Modern antiplatelet therapy: place of ticagrelor in clinical guidelines
The leading cause of mortality worldwide is still cardiovascular pathology, despite the high level of development of cardiology over the past decades [1, 2]. The various clinical manifestations of vascular pathology are based on a common anatomical substrate in the form of dysfunction of the arterial endothelium, chronic inflammation and damage to the cap of the atherosclerotic plaque, slowing of blood flow, and the formation of an intravascular thrombus [3]. In this regard, reducing the risk of developing thrombotic complications is the main task that a doctor who wants to increase the duration and improve the quality of life of patients with cardiovascular diseases should set.
The pathogenesis of thrombosis includes three main points for drug action: platelet link - the action of antiplatelet agents, the coagulation system - the zone of action of anticoagulants, fibrin - the action of fibrinolytics. Platelets are the first to respond to the rupture of an atherosclerotic plaque, launching a coagulation cascade; they are a source of active synthesis of humoral factors that simultaneously stimulate the processes of thrombus formation and inflammation. According to a meta-analysis of 287 randomized studies on secondary prevention and 6 studies on primary prevention, the use of antiplatelet therapy can reduce the risk of non-fatal myocardial infarction and non-fatal cerebral infarction by 23% [4]. This meta-analysis confirms that the leading role in the prevention of complications of atherosclerosis should be given to antiplatelet agents.
Antiplatelet agents are medications that prevent thrombosis by reducing the functional activity of platelets. To date, more than 20 different drugs are known that can inhibit platelet function through various mechanisms of action. However, during many years of practice and clinical studies, effectiveness was confirmed only for cyclooxygenase inhibitors (acetylsalicylic acid), adenosine diphosphate (ADP) receptor blockers - P2Y12 (clopidogrel, prasugrel, ticagrelor), phosphodiesterase inhibitors (dipyridamole) and glycoprotein IIb-IIIa antagonists for intravenous use (abciximab, tirofiban, eptifibatide). Activation of platelets and their subsequent aggregation occur under the influence of various mediators, the most important of which are thromboxane A2 and ADP, therefore acetylsalicylic acid (ASA) and ADP inhibitors (clopidogrel, prasugrel, ticagrelor) are most widely used.
The history of the creation of the class began with the discovery of the antiplatelet properties of ASA. In 1987, the first randomized Canadian trial was published involving 585 stroke patients treated with ASA for 26 months. The study demonstrated the effectiveness of ASA against recurrent stroke [5]. This was the reason that in 1980, the US Food and Drug Administration (FDA) approved ASA for the treatment of patients after stroke. Subsequently, the effectiveness of ASA in reducing the risk of death and recurrent myocardial infarction in patients with unstable angina and non-ST segment elevation myocardial infarction was proven [4]. Thus began the era of antiplatelet therapy and its first worthy representative - acetylsalicylic acid.
Acetylsalicylic acid blocks platelet activation by inhibiting cyclooxygenase (COX), preventing the formation of thromboxane A2. Platelets are anucleate cells, so they lack the ability to synthesize proteins. Irreversible inhibition of COX-1, the impossibility of its resynthesis due to the absence of a nucleus, as well as the daily renewal of the platelet pool by only 10% lead to the fact that the blockade of thromboxane synthesis during ASA therapy persists throughout the platelet life span, up to 10 days. Complete suppression of thromboxane production is achieved with constant long-term administration of ASA in doses ≥ 75 mg/day. In most patients with stable coronary heart disease (CHD), low-dose ASA is preferable due to its favorable benefit-risk ratio. ASA for this category of patients remains the basis of drug prevention of arterial thrombosis [6]. The damaging effect of ASA on the gastrointestinal tract (GIT) increases as the dose increases. The drug is recommended for all patients with an established diagnosis of coronary artery disease without any restrictions on the duration of use. The optimal benefit-risk ratio is achieved when using ASA in a dose range from 75 to 150 mg/day; when used as part of dual antiplatelet therapy, the dose is 75–100 mg.
