death. Indeed, cardioverter defibrillators increased patient survival by 75% compared with traditional therapy.
The next study is the Mustt study. It had a somewhat confusing design. But what should interest us is that these, again, were patients who had suffered a myocardial infarction. But the ejection fraction has already been increased to 40%. Again, all patients underwent electrophysiological intracardiac testing. Ventricular tachycardia was induced in all. And after that, patients were randomized based on electrophysiological testing. Some patients received cardioverter defibrillators, and some patients received antiarrhythmic drugs based on intracardiac electrophysiological studies. These were a variety of drugs: Amiodarone, Sotalol, drugs of the first “A” class. And 46% received cardioverter defibrillators.
As a result, when five-year mortality was assessed, it turned out that therapy that was selected on the basis of intracardiac EPS reduced the five-year mortality of these patients. But when this therapy was divided into two branches, it turned out that implantation of EPS-based cardioverter-defibrillators actually halved the five-year mortality rate.
But please pay attention. Antiarrhythmic drugs, which were selected on the basis of EPI, on the contrary, increased five-year mortality. It was as a result of this study that the management of patients changed. And at present, intracardiac electrophysiological testing is not required for high-risk patients. As they say, the researchers concentrated as much as possible on a single factor, namely, the ejection fraction.
The next study, Definite, addressed non-ischemic heart failure for the first time. This is 458 patients with an ejection fraction below 35%. Again, let's see that the ventricular events were completely asymptomatic. As a result, arrhythmic mortality decreased by 80% under the influence of cardioverter defibrillators. But when overall mortality was assessed, it turned out that it also decreased by 35%, but these differences were not significant. Therefore, this study temporarily suspended the study of cardioverters in patients with non-ischemic etiology.
The next study is the Madit-II study, which again returned to post-infarction patients. Please note that the inclusion criterion does not have any arrhythmic criterion. This is a previous heart attack and low ejection fraction. The patients were divided into two groups. 742 patients received a cardioverter-defibrillator. As a result, patients in the cardioverter-defibrillator group had a 31% better survival rate compared to patients who received traditional therapy.
And finally, the last and largest study is SCD-HeFT. It included more than two thousand patients, long-term, multi-year observation. It, again, returned to any form of heart failure. This study included patients with both ischemic and nonischemic failure. The main criterion was low ejection fraction. And again, please note: at the time of inclusion there were no arrhythmic indications for implantation of cardioverter defibrillators and stimulators. The study took place at 168 sites in North America and New Zealand. Patients were divided into three groups: patients receiving placebo, amiodarone, or an implantable cardioverter defibrillator.
As a result, the five-year mortality rate was lowest in the implantable cardioverter-defibrillator group. So, cardioverter-defibrillators significantly reduced mortality in the group of these patients by 23%. But the effect of Amiodarone was completely unreliable. Moreover, such a positive effect of cardioverter-defibrillators was noted both in ischemic heart failure and also in patients with non-ischemic heart failure: they reduced mortality by 27%. In summary, this study definitively defined the indication as severe systolic dysfunction, regardless of its etiology.
What types of mortality are affected by cardioverters? First of all, of course, on arrhythmic mortality. They reduce the likelihood of death from life-threatening arrhythmias by 61% on average. As a result, cardiac mortality also decreases, because the final outcome of many cardiac accidents is also ventricular fibrillation. Finally, overall mortality also decreases by 31%.
This analysis of the Madit-II study shows who the ideal patient is for cardioverter implantation. This is a patient, regardless of age and gender, but this is a patient with the lowest ejection fraction, and at the same time with the lowest functional class of heart failure. That is, the ideal patient for a cardioverter-defibrillator is a patient who has extremely low left ventricular systolic function, but at the same time a mild clinical picture of heart failure, not terminal - a manifestation of heart failure.
