Pharmacological properties of the drug Labetalol
Non-selective blocker of β-adrenergic receptors with a selective blocking effect on postsynaptic α1-adrenergic receptors. Due to the presence of two optical centers in the molecule, there are four diastereoisomers of labetalol, which differ in the degree of pharmacological activity. The ratio of β- and α-adrenergic blocking activity of racemic labetalol is 3–7:1. As a result of interaction with α- and β-adrenergic receptors, labetalol causes vasodilation and a decrease in peripheral vascular resistance, leading to a decrease in systemic blood pressure without a significant decrease in cardiac output and the development of reflex tachycardia. The adverse effect of labetalol on the lipid spectrum of blood plasma is minimal. With systematic use, labetalol reduces the severity of left ventricular myocardial hypertrophy in patients with hypertension (arterial hypertension). Labetalol has a quinidine-like membrane-stabilizing effect, which, however, only occurs when labetalol is administered in very high doses. Compared with other beta-adrenergic blockers (eg propranolol), labetalol does not reduce glomerular filtration and renal blood flow. After oral administration, labetalol is rapidly and almost completely absorbed. Concomitant use with food slows down the absorption of labetalol in the intestine, but increases absolute bioavailability. It undergoes significant first-pass metabolism in the mucous membrane of the digestive tract and during the initial passage through the liver, due to which only about 25% of the administered dose of labetalol enters the systemic circulation unchanged. The hypotensive effect develops within 20 minutes - 2 hours after oral administration, the maximum effect occurs after 1-4 hours. The duration of the hypotensive effect is dose-dependent and ranges from 8 to 24 hours. The hypotensive effect after IV administration develops after 2-5 minutes and reaches its maximum expression in 5–15 minutes; its duration is 2–4 hours. The half-life in patients with normal renal function ranges from 2.5–8 hours. With severe renal failure, accumulation of labetalol is possible. Widely distributed in all tissues of the body, penetrates the placenta, and is excreted in breast milk. In small quantities it penetrates the BBB. Extensively metabolized in the liver by glucuronidation. About 30% is excreted in bile and excreted in feces, the rest is excreted in urine (55–60% as metabolites and 5% unchanged).
Links[edit]
- ^ abcdef "Monograph on labetalol hydrochloride for professionals". Drugs.com
. American Society of Health-System Pharmacists. Retrieved March 3, 2021. - ^ abcd British National Formulary: BNF 76
(76th ed.). Pharmaceutical press. 2021, pp. 147–148. ISBN 9780857113382. - "Use of labetalol during pregnancy". Drugs.com
. Retrieved March 11, 2021. - Fisher, Jnos; Ganellin, S. Robin (2006). Analog-based drug discovery. John Wiley and Sons. item 463. ISBN. 9783527607495.
- "Top 300 2020". ClinCalc
. Retrieved April 11, 2021. - "Labetalol - Drug Use Statistics". ClinCalc
. Retrieved April 11, 2021. - ^ab Koda-Kimble, Mary A.; Aldridge, Brian K. (2013). "21". Applied Coda-Kimble and Young Therapy: Clinical Use of Drugs
. Philadelphia: Philadelphia: Lippincott Williams & Wilkins. ISBN 978-1-60913-713-7. - Arulkumaran, N; Lightstone, L. (December 2013). "Severe preeclampsia and hypertensive crisis." Best practices and research. Clinical Obstetrics and Gynecology
.
27
(6):877–84. DOI: 10.1016/j.bpobgyn.2013.07.003. PMID 23962474. - ^ abcdefghijklmnopq "Trandate" (PDF). Prometheus Laboratories Inc. November 2010. Retrieved November 3, 2015.
- "Labetalol hydrochloride" (PDF). Hospira. May 2015. Retrieved November 3, 2015.
- Shiohara T, Kano Y (2007). "Lichen planus and lichenoid dermatoses." In Bolonia JL (ed.). Dermatology
. St. Louis: Mosby. item 161. ISBN. 978-1-4160-2999-1. - ^ abcd "Labetalol [package insert]. Spring Valley, NY: Par Pharmaceutical; 2011" (PDF). Archived from the original (PDF) on December 10, 2015. Retrieved November 3, 2015.