However, in recent years, the problem of resistance to ASA therapy has been actively discussed, which is understood as the inability of the drug in some patients to adequately suppress platelet function, reduce the synthesis of thromboxane A2 and/or prolong bleeding time. The prevalence of resistance to ASA therapy, according to various studies, ranges from 10% to 45% [7]. Among the possible reasons for this phenomenon are the following:
- pharmacodynamic interactions of ASA with non-steroidal anti-inflammatory drugs (NSAIDs);
- the presence of non-platelet sources of thromboxane A2 synthesis;
- expression of COX-2 in newly formed platelets;
- hydrolysis of ASA by esterases of the gastrointestinal mucosa;
- increased synthesis of thromboxane A2;
- hyperlipidemia;
- genetic features.
A number of independent studies have found that in patients with acute coronary syndrome (ACS) without ST segment elevation (ESSENCE, PRISM PLUS), the immediate prognosis depends on previous use of ASA before the development of exacerbation of coronary artery disease. Thus, in the PRISM PLUS study, when using ASA for ACS, the incidence of myocardial infarction, refractory angina and sudden death by the 7th day of observation was 12.1% among patients who had not previously taken ASA, and 23.5% among those taking ASA before the development of an exacerbation. This fact was called the “aspirin paradox,” which led DL Bhatt and EJ Topol (2004) to classify ASA as “suboptimal antiplatelet drugs” [8, 9]. All this contributed to the development and study of new antiplatelet drugs - ADP P2Y12 receptor inhibitors and the identification of approaches to dual antiplatelet therapy.
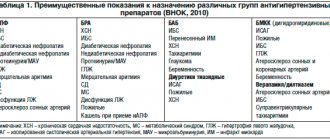
The group of ADP-P2Y12 receptor blockers includes the drugs ticlopidine, clopidogrel, prasugrel, and ticaglerol. These drugs inhibit platelet aggregation induced by adenosine diphosphate by causing changes in the platelet ADP receptor, which is called P2Y12 [9]. There are significant differences between the drugs listed above, for example, irreversible inhibitors of P2Y12 receptors include thienopyridines (ticlopidine, clopidogrel and prasugrel), and reversible inhibitors include triazolopyridines (ticagrelor). Comparative characteristics of the drugs are presented in table. 1.
Clopidogrel is the most well-known and actively used antiplatelet agent after ASA in domestic medicine today [10]. The results of large clinical trials have proven the effectiveness of reducing the incidence of complications in a wide range of patients with coronary artery disease when adding clopidogrel to ASA [11, 12], which served as the basis for the development of indications for dual antiplatelet therapy in patients with ACS without ST elevation, as well as after coronary artery bypass grafting (CABG) and percutaneous coronary intervention (PCI) for the prevention of thrombosis [13].
Clopidogrel, as can be seen from the table, is a prodrug; the drug has a complex metabolism. The absorption of clopidogrel in the intestine is controlled by a special protein (P-glycoprotein), encoded by the ABCB1 gene, in this regard, only about 15% of the absorbed clopidogrel in the liver is converted into an active metabolite. The process is two-step (oxidation and hydrolysis), depending on several isoenzymes of the cytochrome P450 system, the most important of which are CYP2C19 and CYP3A4 [14]. Despite the wide evidence base for the effectiveness of this drug, clopidogrel has a number of disadvantages, which include a delayed antiplatelet effect, since it is a prodrug and requires time to activate; maximum suppression of ADP receptors occurs only on the 4th–5th day of regular use. In addition, there is variability in the antithrombotic effect of clopidogrel in different patients, which may be due to a number of pharmacokinetic factors, including insufficient loading and maintenance doses of the drug, impaired absorption and formation of the active metabolite, drug interactions, in particular with proton pump inhibitors, which are often prescribed for the prevention of bleeding from the upper gastrointestinal tract [15, 16].
