Transferrin is a protein in the blood plasma that binds iron ions and transports them throughout the body. When your body contains enough transferrin, you can effectively use the iron you get from food. The presence of iron in the body dictates the production of transferrin, but its levels are also affected by inflammation, liver and kidney health. Below in the article we will talk about high and low transferrin levels, and ways to normalize them.
The article is based on the findings of 56 scientific studies
The article quotes the authors:
- Department of Pathology, Children's Hospital Boston, USA
- Fernando Bermejo, Digestive Service, University Hospital of Fuenlabrada, Spain
- University of Utah, USA
- Department of Gastroenterology and Hepatology, Medical University of Wroclaw, Poland
- Medical University and University Hospital of Innsbruck, Austria
- and other authors.
Please note that the numbers in parentheses (1, 2, 3, etc.) are clickable links to peer-reviewed scientific studies. You can follow these links and read the original source of information for the article.
What is transferrin
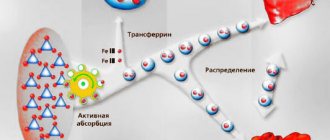
Transferrin is a blood plasma protein that binds iron and transports it throughout the body. It is the main carrier of iron in the blood. If you have enough transferrin, then your body can effectively use the iron you get from your diet. [, ]
The characteristic patterns of changes that occur in the blood plasma through the concentration of certain acute phase proteins after moderate inflammation are shown. Pay attention to the duration of fibrinogen production (simultaneous increase in ESR).
Transferrin levels increase with increasing iron deficiency. When iron is low, your body will try to compensate by increasing the amount of transferrin to increase the availability of iron in tissues. [] On the other hand, the amount of transferrin decreases with increasing iron content. [, ]
Acute phase reaction. The inflammatory stimulus leads to the activation of monocytes and macrophages, which release cytokines. Cytokines act on the liver to stimulate the production of acute phase proteins. Cytokines, together with acute phase proteins, produce a systemic response with neuroendocrine, metabolic, hematological and biochemical changes. (www.researchgate.net)
Transferrin protein is produced in the liver, so its levels are also associated with overall health and general inflammation in the liver and in the body as a whole. Transferrin is a negative acute phase protein. This means that as inflammation increases, and as the liver produces more inflammatory proteins (eg, C-reactive protein , ferritin), transferrin production decreases. [,]
Scheme of iron homeostasis (iron metabolism). The central part of the figure depicts the entry of iron into the body (via the small intestine), its attachment to transferrin (TF), movement to the main site of disposal (erythroid bone marrow), attachment to circulating red blood cells, to tissue macrophages, which phagocytize red blood cells and recycle iron levels to spleen, movement for storage in hepatocytes. (www.researchgate)
Interpretation of results/Information for specialists
NEGATIVE RESULT
Hemoglobin and haptohemoglobin complex – NOT DETECTED
Absence of hemoglobin and haptohemoglobin complex in the stool sample is normal
A false negative result is also possible against the background of an occasionally bleeding polyp (neoplasm) and in the absence of bleeding at the moment.
IMPORTANT: a negative test result does not completely exclude intestinal pathology, for example, in the case of episodic bleeding of a polyp. In this case, it is possible to recommend repeated examinations (at least three times) at intervals determined by the attending physician, and to use instrumental diagnostic methods for final verification of the diagnosis.
Normal transferrin level
The unit of measurement for transferrin when taking tests is g/l.
Transferrin reference values (normal range)
Age, gender | Transferrin, g/l |
| up to 2 months | 0,99 – 2,18 |
| 1 month – 1 year | 1,02 – 3,17 |
| 1 – 14 years | 2,14 – 3,30 |
| >14 years old | 2,0 – 3,6 |
| Pregnant women 1st trimester | 2,54 – 3,44 |
| II trimester | 2,2 – 4,41 |
| III trimester | 2,88 – 5,3 |
Serum transferrin concentrations are approximately 10% higher in women than in men. A high concentration of transferrin in the blood serum is observed during pregnancy (especially in the third trimester) and when using estrogens.
Transferrin test
A study of the level of transferrin in the blood is necessary for a more detailed study of iron metabolism in the body. This in-depth consideration is necessary to:
- iron metabolism assessments (along with iron testing) to determine how much iron the blood carries
- estimates of iron stores in the body
- identifying the cause of anemia - iron deficiency, chronic diseases or vitamin B12 deficiency
- liver health assessments.
Transferrin saturation coefficient (TSR)
After the synthesis of transferrin in the liver, it is saturated with iron. This saturation depends on the level of iron in the body, which comes with food. The main location of transferrin is the mucous membrane , where this protein captures iron ions from food and prevents harmful microorganisms from also using the iron. With a lack of iron, pathogens on the mucous membranes are inhibited, which allows a very small list of bacteria to multiply. In addition to iron, transferrin is capable of binding cobalt and zinc.
The transferrin saturation coefficient (TSC) is the ratio of iron bound in transferrin (iron in serum) to the total iron binding capacity (TIBC) or total transferrin, measured as a percentage.