What are the current indications for implantation of cardioverter-defibrillators in patients with heart failure? The first indication is ischemic heart failure with an ejection fraction below 40%. In this case, there is a certain postscript: no earlier than 40 days after myocardial infarction. Where did this addition come from? The Dynamit study was conducted in which cardioverter defibrillators were tried to be implanted in the early stages after myocardial infarction - before the 40th day. These were, again, patients with extremely low ejection fraction. But as a result, it turned out that the mortality rate in both groups - in patients with defibrillators and those without - was not different at all. That is, the tactic of installing defibrillators in the early stages after myocardial infarction did not justify itself.
If we are talking about non-ischemic etiology, non-ischemic heart failure, then this should be an ejection fraction below 35%.
And the third group are patients who are waiting for a heart transplant outside the hospital.
I would like to give one example. This is a 33-year-old young man who had dilated cardiomyopathy. Ejection fraction – 23%, functional class of heart failure – three. This patient did not initially have any arrhythmic indication for a defibrillator. That is, he had only a single ventricular systole; he never had any ventricular tachycardia. A cardioverter-defibrillator was implanted in him in 2005. Please note: 11 months passed before the device worked for the first time. And on the printout obtained from this device, we see the reason for the operation. The patient did experience rapid ventricular tachycardia at a rate of 220 beats per minute. And it was effectively stopped with a single discharge from the cardioverter-defibrillator. Subsequently, this patient was regularly monitored by us. He underwent a heart transplant. And this patient is currently alive.
Let's now turn to what would have happened if this patient had not had at that time, October 2, 2006, a cardioverter-defibrillator - a device that (I would like to emphasize again) was installed prophylactically in a patient who did not have any arrhythmic events.
But there is a group of patients for whom cardioverter implantation is not indicated. These are patients whose life expectancy in the satisfactory functional class is less than one year. The wording is very complex, it must be interpreted as follows. These are patients who have extracardiac pathology, very severe, multi-organ pathology, which does not allow predicting the preservation of quality of life for a long time. That is, these patients are likely to die from non-cardiac pathology.
The second group consists of patients with the fourth functional class of heart failure. Implantation of a cardioverter-defibrillator is not indicated in them due to the fact that these patients die mainly from heart failure, from cardiac accidents, compared to patients from milder functional classes, who die mainly from sudden cardiac death, from life-threatening arrhythmias .
Finally, cardioverter implantation is not indicated for patients if they require myocardial revascularization. This indication, again, was confirmed by a multicenter study. The CABG-PATCH study, which was conducted in the late 90s. It included patients with ischemic heart failure and low ejection fraction. It would seem that patients are suitable for cardioverter implantation. But these patients needed coronary artery bypass grafting. And they were divided into two groups. One group consists of patients with isolated coronary artery bypass grafting, the second group consists of patients who also underwent implantation of a cardioverter during bypass surgery.
As a result, please note: the two-year mortality rate was completely indistinguishable. That is, patients who are indicated for cardiac surgical correction of the disease do not need cardioverter implantation. They need to first correct the cause of severe systolic dysfunction.
Thus, dear colleagues, many doctors believe that cardioverter-defibrillators are always associated with some kind of life-threatening arrhythmias, ventricular tachycardia or sudden death is necessary - this is absolutely not the case. The main candidates for cardioverter implantation are patients at high risk of sudden death. If your patient has an ejection fraction below 40%, especially below 35%, he has a functional class of heart failure from first to third, it is impossible for him to undergo radical cardiac surgery, angioplasty, coronary artery bypass grafting, valve replacement, and so on, then this patient is absolutely implantation of a cardioverter-defibrillator is indicated.
Also, many doctors say: “This is a very expensive approach, it is not for our country. And our domestic patients will never receive a cardioverter-defibrillator.” This is absolutely not true. Let's look at this slide. One of the most important economic criteria is the Number Needed to Treat criterion: how many patients, how many years need to be treated in order to save one year of life for any patient. It turns out that cardioverter-defibrillators are the most convenient, most economically rational approach. They appear to be more cost-effective than ACE inhibitors, beta blockers, statins and amiodarone when it comes to preventing sudden cardiac death.
And we see that even in the United States, where the indications for implantable cardioverters are very expanded, these devices are funded significantly less compared to the huge field of pharmacotherapy for cardiac patients.