Due to the existing shortcomings of clopidogrel and the inability to solve this problem, the need to create a new drug from the group of ADP receptor blockers - P2Y12 - became obvious to the world community.
A new antiplatelet drug is ticagrelor, a direct-acting reversible antagonist of P2Y12 receptors. The drug is an active substance that is metabolized via the CYP3A4 isoenzyme to form an active metabolite. The degree of inhibition of P2Y12 receptors is determined primarily by the plasma levels of ticagrelor and, to a lesser extent, its active metabolite. The half-life is about 12 hours, and therefore the drug is prescribed twice a day. Ticagrelor has a faster onset of therapeutic action and provides a more pronounced and persistent inhibition of platelet activation compared to clopidogrel. At the same time, recovery of platelet function after discontinuation of ticagrelor occurs faster compared to clopidogrel. The presence of more attractive pharmacological properties, as well as existing problems associated with taking clopidogrel, were the main reasons for organizing the large-scale PLATO (Platelet inhibition and patient outcomes) study, which compared the effectiveness and safety of ticagrelor compared with clopidogrel in patients with ACS [17] . According to a study published on August 30, 2009 at the Congress of the European Society of Cardiology (ESC), the new antithrombotic drug ticagrelor is more effective than clopidogrel in treating patients with acute coronary syndrome and does not increase the risk of bleeding.
Researchers led by Lars Wallentin randomized 18,624 patients with ACS hospitalized between 2006 and 2008 at 862 hospitals included in the PLATO trial. Patients were divided into 2 groups: in the first group, patients received ticagrelor (180 mg loading dose and 90 mg twice a day), in the other - clopidogrel (300 or 600 mg loading dose and 75 mg daily). All patients also took ASA at a dose of 75–100 mg. The groups were carefully balanced taking into account baseline clinical parameters, concomitant diseases and treatment tactics. 37.5% of patients had acute myocardial infarction with ST segment elevation, 42.9% had acute myocardial infarction without ST segment elevation, and 16.6% had unstable angina. The duration of medication use ranged from 6 to 12 months, with an average of 277 days. The results showed that with ticagrelor compared with clopidogrel there was a significant reduction in the total number of primary endpoints (cardiovascular death, myocardial infarction or stroke): 9.8% versus 11.7%, a risk reduction of 16%, p < 0.001. In those receiving ticagrelor, compared with those treated with clopidogrel, there was a significant decrease in the incidence of myocardial infarction: from 6.9% to 5.8%, and cardiovascular death - from 5.1% to 4%. At the same time, the total number of strokes was the same in both subgroups: 1.5% and 1.3%. The incidence of the combined secondary endpoint (death from vascular causes, myocardial infarction, stroke, recurrent myocardial ischemia, transient ischemic attack or other types of arterial thrombosis), as well as death from all causes, was significantly lower in the ticagrelor group compared with clopidogrel: 14.6 % versus 16.7% and 4.5% versus 5.9%, respectively. There were no significant differences between the groups in the incidence of major bleeding or fatal or life-threatening bleeding. It is interesting to note that the risk of major bleeding, including fatal intracranial bleeding not related to the CABG procedure, was slightly higher in the ticagrelor group compared with clopidogrel (4.5% vs. 3.8%, p = 0.03). However, the incidence of CABG-related bleeding was lower among those receiving ticagrelor (7.4% vs. 7.9%) [18].
The results of 13,408 (72%) patients with an invasive treatment strategy planned at the randomization stage were analyzed separately [18]. 49.1% of patients were diagnosed with acute coronary syndrome with ST segment elevation on electrocardiography (ECG) and 50.9% with acute coronary syndrome without ST segment elevation on ECG. During the first hospitalization, PCI was performed in 10,298 (72%) patients and CABG in 782 (5.8%). The average time to PCI was 2.4 (0.8–20.1) hours after randomization in patients with ACS without ST segment elevation on the ECG and 0.5 (0.2–1) hours in patients with ACS with ST segment elevation on the ECG . The median time to CABG was 6 (3–10) days. The total number of myocardial infarctions, strokes and cardiovascular deaths during therapy with ticagrelor decreased to 9% (clopidogrel - by 10.7%), i.e., the risk reduction was 16%, p < 0.0025.