KNT = iron / OZhSS * 100
Normal CST values for adults are: 15-50%
High values of CST (transferrin saturation coefficient) are determined with increased iron content in the body and are inherent in the following conditions: megaloblastic anemia, sideroblastic anemia, hemochromatosis. A decrease in CST indicates the following possible problems in the body: iron deficiency anemia, chronic infections, malignant tumors, tissue inflammation, uremia and nephrotic syndrome.
Complexes with this research
Male check-up No. 1 39 studies for annual preventive examination 10,930 ₽ Composition
Blood biochemistry. 19 indicators Advanced biochemical blood test 3,420 ₽ Composition
Causes of hair loss RUB 1,840 Composition
IN OTHER COMPLEXES
- Examination during pregnancy. 3rd trimester 5,360 RUR
- Women's check-up No. 1 RUB 11,530
- Examination during pregnancy. 1st trimester 9,770 RUR
- Joining IVF RUB 14,350
- Female infertility RUB 9,310
High transferrin levels
Causes of elevated transferrin levels:
- The most common cause of elevated transferrin is iron deficiency anemia. [,, ]
- Pregnancy, especially its third trimester. Normal condition.
- Birth control pills. In a study of 117 women who took birth control pills (oral contraceptives) for at least 2 years, transferrin levels were higher than in women who had never taken them. []
- Obtaining a significant amount of fluorides (fluorine compounds).
Ways to reduce transferrin
Eating foods high in iron can help prevent iron deficiency. Iron-rich foods include red meat, liver, poultry and fish. []
Iron supplements will iron intake, but should only be taken if your iron deficiency cannot be corrected through diet. [, , ]
Reduce consumption of drinks such as coffee , cocoa , green and herbal tea , as they reduce the absorption of iron from food. [, , , , , ] Or postpone their consumption 1-2 hours before meals. alcohol consumption , which completely destroys heme iron in animal foods, but not in plant foods. []
Vitamin C increases iron absorption []. It is a good practice to add sources of vitamin C to iron-rich foods (dried rose hips, lemon juice, sauerkraut, etc.).
FOOD RICH IN IRON AND FOODS WITH VITAMIN C TO IMPROVE IRON ABSORPTION
It is worth noting that night shift work disrupts circadian rhythms and there is a disagreement between the “internal clocks” in the liver and brain. If, in the evening or at night, you eat food that contains a lot of iron (for example, sausage, hamburger, steak), then an even greater mismatch occurs between the circadian rhythms in the liver cells and in the brain. This disorder increases the risk of developing type 2 diabetes. []
Heme and non-heme iron
Heme is part of hemoglobin, myoglobin, and some enzymes (cytochromes, catalase, lactoperoxidase). The iron included in these compounds is commonly called heme iron .
Heme iron is much better absorbed by the body.
SOME FOOD PRODUCTS ARE SOURCES OF HEME AND NON-HEME IRON
Iron compounds found in plant foods are classified as non-heme iron . It is much less absorbed than heme iron, and its absorption is influenced by many additional factors.
Substances that reduce iron absorption
- Solubility of various non-heme iron compounds
- Integrity of the intestinal mucosa (healthy intestines absorb better)
- polyphenols in food – grains, vegetables, spices and drinks
- Calcium (cow's milk, calcium supplements)
- Phytic acid – bran, wheat, rice, legumes, nuts (can reduce absorption by 50-60%).
- Zinc supplements . It is better to take separately from food.
- Oxalic acid – found in spinach, cabbage, beets, nuts, chocolate and tea. Reduces the absorption of heme iron.
- Eggs contain a compound called phosvitin, which impairs iron absorption. One boiled egg can reduce the absorption of iron in food by 28%.
Substances that increase iron absorption
- Vitamin C – can increase absorption 4 times
- Beta-carotene – increases absorption and reduces the effect of phytic acid and tannins.
- Betaine hydrochloride is an acid that is present in the stomach and it helps with the breakdown of food and absorption of nutrients.
Table of examples of iron absorption from various foods
| Iron-rich foods | Iron type | Suction |
| Veal, beef | Heme | 22-25% |
| Fish, kidneys, liver | Heme | 11% |
| Eggs | Heme | 3% |
| Soya beans | Non-heme | 7% |
| Apples, pomegranates, buckwheat | Non-heme | 3% |
| Rice, spinach | Non-heme | 1% |
Preparing for the study
The stool is collected in a sterile, disposable container. When preparing a patient for the study, alcohol and NSAID drugs (non-steroidal anti-inflammatory drugs - ortofen, indomethacin, etc.) acetylsalicylic acid, warfarin (and other anicoagulants), corticosteroid drugs reserpine, phenylbutazone should be discontinued 2 days in advance.
To obtain reliable results, samples should not be used in patients during menstruation, as well as during rectal bleeding due to hemorrhoids or constipation.
You cannot examine stool obtained after an enema and taking laxatives, as well as X-ray examination of the stomach and intestines using contrast agents.