Let's look at the structure of indications for implantation of cardioverter-defibrillators. We see that it has changed over the years. In 1998, the largest category of patients with implantable defibrillators were patients who had previously experienced sudden death. Then, in the early 2000s, the largest category of patients were patients with ventricular tachycardia, that is, what is called an arrhythmic indication for implantation of devices. Finally, over the past four years, the largest category of patients has been high-risk patients who have not yet experienced any arrhythmic events.
I would also like to cite the experience of our own institution. This is the structure of our implantable cardioverter defibrillators. We see that only 3% are patients who previously suffered sudden death. A small number of patients with UIQT syndrome and hypertrophic cardiopathy. 34% of patients who have arrhythmic indications have ventricular tachycardia. And the largest number of patients are patients with severe systolic dysfunction.
And in our budget, in the budget of our country, budget funding for these devices is provided. And here is the code for high-tech medical care, which involves implantation of a cardioverter-defibrillator. Thus, any citizen of Russia has the right to receive this device for free. And only in relation to our institution, I would like to cite statistics: 450 new cardioverter-defibrillators are implanted in our clinic alone every year.
Thus, dear colleagues, summing up my speech. If you are seeing a patient with a low ejection fraction for whom radical cardiac surgery is not indicated or is not possible, then it is advisable to refer him to an interventional arrhythmologist. And this patient will be implanted with such a complex, smart device completely free of charge using government funding. Thank you for your attention.
III. Genetic pathology of ion channels
QT prolongation
Long QT syndrome is associated with a high risk of sudden cardiac death. Risk stratification is mainly based on the presence of syncope, Torsades de Pointe (VT) and a history of cardiac arrest. Primary prevention of SCD is generally based on treatment with beta blockers. CD implantation is recommended for secondary prevention, as well as in patients with VT/VF with a history of adequate treatment with beta blockers.
QT prolongation
| Class | I | IIa | IIb |
| Risk stratification | Torsade de pointes/VF/cardiac arrest Syncope Jervell–Lange-Nielsen syndrome QT prolongation | QT greater than 600 ms Development of VT/VF in childhood Prolongation of QT + AV block Macroscopically dynamic T waves Female gender Postpartum period | Family history of SCD Increased QT interval dispersion |
| Primary prevention | Avoid drugs that prolong the QT interval Beta blockers Avoid strenuous exercise | Sympathetic denervation of the LV pacemaker | |
| Secondary prevention | KD + beta blockers + avoid drugs that prolong the QT interval Avoid intense exercise |
ECS - electrical pacemaker
Brugada syndrome
Diagnosis of Brugada syndrome (BS) is based on the presence of spontaneous or inducible ST segment elevation in leads V1-V with or without right bundle branch block (RBBB). Risk stratification is still poorly defined, and the role of EPS in identifying patients with high-risk factors is debated. In survivors of cardiac arrest, CD implantation is recommended. Prophylactic use of KD in high-risk populations is strongly recommended, but this approach is limited by the lack of clearly defined risk criteria.
Brugada syndrome
| Class | I | IIa | IIb |
| Risk stratification | Sustained VT VF | Syncope Family history of SCD | Inducible VT/VF during EPI |
| Primary prevention | CD in patients with syncope/VT | KD in asymptomatic patients with VT induced by EPI | |
| Secondary prevention | KD |
Catecholaminergic polymorphic ventricular tachycardia
To date, there is no precise definition of catecholaminergic polymorphic ventricular tachycardia (CPVT), since large-scale studies are not possible. This disease is associated with a high risk of sudden cardiac death at a young age, but criteria for stratification are lacking. Prevention of sudden cardiac death is based on the use of beta blockers; KDs are recommended for secondary prevention, since the significance of KDs for primary prevention has not been determined.