It is important to emphasize that the benefit of ticagrelor on the primary endpoint was observed in different subgroups and was independent of the loading dose of clopidogrel. Major bleeding was equally common in those treated with ticagrelor and those treated with clopidogrel (11.6% vs. 11.5%). The incidence of stent thrombosis was significantly lower in the ticagrelor group, both with and without drug-eluting stents. The incidence of certain stent thrombosis in patients receiving ticagrelor was significantly lower at both 30 days and 360 days of follow-up compared with those treated with clopidogrel, including those patients taking a loading dose of 600 mg or more.
In a substudy analysis of 1,261 patients undergoing CABG within 7 days of the last study drug dose, there was no significant difference in the reduction in primary endpoints (10.6% in the ticagrelor group and 13.1% in the clopidogrel group). Moreover, among those taking ticagrelor, there was a significant decrease in overall mortality by 51%, and cardiovascular mortality by 48%, both in the early and late periods after surgery [19].
Thus, PLATO was the first large-scale study to demonstrate the clinical effectiveness of ticagrelor in reducing the incidence of major vascular events in patients with ACS, without a significant increase in the risk of bleeding. A more significant reduction in the risk of thrombotic episodes during therapy with ticagrelor appears to be due to more rapid and intense inhibition of platelet P2Y12 receptors. When a loading dose of 600 mg of clopidogrel is administered, it takes 2–4 hours to achieve 50% inhibition of platelet aggregation, and the same effect is achieved after 30 minutes when taking 180 mg of ticagrelor. In addition, there is a fairly large group of patients with the presence of defective variants of alleles of the cytochrome P450 system, which is associated with a slowdown in the formation of the active metabolite of clopidogrel, insufficient suppression of platelet function when taking it, as well as with a higher risk of cardiovascular complications after acute coronary syndrome and during PCI. The advantages of ticagrelor also include the reversible nature of inhibition of platelet P2Y12 receptors, which means a more rapid cessation of the antiplatelet effect after discontinuation of the drug. This circumstance seems important during invasive interventions, as well as before the upcoming CABG procedure. Although the incidence of major bleeding was no lower with ticagrelor than with clopidogrel, it should be noted that the greater inhibition of platelet function was not associated with an increase in the incidence of major bleeding. This distinguishes ticagrelor from prasugrel, whose more pronounced antiplatelet effect is accompanied by an increased risk of major bleeding.
The European Society of Cardiology recommended the use of ticagrelor (at a loading dose of 180 mg and 90 mg 2 times a day as a maintenance dose) to all patients with ACS, regardless of the planned treatment strategy (invasive or conservative) as first-line therapy. If patients received clopidogrel at the very beginning of the disease, it should be replaced with ticagrelor. Taking clopidogrel in patients with ACS with invasive or conservative strategies is possible only in cases of absence or intolerance to ticagrelor or prasugrel. The duration of therapy with P2Y12 receptor inhibitors in patients who have suffered acute coronary syndrome is 12 months. In patients on therapy with P2Y12 receptor inhibitors, in cases of planned surgery (including CABG), ticagrelor and clopidogrel are discontinued 5 days before, and prasugrel 7 days before. Dual antiplatelet therapy is mandatory while taking ASA at a dose of 75–100 mg/day [13]. The use of dual antiplatelet therapy in stable coronary artery disease could provide more effective prevention of coronary thrombosis. However, in the CHARISMA study, which included stable patients with atherosclerotic lesions of various vascular territories or multiple cardiovascular risk factors, the addition of clopidogrel to ASA did not bring additional benefit [20]. The 2013 European Society of Cardiology guidelines indicate that dual antiplatelet therapy is beneficial only in certain categories of patients at high risk of ischemic events. Routine administration of this therapy to patients with stable coronary artery disease is not recommended [21].
