May 31, 2021
Most strokes occur due to a blockage in an artery leading to the brain or part of the brain. This disease is called ischemic stroke.
In the article we explain the causes of ischemic stroke, consider its types, as well as diagnostic methods, timing of when to undergo treatment after an ischemic stroke and recovery methods.
What is ischemic stroke
Ischemic stroke occurs when a mechanical obstacle occurs - an atherosclerotic plaque, embolus, thrombus. The clot blocks a blood vessel, cutting off blood flow to brain cells. The most common condition of stroke is the development of cholesterol in the walls of blood vessels (atherosclerosis). Fatty deposits narrow the artery and block blood flow to the brain.
Pathogenesis of ischemic stroke
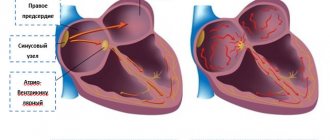
The difference between an ischemic stroke and a hemorrhagic stroke is that with a hemorrhagic stroke, bleeding into the brain occurs due to a ruptured vessel.
Hemorrhagic stroke occurs less frequently than ischemic stroke:
- ischemic stroke - in 80-85% of patients;
- hemorrhagic - in 10-15% of patients.
Types of ischemic stroke
There are a number of reasons why blockages in the arteries can form, causing an ischemic stroke. Experts identify several types of this disease.
Atherothrombotic stroke
Atherothrombotic ischemic stroke is when a blood clot forms at the site of an atherosclerotic plaque (fatty deposit), which clogs a vessel. Blood does not flow to the brain and because of this, cells die. The extent of brain damage varies from minor to extensive.
Common causes of this type of stroke:
- atherosclerosis.
Cardioembolic stroke
In the artery supplying the brain, a blockage occurs with emboli - this is a substrate that moves along the bloodstream. More often it occurs under abnormal conditions of the functioning of the human heart.
Common causes of this type of stroke:
- atrial fibrillation;
- heart valve disease;
- artificial heart valve;
- chronic heart failure;
- acute myocardial infarction;
- orthopedic surgeries, injuries.
Lacunar stroke
Lacunar ischemic stroke is characterized by damage to small arteries due to prolonged high blood pressure. In the tissues of the gray matter of the brain, softening occurs and a cavity is formed - a “lacuna”.
Common causes of this type of stroke:
- arterial hypertension;
- cerebral atherosclerosis;
- diabetes;
- other reasons.
Hemodynamic stroke
A sharp drop in blood pressure causes a lack of cerebral circulation.
Common causes of this type of stroke:
- acute heart failure;
- myocardial infarction;
- heart rhythm disturbance;
- bleeding;
- vascular collapse.
Hemorheological stroke
Impaired blood flow.
Common causes of this type of stroke:
- uncontrolled use of large diuretics;
- smoking abuse in combination with large doses of coffee and alcohol.
Classification
By nature, there are two main types of stroke: ischemic - the result of a sudden disruption of the blood circulation of a part of the brain and hemorrhagic - spontaneous (non-traumatic) intracranial hemorrhage. The ratio of ischemic and hemorrhagic strokes averages 5.0–5.5: 1, i.e. 80–85% and 15–20%, respectively. There is also a minor stroke, in which impaired functions are completely restored during the first 3 weeks of the disease. However, such relatively mild cases occur in only 10–15% of stroke patients.
There are several periods during the course of the disease.
Transient cerebrovascular accidents (TCI) are characterized by the sudden onset of focal neurological symptoms that develop in a patient with vascular disease and last several minutes, less often hours, but not more than a day and end with complete restoration of impaired functions. A special form of PNMK is acute hypertensive encephalopathy. More often, acute hypertensive encephalopathy develops in patients with malignant arterial hypertension and is clinically manifested by severe headache, nausea, vomiting, impaired consciousness, convulsive syndrome, and in some cases is accompanied by focal neurological symptoms. The appearance of a TIA or minor stroke indicates a high risk of repeated and, as a rule, more severe strokes, since the pathogenetic mechanisms of these conditions are largely similar and require prevention of repeated strokes.
Time intervals for the development of stroke are presented in Table 1.
| The most acute period | Acute period | Early recovery period | Late recovery period | Persistent residual effects | ||
| 0-3(hours) | Up to 24 hours | Up to 3 days | Up to 21 days | Up to 6 months | Up to 2 years | After 2 years |
| Therapeutic window | PNMK | Small stroke | Stroke with persistent residual effects | |||
Anatomical and physiological characteristics of cerebral circulation
The human brain makes up approximately 2% of body weight, while it consumes 20% of all incoming oxygen and 17% of all glucose. Unlike other organs, the brain does not have oxygen reserves; the consumption of all reserve oxygen, if its supply ceases, is completed within 10–12 s. Loss of consciousness occurs 5–7 seconds after “turning off” blood circulation in the brain. If total cerebral ischemia does not exceed 100 s, consciousness returns without signs of damage to the nervous system. Irreversible changes in the cells of the cerebral cortex occur with ischemia for more than 5 minutes, in the cells of the midbrain - 10 minutes, in the medulla oblongata - 20-25 minutes. When blood flow in the brain is resumed after a > 5-minute pause, the “Phenomenon of the absence of capillary perfusion” develops (the phenomenon of non-restoration of blood flow) - a perfusion block is formed due to changes in the endothelium and pronounced glial edema. The longer the total ischemia, the greater the surface area of the brain with the phenomenon of non-restoration of blood flow. Ischemia duration of 7.5 minutes – 10% of the brain surface; in 15 minutes – 50% of the brain surface.