- ^ a b "Therapeutic chemistry of adrenergic and cholinergic drugs". Archived from the original on 2010-11-04. Retrieved October 16, 2010.
- ^ B s d e Louis, WJ; McNeill, JJ; Drummer, Ohio (1988). Doyle, A. E. (ed.). Labetalol and other vasodilators/beta blockers. IN: Handbook of Hypertension
. Amsterdam, The Netherlands: Elsevier Sciences Publishing Co., pp. 246–273. ISBN 978-0-444-90469-0. - Jump up
↑ Riva E, Mennini T, Latini R (December 1991).
"Alpha and beta adrenergic activity of labetalol and its RR-SR (50:50) stereoisomers". Br. J. Pharmacol
.
104
(4):823–8. DOI: 10.1111/j.1476-5381.1991.tb12513.x. PMC 1908821. PMID 1687367. - ^ ab Robertson D., Biagioni, I. Adrenergic antagonist drugs. In: Katzung BG, Masters SB, Trevor AJ, eds. Fundamental and clinical pharmacology. 12th ed. San Francisco, CA: McGraw Hill Lange Medical; 2012: 151–168. ISBN 978-0-07-176401-8.
- Katsung, Bertram G. (2006). Basic and Clinical Pharmacology
. New York: McGraw-Hill Medical. p. 170. ISBN 978-0-07-145153-6. - DA Richards; J. Tuckman; B. N. Pritchard (October 1976). "Evaluation of the alpha and beta adrenergic blocking effects of labetalol". Br J Clin Pharmacol
.
3
(5):849–855. DOI: 10.1111/j.1365-2125.1976.tb00637.x. PMC 1428931. PMID 9968. - "Labetalol | C19H24N2O3 - PubChem". pubchem.ncbi.nlm.nih.gov
. Retrieved November 4, 2015. - ^a b McCarthy, E.P.; Bloomfield, S. S. (1983-08-01). "Labetalol: a review of its pharmacology, pharmacokinetics, clinical use and side effects." Pharmacotherapy
.
3
(4): 193–219. DOI: 10.1002/j.1875-9114.1983.tb03252.x. ISSN 0277-0008. PMID 6310529. S2CID 20410587. - ^ a b c d Louis, WJ; McNeil, J.J.; Drummer, Ohio (1984-01-01). “Pharmacology of combined alpha-beta blockade. I". Drugs
. 28 Supplement 2: 16–34. DOI: 10.2165/00003495-198400282-00003. ISSN 0012-6667. PMID 6151889. S2CID 46974416. - ^ abc Robertson, D; Biagioni, I (2012). Katsung, B.G. (ed.). Adrenoreceptor antagonist drugs IN: Basic & Clinical Pharmacology
(12 ed.). San Francisco: McGraw Hill Lange Medical. pp. 151–168. ISBN 978-0-07-176401-8. - ^ abcd Westfall, David P. (2004). Craig, Charles R. (ed.). Adrenoreceptor antagonists IN: Modern pharmacology with clinical applications
(6th ed.). Baltimore, MD: Lippincott Williams and Wilkins. pp. 109–117. ISBN 978-0781737623. - Lund-Johansen, P. (1988-01-01). "Hemodynamic effects of beta-blocking compounds with vasodilatory activity: a review of labetalol, prisidilol and dilevalol." Journal of Cardiovascular Pharmacology
. 11 Supplement 2: S12–17. DOI: 10.1097/00005344-198800000-00004. ISSN 0160-2446. PMID 2464093. - ^ ab Lund-Johansen, P. (1984-01-01). “Pharmacology of combined alpha-beta blockade. II. Hemodynamic effects of labetalol." Drugs
. 28 Supplement 2: 35–50. DOI: 10.2165/00003495-198400282-00004. ISSN 0012-6667. PMID 6151890. S2CID 46986875. - Mottram, Allan R.; Erickson, Timothy B. (2009). Field, John (ed.). Toxicology in emergency cardiovascular care IN: Textbook of emergency cardiovascular care and CPR
. Philadelphia, PA: Lippincott WIlliams & Wilkins. pp. 443–452. ISBN 978-0-7817-8899-1. - Exam Zone (January 1, 2009). Elsevier's comprehensive guide. Elsevier India. P. 449–. ISBN 978-81-312-1620-0.