Thus, atherothrombosis is the cause of high mortality in patients with cardiovascular diseases throughout the world. One of the key points of therapy is the competent prescription of antiplatelet drugs. The main effective oral drugs prescribed in clinical practice are ASA, clopidogrel, ticagrelor, prasugrel. In table Figure 2 presents an algorithm for selecting antiplatelet agents. Modern cardiology is actively developing, and one can hope that new facets of known drugs and the development of new ones will help doctors in the daily fight against cardiovascular diseases.
Literature
- Singh, VV, Toskes PP Small Bowel Bacterial Overgrowth: Presentation, Diagnosis, and Treatment // Curr Treat Options Gastroenterol. 2004. Vol. 7(1). R. 19–28.
- McMurray JJ, Adamopoulos S, Anker SD et al. Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology // Eur. Heart J. 2012. Vol. 33 (14). P. 1787–1847.
- Uster V., Fallon JT, Badimon JJ et al. The unstable atherosclerotic plaque: clinical significance and therapeutic intervention // Thrombosis and Hemostasis. 1997. Vol. 78(1). P. 247–255.
- Antithrombotic Trialists' Collaboration. Collaborative meta-analysis of randomized trials of antiplatelet therapy for prevention of death, myocardial infarction? And stroke in high-risk patients // BMJ. 2002. Vol. 324. P. 71–86.
- A randomized trial of aspirin and sulfinpyrazone in threatened stroke. The Canadian Cooperative Study Group // N. Engl. J. Med. 1978. Vol. 299(2). P. 53–59.
- ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the Diagnosis and Management of Patients With Stable Ischemic Heart Disease: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines // Circulation. 2012. Vol. 126. P. 354–471.
- Ushkalova E. A. Aspirin resistance: mechanisms of development, methods of determination and clinical significance // Farmateka. 2006. No. 13 (128). pp. 35–41.
- Ainetdinova D. Kh., Udovichenko A. E., Sulimov V. A. The role of antiplatelet therapy in the primary and secondary prevention of cardiovascular diseases // Effective pharmacotherapy in cardiology and angiology. 2007. No. 2. pp. 36–41.
- Shalaev S.V. Antiplatelet agents in the treatment of acute coronary syndromes // Pharmateka. 2003. No. 312. pp. 94–97.
- Kei A.A., Florentin M. et al. Antiplatelet Drugs: What comes next? // Clin. Applied Thrombosis // Hemostasis. 2011. Vol. 17(1). P. 9–26.
- Patrono C., Baigent C., Hirsh J. On behalf of the American College of Chest Physicians. Antiplatelet drugs: American College of Chest Physicians evidence-based clinical practice guidelines (8 th edition) // Chest 2008. Vol. 133(6). P. 1995–2335.
- Steg G., James SK, Atar D. et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation The Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC) // European Heart Journal. 2012. Vol. 33. R. 2569–2619.
- ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST segment elevation. The Task Force for the management of acute coronary syndromes in patients presenting without persistent ST segment elevation of the European Society of Cardiology // Eur. Heart J. 2011. Vol. 32. P. 2999–3054.
- Cattaneo M. ADP receptors antagonists. In Michelson AD, ed Platelets. San Diego, Calif.: Academic Press. 2006. P. 1127–1144.
- Snoep JD, Hovens MM Clopidogrel nonresponsiveness in patients under-going percutaneous coronary intervention with stenting: a systematic review and meta-analysis // Am. Heart J. 2007. Vol. 154. P. 221–231.
- Norgard NB, Mathews KD, Wall GC Drug-drug interaction between clopidogrel and the proton pump inhibitors // Ann. Pharmacother. 2009. Vol. 43. P. 1266–1274.