Cerebral blood flow is characterized by two features: self-regulation (depending on the level of metabolic activity of individual brain areas and the gas composition of the blood) and independence (relative) from the state of general hemodynamics (independence of cerebral blood flow from the state of systemic hemodynamics is possible only within the range of systolic blood pressure from 80 to 190 –200 mmHg).
The blood supply to the brain is carried out by two internal carotid arteries and two vertebral arteries, venous outflow through the internal jugular veins and further into the superior vena cava. The main arteries of the head enter the cranial cavity and divide into cerebral arteries. The largest of them are the anterior and middle cerebral on each side and the basilar artery, with the help of connecting arteries, form the circle of Willis.
The cerebral arteries form two fundamentally different systems:
1) One of them has the character of an arterial network, which is located in the arachnoid membrane and covers the surface of the cerebral hemispheres. From the loops of this vascular network, perpendicularly directed intracerebral short (branch in the cortex) and long (branch in the underlying white matter) arteries plunge into the substance of the brain.
2) The vascular system of the subcortical formations, diencephalon and brain stem is built differently. It is represented by arteries that arise not from the vascular network, but from the arteries of the circle of Willis, which, heading vertically from the base of the skull, plunge into the medulla.
The intracerebral arteries of both systems with numerous branches form a continuous vascular-capillary network. From the post-capillary network of the cortex and white matter, the main part of the blood flows into the superficial venous network, also located in the arachnoid membrane, and from the area of subcortical formations - into the deep veins of the brain. These systems are connected by numerous interhemispheric anastomoses. Further outflow occurs into the sinuses of the dura mater, and then into the internal jugular veins and partially into the external jugular veins. The venous system of the brain is characterized by a branched network, an abundance of anastomoses, the absence of valves and the presence of venous lines (sinuses) that protect the brain from compression. All this allows blood to flow freely and protects the brain from increased intracranial pressure. Two thirds of the blood enters the brain through the internal carotid arteries - the carotid system and one third through the vertebral arteries - the vertebrobasilar system.
Etiology and pathogenesis of stroke
Based on the mechanism of occurrence, there are 4 main subtypes of ischemic stroke.
1.Atherothrombotic stroke – most often associated with atherosclerotic lesions of extracranial and intracranial arteries. Atherosclerotic plaque (atheroma) forms in large or medium-sized arteries, often at the site of their division into smaller branches. Growing atheroma not only narrows the vessel, but also contributes to the formation of a blood clot, causing blockage (occlusion) of the vessel. Most often, occlusion of the main arteries of the neck (internal carotid and vertebral) is observed. But with good collateral blood flow and slow progression, even complete blockage may remain asymptomatic. However, clots can separate from the forming thrombus, and ulceration of a plaque is also possible, the particles of which will clog the small overlying vessels of the brain (arterio-atrial embolism).
2. Cardioembolic stroke. The most common source of embolism is the heart. Cardiogenic embolism can occur with atrial fibrillation or myocardial infarction due to mural thrombus formation, prosthetic valves, infective endocarditis (a source of septic and fibrin emboli), marantic endocarditis, Liebman-Sachs endocarditis and atrial myxoma. The source of emboli can be an ulcerated atherosclerotic plaque in the aortic arch, the mouth of the great arteries or the carotid artery (local embolism).
3. Hemorheological stroke is caused by an increase in blood viscosity (polycythemia vera, secondary erythrocytosis, leukemia, etc.). The hemodynamic type of stroke is caused by a violation of cardiac output, leading to disruption of the systemic circulation (paroxysmal arrhythmias, collapse with a sharp drop in blood pressure, etc.).
4. Lacunar stroke is associated with pathology of small cerebral arteries (diameter 30-100 µm). Typically, a lacunar stroke, the size of which ranges from a few millimeters to 1.5 cm, is a consequence of blockage of small branches of the cerebral arteries supplying blood to the deep parts of the brain (basal ganglia, thalamus, pons, cerebellum). The most common cause of lacunar strokes (75%) is hypertensive microangiopathy (arteriosclerosis), which occurs with prolonged arterial hypertension.