Catecholaminergic polymorphic ventricular tachycardia
| Class | I | IIa | IIb |
| Risk stratification | VF | Family history of SCD Unsustained VT/syncope in childhood | Syncopations |
| Primary prevention | Beta blockers | KD | |
| Secondary prevention | KD + beta blockers | Beta blockers |
IV. Valve pathology
Aortic stenosis
Among patients whose cause of death is aortic stenosis (AS), about 20% are sudden cardiac death. In the absence of symptoms, the survival rate of patients with AS is high even without valve replacement. The prognostic value of various hemodynamic and electrophysiological studies is limited. Asymptomatic patients with hemodynamically severe aortic stenosis should be under constant observation and, if symptoms develop, undergo immediate surgery. In patients with documented sustained ventricular tachycardia, cardiac implantation should be considered.
Aortic stenosis
| Class | I | IIa | IIb |
| Risk stratification | Syncope Angina | VT, including those induced by EPS Decreased exercise tolerance | Significant stenosis |
| Primary prevention | Surgery | Amiodarone | |
| Secondary prevention | KD |
Mitral valve prolapse
Mitral valve prolapse (MVP) generally has a favorable prognosis; There are suggestions about the risk of sudden cardiac death, but there is no evidence. Most cases of SCD are described in patients who have previously suffered syncope or cardiac arrest, a family history of SCD at a young age, with severe prolapse or myxomatous changes in the mitral valve leaflets. For patients surviving cardiac arrest, CD implantation is recommended.
Mitral valve prolapse
Class
| I | IIa | IIb | |
| Risk stratification | Sustained VT VF | Family history of SCD Severe prolapse or myxomatous changes in the leaflets | QT prolongation Frequent/group ES Inducible VT/VF with EPS Mitral valve regurgitation Late potentials |
| Primary prevention | |||
| Secondary prevention | KD |
Results and discussion
It has been established that in the structure of VS, diseases of the cardiovascular system (CVS) occupy a leading place and account for an average of 74% in Omsk (Table 1).
Table 1. Indicators V.S. for 2005-2014 in Omsk
In Moscow, the average mortality rate from cardiovascular diseases also occupies a leading position and amounts to 79.19% (Table 2).
Table 2. Indicators V.S. for 2005-2014 in Moscow
From the data in table. 1 and 2 it can be seen that over the last decade, diseases of the circulatory system have taken first place among other causes of VS.
Analysis of VS cases by gender revealed a predominance of deaths among males. In the age group under 39 years of age, men accounted for 78% of all cases of VS, while in the age group over 40 years of age these figures were 57% for men and 43% for women, and by the age of 60 years and older, gender differences were almost equal to the predominance of numbers among women (Table 3).
Table 3. Sex and age characteristics of aircraft
The second place in the structure of the armed forces in Omsk is occupied by respiratory diseases - 9% and in Moscow - 6%. Mortality rates for diseases of the gastrointestinal tract are stable throughout the entire period and amount to 4% in both cities. Diseases of the central nervous system account for from 1.2 to 3% in different periods. In both cities, the indicator of BC from cancer pathology attracts attention. It is characterized by progressive growth over 10 years. In Moscow, these indicators increased 2.2 times (Table 4).
Table 4. Indicators V.S. from oncological pathology (according to the BSME of the Moscow Department of Health)
In the group of infectious diseases, one or another form of tuberculosis with complications, in some cases undiagnosed during life, was noted as the main cause of death. As a rule, this cause of VS was observed in a group of people leading an asocial lifestyle, with varying degrees of signs of alimentary cachexia and organ pathology reflecting chronic alcohol intoxication.
Thus, the structure of VS in both cities is characterized by stable mortality rates in the SCD group (74-79%) and an increase in VS from cancer in Moscow.
Of particular interest in forensic medical practice are cases of SCD in young people under the age of 35 years2, which raise controversial issues on the part of relatives, loved ones and law enforcement agencies, due to the lack of any clinical data on intravital medical observation or referral to doctors. With the usual macro- and microscopic examination of the corpses of such persons, pathological changes in the heart and large vessels are practically absent or, as a rule, insignificant.
In the group under 35 years of age, 1914 such cases were selected and studied over a 10-year period. The analysis showed that in this group, men make up 78% (Table 5), whose average age is 32-34 years, i.e., the category of working, economically promising and reproductive age.
Table 5. Indicators V.S. persons in the age group up to 35 years
The frequency of VS in young people from the entire population of deaths ranged from 15 to 15.3%.