- Wallentin L., Becker RC, Budaj A. et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes // N. Engl. J. Med. 2009. Vol. 361. P. 1045–1057.
- Cannon CP, Harrington RA, James S. et al. Comparison of ticagrelor with clopidogrel in patients with a planned invasive strategy for acute coronary syndromes (PLATO): a randomized double–blind study // Lancet. 2010. Vol. 375 (9711). P. 283–293.
- Held C., Asenblad N., Bassand JP et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes undergoing coronary artery bypass surgery, results from the PLATO // J. Amer. Coll. Cardiol. 2011. Vol 57. P. 672–684.
- Bhatt DL, Flather MD, Hacke W. et al. Patients with prior myocardial infarction, stroke, or symptomatic peripheral arterial disease in the CHARISMA trial // J. Am. Coll. Cardiol. 2007. Vol. 49. P. 1982–1988.
- ESC guidelines on the management of stable coronary artery disease. The Task Force on the management of stable coronary artery disease of the European Society of Cardiology // Eur. Heart J. 2013. Vol. 38. P. 2949–3003.
G. I. Nechaeva1, Doctor of Medical Sciences, Professor O. V. Drokina, Candidate of Medical Sciences N. I. Fisun, Candidate of Medical Sciences
State Budgetary Educational Institution of Higher Professional Education Omsk State Medical Academy of the Ministry of Health of the Russian Federation, Omsk
1 Contact information
* The drug is not registered in the Russian Federation.
Physiology of hemostasis
There are cellular and plasma coagulation factors. Cellular factors include platelets, and plasma factors include proteins and enzymes involved in the process of blood coagulation. Plasma coagulation factors are synthesized in the liver and circulate in the blood in an inactive form.
Stopping bleeding occurs in 3 stages and involves both blood vessels and platelets, and plasma coagulation factors:
- Temporary (primary) vasospasm (VascularPhase).
- Formation of an unstable, loose platelet plug due to platelet adhesion and aggregation (PlateletPhase).
- Retraction (contraction and compaction) of the platelet plug due to fibrin threads (CoagulationPhase).
Anticoagulants (drugs that disrupt secondary hemostasis)
Warfarin
In addition to antiplatelet agents, the process of thrombus formation can be influenced by anticoagulants - drugs that prevent the activation of plasma coagulation factors. Studies performed before the widespread introduction of anticoagulant therapy demonstrated a high incidence of thrombus formation (up to 50%) in the left ventricular cavity in the post-infarction period [5]. The cause of blood clots is not the activation of platelets, but a local violation of myocardial contractility (violation of the rheological properties of blood), which in turn activates plasma coagulation factors. In simple words, platelets have nothing to do with it, and antiplatelet agents will not help. Indications for anticoagulant therapy: prevention of arterial and venous embolism of cardiogenic origin in patients with atrial fibrillation, after heart valve replacement, after extensive transmural MI in patients with parietal thrombosis of the left ventricle, etc.
Vitamin K plays an important role in the production of many plasma coagulation factors. Warfarin blocks the synthesis of vitamin K-dependent blood coagulation factors in the liver, namely factors II, VII, IX and X. The concentration of these components in the blood decreases and the clotting process slows down.
Warfarin has a narrow therapeutic window and requires individual dose selection. It is quite difficult to maintain optimal levels of the drug in the blood during long-term outpatient treatment. It interacts with many medications. A large group of pharmacological drugs can enhance or weaken the effect of Warfarin. The interaction of Warfarin with green vegetables containing large amounts of vitamin K reduces its effectiveness. All this dictates the need for regular monitoring of anticoagulants, which makes their use extremely difficult in areas where such monitoring is not organized or is of poor quality.