Rare causes of ischemic stroke include cerebral vein thrombosis, paradoxical embolism (foramen ovale patent), meningovascular syphilis, tuberculous arteritis, collagen arteritis, giant cell arteritis, Takayasu arteritis, fibromuscular dysplasia, subclavian steal syndrome, and dissecting aortic aneurysm. In the pathogenesis of cerebral infarction, the main role is played by a critical decrease in cerebral blood flow - below 50 ml per minute per 100 g of brain substance, due to a disorder of general or local hemodynamics, which triggers a cascade of pathogenetic reactions leading ultimately to apoptosis (a sharp decrease in the functional state) and death neuron.
Hemorrhagic stroke is divided into
— Intracerebral (parenchymal) hemorrhage - the outflow of blood from a ruptured vessel into the brain tissue with the formation of a hematoma of various sizes, which causes the occurrence of neurological manifestations. The main causes of intracerebral hemorrhage are arterial hypertension, intracranial aneurysm (including microaneurysms formed as a result of traumatic brain injury or septic conditions), arteriovenous malformation, cerebral amyloid angiopathy, the use of anticoagulants or thrombolytics, diseases accompanied by hemorrhagic syndrome (leukemia, uremia, Werlhof's disease, etc.). since hypertension often affects small vessels, hematomas with hypertensive hemorrhage often form in the subcortical areas - the basal ganglia, thalamus, pons, cerebellum. — Subarachnoid hemorrhages - the outpouring of blood into the intrathecal space of the brain - are mainly caused by the rupture of an aneurysm: saccular, S-shaped, spherical, etc. (80% of all cases). Aneurysms form at a site of congenital weakness in the arterial wall and are present in 5% of the population by age 20, but rupture is more common after age 40. Arteriovenous malformations are a congenital anomaly of the development of cerebral vessels (5% of all cases). In approximately 30% of cases, the cause cannot be determined. A provoking factor may be a sharp increase in blood pressure (during physical stress, straining, during sexual intercourse, etc.), severe alcohol intoxication, and in the elderly - a pronounced deterioration in venous outflow during night sleep.
What is a transient ischemic attack (TIA)
Transient ischemic stroke or transient ischemic attack (TIA) is a short-term disruption of brain function when blood circulation stops in one area, and is restored after a few hours. Local ischemia lasts no more than 24 hours, then it is reversible.
The main difference between TIA and ischemic stroke is that the first disease does not cause any changes in the brain. Scientists are currently examining the brain to determine whether TIA actually causes permanent changes to the brain.
New research tells a different story:
- TIA up to 5 minutes - no changes in the brain;
- TIA from 6 to 30 minutes - changes in the brain in every third person;
- TIA from 12 to 24 hours - changes in the brain of ⅔ patients.
It is important to understand that a transient ischemic attack is a precursor to a stroke, so you need to track it, see the subtle symptoms and consult a doctor as soon as possible to prevent stroke. From 10% to 40% of TIAs end in stroke, the risk is greatest in the first week after a transient ischemic attack.
At first glance, the symptoms of a TIA are indistinguishable from a stroke:
- darkening of the eyes;
- decreased vision;
- loss of vision in one eye;
- other visual impairments;
- speech disturbance, as if “porridge in the mouth”;
- inability to pronounce a word;
- inability to formulate words and sentences in your head;
- sensory disturbance;
- movement disorders;
- weakness in the body;
- numbness of the face;
- numbness of the upper and lower extremities;
- dizziness;
- falling without loss of consciousness;
- disorientation in time and space;
- memory impairment for recent events;
- loss of balance.
Diagnosis of stroke
The diagnosis is based on a thorough study of the medical history, identification of risk factors and analysis of clinical data, namely neurological symptoms. The clinical picture of strokes is varied and is largely determined by the vascular system in which the cerebral catastrophe occurred and its nature (ischemia or hemorrhage).
Early diagnosis of stroke (history and examination) involves answering the following questions:
— Does the patient have acute damage to the brain or spinal cord or their membranes?
— Is this lesion caused by a stroke?
ACVA is diagnosed with the sudden (minutes, less often hours) appearance of focal and/or general cerebral and meningeal neurological symptoms in a patient with a general vascular disease and in the absence of other causes, namely: traumatic brain or spinal injury; intoxication (alcohol, drugs, medications); hypoglycemia; infection; renal failure; liver failure.
Focal neurological symptoms are manifested by the occurrence of the following disorders:
– motor: mono-, hemi-, paraparesis – weakness in one or two limbs; paresis of the cranial nerves – facial asymmetry, hyperkinesis, etc.
– speech: sensory, motor aphasia – impaired understanding and pronunciation of words, dysarthria – unclear pronunciation of words, “porridge in the mouth”;
– sensitive: hypalgesia, thermoanesthesia, violation of deep, complex types of sensitivity, etc.;
– coordinators: vestibular, cerebellar ataxia, astasia, abasia – dizziness, unsteadiness when walking, falling to any side.
– visual: scotomas, quadrant and hemianopsia, amaurosis, photopsia – decreased or absent vision, loss of visual fields;
– cortical functions: astereognosis, apraxia – violation of the order of actions;
– memory: fixation amnesia, disorientation in time, etc.