Decreased transferrin levels
Iron overload
The most common cause of low transferrin is iron overload (excess iron). [, ]
Protein food deficiency
To produce proteins, the liver needs resources. To do this, the liver requires amino acids, which you get from your diet. When there is not enough protein in your diet, then your liver cannot produce enough transferrin. []
In studies of over 80 children who were malnourished, transferrin levels were significantly reduced. [, ]
Inflammation
As mentioned above, transferrin is a negative acute phase protein. When the liver increases the production of proteins associated with inflammation (eg, C-reactive protein , ferritin), there is a decrease in transferrin production. [,] A number of diseases, such as infections and cancer , which are characterized by an inflammatory process, can reduce transferrin levels. []
PATHOPHYSIOLOGICAL MECHANISMS OF CHRONIC ANEMIA WITH INFLAMMATION (www.scielo.br) The anti-inflammatory cytokine IL-10 regulates the expression of the transferrin receptor, enhancing its binding to iron, mediated by the monocyte transferrin receptor.
An observational study of 297 patients with active inflammatory bowel diseases ( Crohn's disease and ulcerative colitis ) found significantly lower transferrin levels. Increased disease activity and inflammation were associated with decreased transferrin levels. []
Another similar study compared 20 patients with chronic periodontitis (gum inflammation) and 20 healthy people. It has been found that people with chronic gum disease have lower levels of transferrin. Three months after treatment of inflammation, the level of transferrin in the blood increased to the values that were in healthy people. []
Preeclampsia , a condition that causes high blood pressure during pregnancy, is associated with inflammation. Women with preeclampsia often show decreased transferrin values. [, ]
Other chronic diseases leading to an increase in inflammation and a decrease in transferrin: systemic lupus erythematosus, rheumatoid arthritis , tuberculosis, bacterial endocarditis.
Liver disease
In liver disease, this organ cannot effectively produce transferrin. [] This happens when liver function is impaired by inflammation or alcohol consumption. []
Patients with liver disease , including cirrhosis, have significantly lower transferrin levels than healthy people. [, ]
Kidney disease
Nephrotic syndrome is a kidney disorder that causes too much protein to be excreted in the urine. Transferrin is one of the proteins that is excreted from the body in urine. This is why nephrotic syndrome, especially in diabetes, can exhibit significant transferrin losses. [, ] Glomerulonephritis is another inflammatory kidney disease, possibly autoimmune, leading to a decrease in transferrin values.
Genetic predisposition
Transferrin may be low due to genetic reasons. In these cases, transferrin values were in the range of 10-20 mg/dL. [, ]
Other reasons for decreased transferrin levels
- Use of corticosteroids and testosterone
- Thalassemia
- Hereditary hemochromatosis
- Loss of protein in burns
- Malabsorption syndrome
- Serum hemolysis
Other abilities of the transport protein
Transferrin, having the ability to combine with ferric ions, not only delivers this metal to organs and tissues in reserve (ferritin) or to the bone marrow to participate in erythropoiesis (synthesis of the red blood pigment, hemoglobin, in new red blood cells) :
- He “knows how to recognize” reticulocytes (young red blood cells), which are engaged in the synthesis of hemoglobin.
- An important task of transferrin is to pick up ferric iron ions released after the breakdown of red blood cells (and, accordingly, the hemoglobin contained in them), which in a free state pose a danger to the body due to their high toxicity.
- Transferrin, being part of the β-globulin fraction, belongs to the acute phase proteins. It takes part in ensuring the immune response programmed from birth. The main place of permanent residence of transferrin is the mucous membrane, where it, “looking for” and binding iron, makes it impossible for pathogenic microorganisms that get there to use it and thereby creates conditions for them that are unacceptable for life.
- The ability of transferrin to bind metals is not very useful when plutonium enters the body, which the transport protein binds instead of iron and carries it “in reserve” to the bones.
The main producers of transferrin in the body are the liver and brain.
The gene responsible for the production of the “vehicle” for ferrum is located on the third chromosome. A severe deficiency (to the point of complete absence) of transport protein is a severe, but, fortunately, rare hereditary pathology (autosomal recessive path), accompanied by severe hypochromic anemia and called atransferrinemia.
Ways to increase transferrin levels
In order to increase your transferrin levels, you must make sure that your blood does not contain large amounts of iron. An iron blood test will help you answer this question.
DISTRIBUTION OF IRON IN THE BODY OF AN ADULT.
Circulating iron binds to transferrin and is delivered to tissues (black arrows) (openi.nlm.nih.gov)
Reduce iron intake from food
If your transferrin levels are low due to high iron intake:
- Avoid iron-rich foods such as red meat, fish and poultry. []
- Eat more foods that reduce iron absorption, such as fiber and phytic acid (from whole grains) and chili peppers. [, ]
- Drink more coffee, cocoa, green tea and other herbal teas such as chamomile, linden, mint and verbena teas. All of them reduce the absorption of iron from food. [, , , , , ]