To monitor the effect of indirect anticoagulants, INR (International Normalized Ratio) or international normalized ratio (MHO) is usually used. The recommended INR interval for patients with CVD varies depending on the disease, but all heart diseases are in the range of 2-3.5. INR (INR) beyond the recommended level sharply increases the risk of hemorrhagic complications.
Clopidogrel (Plavix)
Platelet aggregation is a process that consumes energy. Platelets receive this energy from a special cell energy carrier, adenosine diphosphate (ADP). To do this, adenosine diphosphate needs to attach to a special binding site (receptor).
Clopidogrel irreversibly changes platelet ADP receptors, and therefore platelets remain nonfunctional throughout life, and restoration of normal function occurs as platelets are renewed (after approximately 7 days).
ADP receptor blockers are used if ASA is intolerant or if Aspirin does not work sufficiently. Compared with ASA, patients taking clopidogrel are more prone to bleeding and bruising.
Introduction
Diseases of the cardiovascular system associated with atherosclerosis currently occupy a leading position in terms of both mortality and disability of the population [1, 2].
In the scientific literature, most attention is paid to atherosclerosis of the coronary and brachiocephalic arteries [3]. However, recently, peripheral atherosclerosis has become a global problem due to its widespread prevalence: in economically developed countries, about 10% of the adult population suffers from ischemia of the lower extremities, while obliterating atherosclerosis accounts for 80–90% of cases [1, 4–6]. In the older age group, the proportion of people suffering from atherosclerosis (the main cause of ischemia of the lower extremities) is even higher [7]. It should also be borne in mind that, according to some authors, the prevalence of subclinical forms of the disease is 3–4 times higher than forms accompanied by pronounced clinical symptoms [1, 6, 8]. The constantly progressive nature of the disease, the high level of mortality and disability force us to recognize the problem of peripheral atherosclerosis as socially significant.
The material costs of both the patient and the state as a whole for the treatment of angiological diseases are often unreasonably high, which requires a revision of the management strategy for this group of patients. One of the main reasons for the significant costs of treatment is the delayed initiation of therapy, which, in turn, explains the large number of patients with severe degrees of arterial insufficiency [3]. Treatment of patients becomes significantly more expensive, and the effectiveness of therapy decreases due to late presentation of patients to medical institutions, the presence of diagnostic defects, as well as non-compliance by doctors with the principles of managing such patients. The greatest problem in light of the above are patients with “critical ischemia” of the lower extremities. It is understood as a condition characterized by the presence of constant pain at rest, which requires analgesic therapy, or the appearance of trophic ulcers of the distal extremities against the background of chronic arterial insufficiency. According to the Fontaine-Pokrovsky classification, this condition corresponds to grade 3–4 chronic ischemia of the lower extremities [9]. Compliance with diagnostic and treatment algorithms in cases where disease progression has not yet led to the development of critical ischemia allows us to reduce direct and indirect costs of treating patients, as well as significantly improve the clinical effect of therapy. Preserving the working capacity of this group of patients is also a socially significant factor.
Dental appointment
Factors influencing decision making:
- the scale of the planned operation;
- degree of hypocoagulation (monotherapy, dual antiplatelet therapy, Heparin, Warfarin, NOAC, etc.);
- topographic anatomy of the operated area.
Oral surgeries with the highest risk of possible bleeding include:
- Sinus lift.
- Invasive procedures in the floor of the mouth.
- Removal of impacted and dystopic wisdom teeth.
Assessing the risk of thromboembolism (depends on the disease and requires consultation with your doctor).
New generation anticoagulants
Rivaroxaban (Xarelto), Apixaban (Eliquis), and Dabigatran (Pradaxa)
Despite the fact that Warfarin has been a popular oral anticoagulant for more than 50 years, it has many limitations, such as high individual sensitivity and unpredictability of the anticoagulant effect, drug interactions, a narrow therapeutic range, the need for dose selection and constant monitoring of the INR. All this sharply reduces adherence to treatment and increases the risk of severe hemorrhagic complications.