General cerebral symptoms: decreased level of wakefulness from subjective feelings of “vagueness,” “fogginess” in the head and mild stupor to deep coma; headache and pain along the spinal roots, nausea, vomiting.
Meningeal symptoms (can appear simultaneously with general cerebral and/or focal neurological symptoms, but more often appear somewhat delayed after the clinical debut of a stroke; with subarachnoid hemorrhages it can be the only clinical syndrome): tension of the posterior cervical muscles, positive Kernig, Brudzinsky signs (upper, middle, lower ), Bekhtereva, etc.
The most common first symptoms of a stroke are: sudden numbness or weakness in the arm and/or leg; sudden difficulty speaking and/or understanding it; sudden loss of balance, lack of coordination, dizziness; sudden loss of consciousness; severe headache for no apparent reason or after severe stress, physical overexertion sudden numbness of the lip or half of the face, often with “distortion” of the face.
Urgently call an ambulance by phone “03” if you see any of these symptoms in your friends or relatives or feel any of these symptoms yourself! A direct relationship between the outcome of a stroke and the time of initiation of its treatment has been proven. Every minute counts!
If a stroke is suspected, the patient must be hospitalized in a specialized neurological department for the treatment of patients with stroke.
Causes of stroke
Factors that influence the development of ischemic stroke, increase the likelihood of the disease occurring, experts divide into two groups: those that can be influenced and, thanks to proper treatment, prevent a stroke, and those that cannot be influenced, but with proper prevention the risks can be reduced.
The first group (cannot be influenced) includes the following symptoms:
- floor;
- age;
- genetics - first-degree relatives who had a stroke.
The second group (can be influenced) includes:
- arterial hypertension (high blood pressure);
- diabetes;
- TIA and/or previous stroke;
- obesity;
- cardiac ischemia;
- lipid metabolism disorder;
- carotid artery stenosis;
- heart rhythm disturbance - atrial fibrillation;
- heart failure;
- smoking;
- alcohol abuse;
- use of certain medications;
- severe stress.
Having these diseases and habits, it is necessary to consult a specialist to prevent a stroke and reduce the risks of it happening.
If a stroke occurs - assessment of the person’s condition, symptoms and first aid
If you notice the first symptoms, which is typical for an ischemic stroke, then you need to call an ambulance as soon as possible. A quick response will save time, and therefore increase the chance of reducing the various consequences of this unforeseen disease.
When diagnosing yourself, you need to pay attention to the following signs - what is included in an ischemic stroke, symptoms:
- weakness, loss of sensation, numbness in the face, arms or legs. Most often on one side of the body;
- decrease or loss of vision;
- loss of speech, difficulty pronouncing a word or sentence, impossible to understand someone else's speech;
- severe headache without any reason, which does not go away with the use of medications that previously helped;
- memory loss;
- it is difficult to navigate in space and perceive what is happening;
- nausea;
- vomit;
- swallowing disorder;
- loss of balance for no apparent reason.
The above signs of ischemic stroke are quite difficult to remember. To make it easier for you, experts have developed a special test that helps identify stroke symptoms and quickly provide assistance for ischemic stroke. It is called FAST - after the first abbreviations of human body parts.
FAST = FAST
Face - face
Arm - hand
Speech - speech
Time - time
We have described how to use the test in the instruction table:
| Part of the body | What to do | If it's a stroke, then... |
| Face | Ask the person to smile or show their teeth | An asymmetry appears on the face: the lips on one side of the face will rise in a smile, and on the other they will be lowered down. |
| Hand | Ask the person to raise both arms and hold them there for 5 seconds. | One hand will go down at once |
| Speech | Ask the person to say a simple phrase, for example, “the sun is bright outside.” | A person may not understand what you asked to do, and if he understands, the spoken phrase will sound incomprehensible, incoherent, and illegible. |
| Time | Call an ambulance if you see any of the signs above. | It is important not to waste time and seek help as quickly as possible. |
Hospitalization - treatment of ischemic stroke
After a person is in the hospital, doctors conduct a full examination to determine the general condition of the patient and give him an accurate diagnosis - what was it, an ischemic or hemorrhagic stroke, or perhaps the person has a completely different disease.
Diagnosis of ischemic stroke is carried out using diagnostic procedures:
- computed tomography (CT);
- magnetic resonance imaging (MRI);
- Doppler ultrasound (USDG).
After the diagnosis has been established, taking into account the chosen rehabilitation strategy and the person’s condition, the patient is placed in a neurological, neurosurgical or intensive care unit, where doctors provide treatment and recovery after an ischemic stroke and prescribe medications.
At the first stages, doctors of different specialties begin to work with a person. Treatment after an ischemic stroke includes:
- neurologist;
- ophthalmologist;
- endocrinologist (if necessary);
- psychologist;
- speech therapist;
- orthopedist;
- exercise therapy specialist;
- masseur;
- physiotherapist;
And basic therapy is carried out, where doctors provide external respiration function, if necessary, monitor blood pressure, correct elevated body temperature, and reduce cerebral edema.