During 2005 and 2014, the structure of causes of death in the study group also changed, which made it possible to establish certain patterns (Table 6).
Table 6. Comparative analysis of the causes of SCD among people under 35 years of age
As can be seen from the data in table. 6, the rates of SCD from cardiomyopathy, the form of which is determined by a forensic expert during an autopsy based on morphological signs (dilated, hypertrophic, etc.), have increased significantly. An analysis of all cases in which a diagnosis of cardiomyopathy (CM) was made allowed us to identify a unified approach to the diagnosis of this pathology, reflecting the presence of diagnostic criteria: cardiac hypertrophy (heart weight more than 360 g), expansion of the cavities, flabbiness, dullness of the myocardium, absence of atherosclerotic vascular lesions, valvular pathology, as well as the presence of pathohistological signs: atrophy of cardiomyocytes, their uneven hypertrophy, severe myocardial lipomatosis, lipofuscinosis, myocytolysis, perivascular cardiosclerosis, endocardial fibrosis (Fig. 1). The main terminal symptom complex in cardiomyopathy is arrhythmia, since during life such individuals exhibit a prolonged RR interval, conduction disturbances, and various forms of arrhythmias (ventricular extrasystoles, paroxysmal tachycardias) [21, 22]. In the presence of a provoking factor (physical stress), acute cardiovascular failure with symptoms of pulmonary edema quickly develops. According to BUZ BSME D.Z. Moscow, mortality from cardiomyopathy has increased significantly over the past 10 years. The growth of this pathology may be due to the increased consumption in the group of adolescents (13 years old) and young men under 23 years of age of low-alcohol drinks (beer), the mechanism of damaging action of which is expressed in the disruption of energy and metabolic processes in the myocardium and in the direct toxic effect of cobalt on cardiomyocytes.
Rice. 1. Cardiomyopathy. a — myocardial lipomatosis with dilated cardiomyopathy; b — lipofuscinosis. Hematoxylin and eosin staining.
In the group of young people, 57% of the deceased, especially those under the age of 29, showed external and internal signs of systemic pathology - connective tissue dysplasia (CTD). Data obtained in recent years on the diagnosis of pathological conditions and diseases associated with CTD have made it possible to consider this pathology as one of the risk factors for VS among young people. Many works devoted to an in-depth study of the functional state of the myocardium and central hemodynamics in CTD have made it possible to formulate the statement that the pathology of the cardiovascular system in people with CTD is the main one, and cardiovascular disorders are the leading causes of shortened life of patients [23, 24].
The search for signs of DST allows one to identify the following large and small biological signs during an external examination of a corpse [25]:
1) asthenic type of constitution;
2) tall;
3) flat, narrow, long chest;
4) poor development of the subcutaneous tissue;
5) the presence of pathology of the sternum (funnel-shaped);
6) pathology of the spine (scoliosis, lordosis, combined forms);
7) skin syndrome - the presence of stretch marks, thin, pale, “marbled” skin;
 "blue sclera" syndrome;
"blue sclera" syndrome;
9) fused earlobe;
10) diastema between the first teeth, crowding, irregular tooth growth, Gothic palate;
11) curvature of the lower extremities (X- and O-shaped shins);
12) all types of flat feet (longitudinal, transverse); hallux valgus;
13) the second toe is larger than the first;
14) sandal-shaped gap (between the 1st and 2nd toes)
The presence of 1-2, 3 or more large external signs allows us to consider this pathology as a pre-existing onset of VS, since external signs indicate the presence of DST, which forms cardiovascular syndrome, dysplastic heart syndrome with metabolic disorders, as well as other syndromes: vascular, thoracodiaphragmatic, immunological .
The pathology of the cardiovascular system in persons with CTD is the main one and is diagnosed already during macroscopic examination.
1. Heart: violation of shape, size, position, changes in anatomical and topographic relationships; pathology of cavities and valve apparatus (mitral valve prolapse), endocardium, myocardium, pathology of the conduction system of the heart.