Therefore, in recent years, the FDA has approved new anticoagulants that are safer and have a wider therapeutic range than their predecessors.
Today, a new generation of anticoagulants, which successfully replace Warfarin in many situations (cardiology, prevention and treatment of deep vein thrombosis of the extremities, in the treatment and prevention of strokes), allows us to get away from the problem of INR control. We are talking about three main drugs: Rivaroxaban (Xarelto), Apixaban (Eliquis) and Dabigatran (Pradaxa).
Factor Xa inhibitors (Eliquis and Xarelto) bind directly to the active site of factor Xa, which leads to blocking of the general coagulation pathway. This results in decreased thrombin formation, which in turn inhibits clot formation and platelet activation.
Direct thrombin inhibitors (Pradaxa) bind specifically and reversibly to the active site of thrombin. Due to thrombin inhibition, fibrin clot formation and platelet aggregation are reduced.
The standard test for monitoring patients on warfarin is the prothrombin time or INR, while the standard test for monitoring patients on heparin is the activated partial thromboplastin time or aPTT. Unfortunately, to date there are no laboratory tests to monitor patients taking NOACs. Currently, routine laboratory monitoring in patients taking new oral anticoagulants (NOACs) is not accepted due to the proven effectiveness of fixed doses. Therefore, the real degree of hypocoagulation in such patients is almost impossible to determine, which extremely complicates management tactics during surgical manipulations in the oral cavity. NOACs were developed as a physician- and patient-friendly alternative to vitamin K antagonists (VKAs) that did not require regular laboratory visits.
Secondary hemostasis (coagulation)
The formed platelet plug (without subsequent formation of fibrin) can only temporarily stop bleeding, and if the platelet thrombus does not thicken with insoluble fibrin, then such a thrombus will disintegrate after a few hours. Simultaneously with platelet activation, plasma coagulation factors are activated (secondary hemostasis). Goal: stabilization of the primary platelet plug due to the formation of fibrin networks and the formation of a dense and stable fibrin clot.
Clinical significance:
- if disturbances are present at the stages of primary hemostasis (vascular-platelet), for example, thrombocytopenia (< 50,000 cells/mm3) or taking antiplatelet drugs (Aspirin, Plavix), then prolonged and continuous bleeding should be expected during and immediately after surgery (due to disturbances in the formation of the primary platelet plug);
- if disturbances are present at the stages of secondary hemostasis (coagulation), and primary hemostasis is not impaired (for example, taking anticoagulants), bleeding problems will be detected only a few hours, or even the next day, after surgery (when the patient is no longer in the clinic) .
Patient taking antiplatelet drugs
Monotherapy
Recent studies have shown that basic surgical skills and local bleeding control measures are sufficient to control bleeding. Antiplatelet monotherapy does not pose a significant risk during or after surgery.
Recommendations [6]: it is strictly not recommended to interrupt the intake of oral antiplatelet agents during outpatient dental procedures, including surgical procedures.
Dual antiplatelet therapy after stent implantation in patients with stable coronary artery disease or acute coronary syndrome (ACS)
Cardiologists recommend dual antiplatelet therapy for at least six weeks after bare metal (inactive) stent implantation, and for 12 months after an episode of ACS or drug-eluting stent (active stent) implantation.
Recommendations [7]: Low-risk dentoalveolar surgery does not require any changes in the treatment plan.
Dentoalveolar surgery with an average risk of bleeding requires consultation with a cardiologist about temporarily stopping one of the drugs before the surgical procedure (monotherapy does not pose a serious risk). If it is not possible to cancel one of the drugs, you can perform the surgical procedure in stages: divide the surgical procedure with an average risk of bleeding into several smaller interventions.
Dentoalveolar surgical procedures with a high risk of bleeding require consultation with a cardiologist regarding temporary discontinuation of one of the medications before the surgical procedure. If it is not possible to discontinue one of the drugs, major surgical operations should be delayed for 1 year.