Medical Internet conferences
Introduction. With the development of ultrasound and computer diagnostic methods at the end of the 20th century, the role of cardiocerebral embolism in the structure of ischemic strokes has significantly increased [1]. Currently, more than 20 nosological forms of cardiac pathology have been described - sources of cerebral embolism [2-4]. Cardioembolic strokes (CEI) are characterized by high mortality and a significant incidence of disability in the general structure of ischemic strokes [5,6]. Stroke in young patients always requires the exclusion of cardioembolic origin of the disease. We present our own observation of patient T., 29 years old.
Clinical case. Patient T., 29 years old, was observed by pediatricians since childhood with a diagnosis of congenital heart disease: bicuspid aortic valve. He coped with the loads, surgical treatment was not offered. Since the late 1990s (10-12 years old), he began to notice the appearance of shortness of breath during physical activity (climbing to the 1st floor), which passed at rest. From that time on, he began to notice the appearance of acrocyanosis of the nasolabial triangle. In 2001 (15 years old), due to increasing shortness of breath, which began to occur when climbing several steps, he was examined at the cardiocenter of Samara, where coarctation of the aorta was detected, followed by surgical treatment: a bypass anastomosis of the site of aortic coarctation. After the operation I felt satisfactory. I took Curantil for several months, then, without any reason, I stopped taking it on my own. He coped with the loads satisfactorily, shortness of breath did not bother me. For 2 years after the operation, he was observed by a cardiologist in Samara, where he lived at that time. Then he was not treated or examined. Shortness of breath did not bother me, and blood pressure did not increase.
Specialized secondary education, worked as a designer. He has been smoking 20 cigarettes a day since he was 15 years old. Denies smoker's cough. Denies alcohol abuse and drug use.
On December 27, 2015, patient T. was transported by ambulance to the intensive care unit (ICU) of the Regional Clinical Hospital (RCH) in Saratov with impaired speech and movements in the left upper and lower extremities. From the medical history, it is known that he considers himself sick since the end of October 2015, when he began to notice the appearance of nasal congestion and an increase in body temperature to 37.50C. The patient regarded nasal congestion as sinusitis, and was treated independently at home with vasoconstrictor drugs and antibacterial drugs (i.m. Cefazolin). Against this background, he noted a slight improvement in the form of a decrease in body temperature and a decrease in nasal congestion. However, from the end of November 2015, he began to notice the appearance of pain in the knee and ankle joints, which occurred during movement and went away with rest; he also began to notice the appearance of heaviness in the right hypochondrium; he took Essentiale on his own. On 12/27/15, the patient went to bed, woke up and noted a speech disorder, lack of active movements in the upper and lower extremities on the left. An ambulance was called, he was hospitalized in the district hospital, then was transferred to the OKB, to the ICU with a diagnosis of cerebral infarction. Ultrasound of the abdominal organs: hepatosplenomegaly. According to magnetic resonance imaging (MRI) of the brain: MRI shows an ischemic stroke in the area of the right middle cerebral artery, dislocation syndrome. To verify the source of the embolism, transthoracic echocardiography (Echo-CG) was performed on December 30, 2015 ( Fig ). Conclusion: condition after surgical treatment of congenital heart disease: Coarctation of the aorta. Bypass surgery using a vascular prosthesis. Dilatation of the ascending aorta is aneurysmal. UPS. Bicuspid aortic valve. Combined aortic disease: slight aortic stenosis, closer to moderate, to moderate aortic regurgitation. Many hyperechoic structures on the aortic valve leaflets. The dimensions of the heart cavities and global contractility of the LV myocardium were within normal limits. Left ventricular FI 63%. MPAP 41 mmHg. Slight hypertrophy of the left ventricular myocardium. Mild to moderate mitral regurgitation. To moderate tricuspid regurgitation. Considering the structural changes in the aortic valve leaflets, it is most likely that there is a history of infective endocarditis. In connection with the examination data in the ICU, the patient was consulted by a cardiologist and diagnosed with infective endocarditis. Antibacterial therapy was started on December 31, 2015 (Ceftriaxone + Gentamicin). Against this background, the body temperature was in the range of 37.0-37.8 0C, cardialgia, heaviness in the right hypochondrium, and joint pain were not bothered. From the ICU, the patient was transferred to the neurology department with stroke, where antibacterial therapy was continued (Ceftriaxone +, Gentamicin, which was canceled on January 12, 2015, Editsin 2 g/day was prescribed, but after the 1st administration an allergic reaction like urticaria was noted , in connection with which Editsin was canceled). Laboratory tests revealed positive markers of chronic viral hepatitis C, blood cultures did not test for sterility of growth, ESR - 39 mm/h, hemoglobin - 96 g/l. Examined by a speech therapist: pseudobulbar dysarthria, spastic-paretic form. Examined by a neuropsychologist: syndrome of damage to the basal ganglia of the brain on the right. On the background of antibacterial therapy, from January 11, 2016, the body temperature returned to normal. Cardialgia, joint pain, heaviness in the right hypochondrium do not bother me. Hospitalized in the cardiology department for continued treatment and examination with a diagnosis of cerebral infarction, cardioembolic origin, in the territory of the right middle cerebral artery on 12/27/15. Central prosoparesis on the left. Left-sided hemiplegia. Right basal ganglia lesion syndrome. Infectious endocarditis of the native aortic valve. ACHD, bicuspid aortic valve. CHD, coarctation of the aorta. Bypass surgery using a vascular prosthesis in 2001.