2. Coronary vessels: the presence of aneurysms, pathologically altered course of vessels, tortuosity, abnormal outlet.
3. Pathology of the aorta: hypoplasia, thinning, formation of aneurysms of the arch or ascending section.
4. Pathology of cerebral vessels: malformations, congenital aneurysms, thinning and rupture of the wall, pathological tortuosity, etc.
5. Pathology of the venous section: thrombosis, thrombophlebitis, pulmonary embolism as a cause of death.
According to the literature [4, 5, 26], the immediate causes of death in persons with signs of CTD and the presence of cardiovascular syndrome were massive basal subarachnoid hemorrhages with a breakthrough into the ventricular system of the brain as a result of rupture of congenital aneurysms of the cerebral arteries; pulmonary embolism due to varicose veins; hemorrhagic shock due to rupture of a congenital aneurysm of the thoracic aorta; profuse bleeding caused by rupture of small arteries of internal organs (gastric, esophageal). The main links in the formation of vascular aneurysms in people with DST are a congenital defect of the muscular layer of the vascular wall, damage to the internal elastic membrane, changes in the collagen fibers of blood vessels and hemodynamic disorders that arise in the presence of provoking risk factors: physical activity, psycho-emotional stress, smoking, addiction to weak alcoholic drinks (Fig. 2).
Rice. 2. Rupture of an aneurysm of a vessel at the base of the brain with the development of basal subarachnoid hemorrhage.
Cases of the onset of VS during sports (during training, at competitions, during physical education classes at school or educational institution) in forensic medical practice are the most difficult, since, as a rule, boys or young men aged 16-23 die years, considered practically healthy [27-30]. According to our data, deaths were recorded in sports such as hockey, volleyball, basketball, as well as during exercise in the gym and sports halls. In such cases, sports activity as a psychophysical effort of increased intensity is a causative factor of VS. A.V. Smolensky and B.G. Lyubin [30] proposed to interpret VS in sports as follows: it is death that occurs within an hour from the moment of acute symptoms and coincides in time with sports activity (before the start, during competitions, immediately after the finish) in the absence of external causes, which themselves could have caused their own death. Consequently, the circumstances of death will always indicate the presence of a provoking factor - active physical activity of a sporting nature, and the development of terminal conditions will take place in the presence of witnesses. According to our data, the onset of VS in 42% of young people was detected before the arrival of the ambulance team, in 47% - after the arrival of medical workers and the provision of resuscitation measures, and in 11% death occurred without witnesses.
In our studies, death during physical activity (beginning of training, moment of loading, after loading) was recorded in 23 cases. The provoking factor for the onset of VS in 4 cases was physical activity of a sexual nature, in 7 cases - physical activity associated with lifting weights (lifting weights, transporting furniture, working in a summer cottage, etc.), in 12 cases - active sports (exercises physical education at a university, physical training in a military unit, death in the gym, death at sports competitions). Analysis of all these cases allowed us to consider physical activity as the main provoking factor in the onset of cardiac arrest. In all cases of VS during physical activity, the main pathological changes were identified in the heart, cardiac conduction system, as well as in the coronary vascular bed.
Pathomorphological changes in the heart, as a rule, reflected the main mechanism of SCD—arrhythmogenic. In a number of cases, emergency medical doctors who arrived before the onset of biological death recorded episodes of paroxysmal tachycardia on the ECG, the presence of groups of extrasystoles followed by atrial flutter and fibrillation, which allowed experts to identify and establish the main cause of death. The main types of fatal arrhythmias were ventricular arrhythmias (80% of cases), intraventricular or atrioventricular block. Asystole was much less common (about 20%) and reflected atrioventricular block or sinus node weakness. To date, there are no pathomorphological, biochemical and pathohistological markers that allow diagnosing the arrhythmic genesis of death, which in some cases leads to distortion and substitution of nosological verification of the cause of death in young people.
V. Pathology of the coronary arteries
Anomalous origin of the coronary arteries
SCD most often occurs in patients with an anomalous origin of the trunk of the left coronary artery from the right or non-coronary sinus of Valsalva. Therefore, special attention should be paid to young patients with chest pain similar in description to angina. Surgery is the most appropriate treatment option for patients at high risk of sudden cardiac death.