- Detlev Ganten; Patrick J. Mulrow (December 6, 2012). Pharmacology of antihypertensive therapy. Springer Science & Business Media. pp. 147–. ISBN 978-3-642-74209-5.
Use of the drug Labetalol
In case of hypertensive crisis, it is administered intravenously slowly (over 2 minutes) at a dose of 20 mg (2 ml of 1 % solution). If necessary, the administration is repeated at intervals of 10 minutes. It is preferable to administer labetalol as an infusion in an isotonic solution of sodium chloride or glucose (the concentration of the solution for infusion is 1 mg/ml) at a rate of 2 mg/min. Typically the effective dose is 50–200 mg. The total dose for adults when administered intravenously should not exceed 300 mg. Information on use in children is limited. It is recommended to administer orally at a rate of 4 mg/kg/day in 2 divided doses with constant monitoring of blood pressure levels. When administered intravenously, the bolus dose (administered slowly) is 0.2–1 mg/kg. The initial infusion rate is 0.4–1 mg/kg/h, the maximum is no more than 3 mg/kg/h.
Side effects of the drug Labetalol
dizziness, hypertension (arterial hypertension), syncope, orthostatic hypotension (mainly with intravenous administration), sinus bradycardia, AV block, increased symptoms of heart failure, headache, fatigue, depression, nightmares, paresthesia, nausea, vomiting, hepatotoxic effect, shortness of breath, sexual dysfunction (impotence, ejaculation disorders, decreased libido, priapism), urinary retention, hypoglycemia, itching, xerosis and hyperpigmentation of the skin, reversible alopecia, exfoliative dermatitis.
Contraindications
Labetalol is contraindicated in case of hypersensitivity to the drug, cardiogenic shock; GOST standards for myocardial infarction; uncontrolled initial heart failure or heart failure refractory to cardiac glycosides; Prinzmetal's angina; sinoatrial block; AV block II-III degree; for broncho-obstructive diseases or bronchial asthma; untreated pheochromocytoma; bradycardia, arterial hypotension; metabolic acidosis; severe peripheral circulatory disorders. Labetalol is not used in childhood and adolescence. Labetalol is contraindicated during pregnancy and breastfeeding. It is prescribed with caution for severe impairment of liver and kidney function, myasthenia gravis, diabetes mellitus, thyrotoxicosis, and psoriasis.
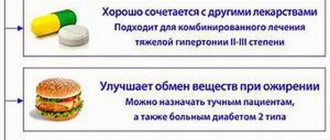
Drug interactions Labetalol
With simultaneous use of labetalol with other antihypertensive drugs, an additive effect is observed. When prescribed with verapamil or diltiazem, the risk of developing AV block increases. Undesirable pharmacodynamic interactions are possible when combined with the simultaneous use of labetalol and antidiabetic agents. Anesthetics can potentiate and prolong the hypotensive effect of labetalol. The combination of halothane and labetalol may produce a synergistic hypotensive effect, reducing cardiac output and lowering central venous pressure. Labetalol should be used with caution in patients taking MAO inhibitors due to the possibility of developing sinus bradycardia. Cimetidine increases the bioavailability of labetalol when administered concomitantly, probably by increasing absorption or decreasing first pass metabolism. Concomitant use of sympathomimetics may reduce the hypotensive effect of labetalol. Labetalol reduces nitroglycerin-induced reflex tachycardia and has additive hypotensive effects. With simultaneous use of labetalol with tricyclic antidepressants, tremor may develop. When used simultaneously with mefloquine, the risk of developing ECG changes and cardiac arrest increases.
List of pharmacies where you can buy Labetalol:
- Moscow
- Saint Petersburg
History[edit]
Labetalol was the first drug to combine both alpha and beta adrenergic receptor blocking properties. It was created to potentially correct the compensatory reflex problem that occurs when one receptor subtype is blocked, that is, vasoconstriction after blocking beta receptors or tachycardia after blocking alpha receptors. Because the reflex to block individual receptor subtypes prevents a decrease in blood pressure, it has been proposed that mild blocking of both alpha and beta receptors may work together to reduce blood pressure. [14] [21]