When examined in the cardiology department: the condition is serious. Position active. Consciousness is clear. The skin is of normal color, warm, dry. Rash: no. Spider veins: no. Scars: in the 5th intercostal space from the left sternal line to the anterior axillary line. Skin turgor is normal. The mucous membranes are pink. Subcutaneous tissue: moderately developed (height 172 cm, weight 65 kg). Edema of the lower extremities – no. Lymph nodes: not palpable. Joints: active, full passive mobility. Acropachia, most pronounced on the upper extremities ( Fig. 2 ). A catheter was installed in the area of the right subclavian vein. Respiratory rate 18 per minute. On percussion there is a clear pulmonary sound above the lung parenchyma; on auscultation, breathing is harsh. Heart sounds are rhythmic, muffled, in the area of the projection of the aortic valve there is moderate systole-diastolic murmur, I tone>II tone at the apex of the heart (2:1). Heart rate = pulse = 64 per minute, the same in both arms, satisfactory qualities. Blood pressure 90/60 mm Hg. Art. Palpation of the abdomen is painless. The liver is palpated, the edge has a dense elastic consistency, slightly rounded, percussion dimensions according to Kurlov are 12x10x9 cm, the spleen is palpated, percussion its dimensions: 7x12 cm. The kidney area is not visually changed. Palpation in the projection of the bladder is painless. The symptom of tapping in the lumbar region is negative on both sides. Tendon reflexes: D=S. There are no pathological reflexes. Sense organs: decreased vision.
Data from the examination results: Hemoglobin - 100 g/l, erythrocytes - 3.14x1012 per l, leukocytes 7.6x109 per l, ESR - 38 mm/hour. Total cholesterol - 5.0 mmol/l; LDL - 3.8 mmol/l, ALT 16 u/l, AST 15 u/l. Blood test for HIV infection dated 12/31/15: negative. ECG: Sinus rhythm with heart rate 70 per minute. Horizontal position of the electrical axis of the heart. Violation of intraventricular conduction. Complete block of the right bundle branch. ( Fig. 3 ). Holter ECG monitoring: sinus rhythm, sinus arrhythmia (at night). Average heart rate is 71 beats per minute. The circadian index is 1.17. Paroxysm of unstable supraventricular tachycardia (1 episode). Rare (94) single, paired (5), aberrant (72) daytime supraventricular extrasystoles. Rare (45) single, bigeminy type in one episode, monotopic ventricular extrasystoles of the daytime type. No ST segment deviations were recorded. Consultative appointment with a neurologist on January 21, 2016: clear consciousness, communicative, oriented. Speech and swallowing are not impaired. FMN – pupils OD=OS, photoreaction preserved, no nystagmus. The face is asymmetrical, the nasolabial fold on the left is smoothed, the left corner of the mouth is slightly lowered. The tongue is deviated to the left. Tendon reflexes S>D. Left-sided hemiplegia. Left-sided hemihyposthesia. The Babinski sign on the left is positive. There are no meningeal symptoms. Ultrasound of the abdominal organs: hepatosplenomegaly.
Final diagnosis:
Main: Infectious endocarditis of the native aortic valve. UPS. Coarctation of the aorta. Bypass surgery using a vascular prosthesis in 2001. Combined aortic disease: moderate stenosis, moderate insufficiency. Relative mitral insufficiency stage II. Relative tricuspid insufficiency grade III. Pulmonary hypertension stage I Mild anemia. Hepatosplenomegaly. Dyslipidemia.
Cerebral infarction, cardioembolic origin, in the territory of the right MCA from 12/27/15. Central prosoparesis on the left. Left-sided hemiplegia. Syndrome of damage to the basal ganglia of the brain on the right. Placement of the subclavian catheter on the right 12/28/15, removal 01/25/16.
Sop.: Retinal angiopathy OU. Chronic viral hepatitis C.
Donkey: Dislocation syndrome. Single ventricular and supraventricular extrasystole. Paroxysm of unstable supraventricular tachycardia.
Treatment was carried out: Cereton 1200 mg/day, Mexidol solution 600 mg/day, cancelled, Cefogram solution 4 g/day IV drops + tab. Tavanik 500 mg/day, physiotherapeutic treatment. During treatment, stable normalization of temperature, hemodynamic stability, improvement in general condition, leukocyte level, ESR in the blood test were within normal limits. In a stable condition of moderate severity, he was transferred to a district hospital to continue treatment. It is recommended to continue combination antibacterial therapy for up to 6 weeks.