Anomalous origin of the coronary arteries
| Class | I | IIa | IIb |
| Risk stratification | VF | Young patients with angina or a positive stress test | |
| Primary prevention | Surgery | ||
| Secondary prevention | Surgery |
Myocardial bridges
The long-term prognosis for patients with the presence of myocardial bridges seems favorable, but in some cases this pathology can cause the development of tachyarrhythmias or sudden cardiac death. In symptomatic patients, quantitative coronary angiography, Doppler, and intravascular ultrasound are used to diagnose myocardial bridges. Drug treatment with beta blockers, surgery, angioplasty and coronary artery stenting are alternative treatments.
Myocardial bridges
| Class | I | IIa | IIb |
| Risk stratification | Symptomatic VT VF | Myocardial ischemia | |
| Primary prevention | Surgical treatment in patients with myocardial ischemia | Beta blockers | |
| Secondary prevention | Surgical treatment in patients with myocardial ischemia |
VI. Wolff-Parkinson-White syndrome (WPW)
According to modern research, in patients with WPW syndrome, the incidence of sudden cardiac death is 0.15% per year. The main cause of SCD is the transition of atrial fibrillation with a rapid ventricular response to ventricular fibrillation. Survivors of resuscitation for sudden cardiac death are typically characterized by the absence of symptoms, shortened RR intervals (less than 250 ms) during paroxysmal atrial fibrillation, and the presence of multiple or posteroseptal accessory pathways. Electrophysiological study with atrial excitation and determination of RR intervals between preexcited QRS complexes has high sensitivity, but specificity and significance in determining a positive predictor are limited. In patients at high risk for SCD, catheter ablation is recommended, particularly in those resuscitated from ventricular fibrillation or in patients with symptomatic episodes of atrial fibrillation with a rapid ventricular response.
Wolff-Parkinson-White syndrome
| Class | I | IIa | IIb |
| Risk stratification | less than 250 ms cycle duration in AF less than 270 ms anterograde refractory period of additional pathways Multiple additional pathways | Cessation of pre-excitation during treatment with ajmaline | |
| Primary prevention | Ablation for atrial fibrillation and the presence of rapid conduction through accessory pathways | Ablation in asymptomatic patients with – family history of SCD – athletes | Amiodarone Antiarrhythmic drugs classes Ia and Ic |
| Secondary prevention | Ablation |
VII. Bradyarrhythmias
It has been established that bradyarrhythmias are the cause of sudden cardiac death in 15-20% of cases. Risk factors for bradyarrhythmic death include high-degree AV block with intraventricular conduction disturbances, but in the presence of structural changes in the heart, these factors may predispose to the development of tachyarrhythmias. Pacing is the treatment of choice in high-risk patients with bradyarrhythmia: it relieves symptoms and may reduce mortality.
Risk stratification for cardiac conduction disorders
| Class | I | IIa | IIb |
| Profound AV block | AV block III degree AV block II degree, type II Syncope Combination of heart disease with CHF | ||
| Congenital AV block of the third degree | Syncope QT prolongation Congenital heart disease | ||
| Chronic two- or three-fascicle blockade | Combination of heart disease with CHF | Syncope Conduction from the Hiss bundle to the ventricles 100 ms (HV interval 100 ms) Intraventricular blocks Blocks induced during EPI |
Out-of-hospital resuscitation
Survival after cardiac arrest varies from 5% to 60% depending on the characteristics of the cardiac arrest (ie, cardiac etiology or not; verified or not; ventricular fibrillation or not). The outcome of cardiopulmonary resuscitation (CPR) is influenced not only by the success of its implementation, but also by the patient’s condition before the start of CPR.
It is now generally accepted that time to electrical defibrillation is the single most significant determinant of survival after cardiac arrest.
The instructions for the automatic external defibrillator allow defibrillation in cases of out-of-hospital ventricular fibrillation or ventricular tachycardia to people of non-medical professions, often many minutes before the arrival of the ambulance team. This strategy is known in the West as “first responder defibrillation,” based on the principle of mutual aid.