Conclusion. The difficulty of diagnosing cardioembolic stroke is clearly demonstrated in this clinical case. One of the difficulties in diagnosing infective endocarditis and CES, as its complications, is its manifestation, which often leads specialists into diagnostic confusion. It is worth noting that the information content of the classical diagnostic method - transthoracic echo-CG in this case is quite low, which is associated with the impossibility of optimal visualization and assessment of the extent of damage to the aortic valve and vascular prosthesis after surgical treatment of aortic coarctation according to transthoracic echo-CG only. It is recommended to use a transesophageal sensor, which increases the sensitivity of the method to 90-93%. Also in this clinical situation, significant damage to the aortic valve dictates the need for cardiac surgery as the main method of treating this condition. The patient was consulted by a cardiac surgeon, and after stabilizing his condition, he was recommended to go to a cardiac surgery center for aortic valve replacement.
The presented clinical observation proves the difficulties of diagnosing IE, while simultaneously demonstrating that the joint well-coordinated work of cardiologists and neurologists can save the lives of young patients.
Prevention and treatment of complications
Complications can occur after both ischemic and hemorrhagic strokes. Most often, neurological symptoms in ischemic stroke are not as severe as in hemorrhagic stroke, so the main thing for doctors is to combat complications and correct treatment after an ischemic stroke.
A major ischemic stroke affects the large arteries that supply blood to the brain; due to lack of nutrition, one of the brain hemispheres may be affected. Each affected hemisphere of the brain has its own consequences.
| Ischemic stroke (right side) consequences | Ischemic stroke (left side) consequences |
|
|
There are several types of complications that require immediate proper treatment:
Brain swelling
If this complication exists, then doctors try to relieve brain swelling - they use hormonal therapy, place the head in an elevated position, and relieve pain and cramps. Sometimes decompressive surgery is necessary to remove part of the skull bone and avoid squeezing the brain.
Inflammatory processes in the lungs
Inflammation in humans can occur in several cases when swallowing is impaired and food enters the respiratory tract, or from prolonged immobilization and suppression of the cough reflex. Doctors relieve inflammation with antibiotics and other drug therapies.
Inflammation of the urinary tract
Inflammation can begin due to the fact that a person, for example, has a urinary catheter installed. Inflammation can also be relieved with the help of antibiotics and other medications.
Deep vein thrombosis
The disease occurs when the deep veins of the lower extremities are blocked by blood clots. To avoid blood clots in the early stages, a person is given physical therapy and compression garments are used.
Stiffness in the joints
When the limbs remain immobilized for a long time, stiffness occurs in the joints. They are treated with passive physical therapy of paralyzed limbs to avoid the development of contractures.
Colon dysfunction
Intestinal dysfunction occurs when there is difficulty in bowel movements or absence of stool. This problem is solved with a special diet, which includes foods rich in fiber. If the problem is more serious than a lack of diet, then they resort to enemas or laxatives.
Bedsores
They arise from impaired blood supply in places where bone structures are close to the surface of the skin. Most often, bedsores form on the back of the head, shoulder blades, elbows, sacrum, knees, and heels.
Prevention of the formation of bedsores includes a constant change in the position of the human body, proper hygienic treatment of the skin, regular daily examination of the body, proper bedding - not crumpled, dry, clean, without small debris, massage of the skin surfaces.
If bedsores do appear, they are treated using special solutions, ointments, and bandages.
Differential diagnosis.
It should be remembered that in conditions such as hypoglycemia, uremia, liver failure, the sudden appearance of focal neurological disorders is possible. In case of infectious diseases, purulent diseases of the paranasal sinuses, the rapid development of focal/meningeal disorders is also possible, in this case indicating the addition of meningoencephalitis. One should not forget about traumatic brain injuries as the cause of loss of consciousness and the appearance of focal neurological disorders, especially in cases where the medical history is unknown and verbal contact with the patient is impossible; a careful examination and palpation of the soft tissues of the head, examination of the external auditory organs helps in the differential diagnosis and nasal passages for cerebrospinal fluid and hematorrhea; with subdural hematomas, anisocoria is detected in more than 90% of cases. With exogenous and endogenous intoxications (alcohol, ketoacidosis, etc.), leading to deep depression of consciousness, difficulties in differential diagnosis may also arise, since rare and shallow breathing does not allow the smell of alcohol, acetone, etc. to be detected in the exhaled air. Sudden appearance of focal neurological symptoms it is also possible with brain tumors - a “stroke-like” course of the disease or in the post-attack period in patients suffering from epileptic seizures (Todd’s palsy). In this condition, the resulting focal symptoms completely regress within 24 hours, and their appearance is caused not by “stroke” changes, but by local cerebral edema. In patients suffering from migraines, a sudden development of focal neurological symptoms (ophthalmic, oculomotor, sensory, motor, speech disorders, etc.) is also possible, the appearance of which may precede an attack of headache and disappear with the development of the migraine attack itself.
Diagnosis of the nature of the stroke
There are no characteristic clinical signs for hemorrhagic and ischemic strokes.
Clarification of the nature of the stroke is possible only after neuroimaging (computed tomography or magnetic resonance imaging).
Treatment of strokes.
Stroke therapy is divided into basic and specific.
Basic therapy for stroke is carried out regardless of the nature of stroke and begins from the first minutes of the patient’s admission to a specialized hospital.
— Normalization of vital functions - breathing and cardiovascular activity. If consciousness is not disturbed or depressed no deeper than stupor (the patient opens his eyes if called), it is necessary to sanitize the upper respiratory tract and ensure free breathing (elimination of factors that impede breathing - tight clothing, uncomfortable head position, recessed tongue, dentures, etc. .). If consciousness is depressed deeper than stupor, oxygen inhalation is necessary, and if breathing is inadequate, mechanical ventilation is necessary.
— The fight against high or low blood pressure is carried out in stages. Stabilization of elevated blood pressure at a level exceeding 20 mm Hg. the level familiar to the patient, and in the absence of anamnestic data, not lower than 150–160/90 mm Hg. Art.
— Combating cerebral edema (intracranial hypertension). Cerebral edema is defined as excess accumulation of fluid in the brain tissue, resulting in swelling and increased volume of the brain. But the bone walls of the skull are not extensible! Intracranial pressure increases sharply, which causes displacement of brain structures, and sometimes their compression. One of the main methods of treating cerebral edema is the administration of special medications - osmotic diuretics. They create high osmotic pressure in the blood, which forces fluid from the brain tissue along a pressure gradient into the blood, the flow of which carries it away from the cranial cavity.
— Maintaining water and electrolyte balance — the optimal ratio of fluid and electrolytes (potassium, sodium) in the body.
— Maintaining normal blood glucose levels (glycemia), since low (hypoglycemia) and high (hyperglycemia) blood glucose levels are equally dangerous for the brain, so it is necessary to maintain normoglycemia.
— Maintaining normal body temperature, since temperatures above 38*C aggravate brain damage, therefore temperature reduction is carried out both with medication and with the help of external cooling (water-alcohol rubdowns, ice packs). But be sure to find out the cause of the fever, since this may be a manifestation of an infection that requires completely different treatment.
— The fight against deep vein thrombosis in bedridden patients (the risk of pulmonary embolism and death of the patient) is carried out by elastic bandaging of the lower extremities, the use of pneumatic massagers, as well as the use of small doses of anticoagulants (heparin, fraxiparin), which reduce the tendency to thrombus formation.
— Relief of psychomotor agitation, epileptic seizures, nausea and vomiting, pain syndrome is carried out by special groups of drugs.
- Prevention of bedsores is mandatory - treating the patient’s skin, turning him over in bed, positioning the limbs with the help of special pillows. Rehabilitation of the patient begins as early as possible. Early rehabilitation – on days 2-3 when the patient’s condition is stable – significantly improves the outcome of stroke. This includes passive movements in the limbs for the prevention of contractures, verticalization of the patient using a special table - a verticalizer, in a stable condition - mobilization of the patient: transfer to a chair several times a day, physical therapy, physical therapy, for speech and swallowing disorders - speech therapy correction.
— The patient’s nutrition begins from 1-2 days. If swallowing is impaired (swallowing function is assessed immediately upon hospitalization and during treatment), a nasogastric tube is installed and nutritional mixtures are used for nutrition. If the patient is conscious and can swallow, then nutrition is carried out in the usual way.
Special methods for treating stroke.
Without an accurate determination of the nature of the stroke, it is impossible to carry out special treatment! The decision to use a particular drug or method can only be made by the patient’s attending physician. Treatment for a stroke will depend on the type of stroke.
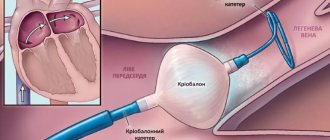
1. In ischemic stroke, the main goals will be to restore cerebral blood flow and protect nerve cells from further damage. Thrombolytics (alteplase) are medications that dissolve blood clots. They are very effectively used in the treatment of myocardial infarction. By dissolving the clot and restoring blood flow, these drugs can prevent the development of damage to nerve cells and, therefore, cerebral infarction or significantly reduce its size. However, the use of such promising drugs is limited by the development of complications, the most serious of which is the “translation” of an ischemic stroke into a hemorrhagic one, i.e. secondary hemorrhage develops in the damaged brain tissue. Therefore, these drugs are indicated only for a strictly defined group of patients and can be used only in the earliest stages of stroke development (up to 4 hours from the onset). Anticoagulant drugs (warfarin) help stop the growth of existing blood clots and prevent the formation of new ones. This results in a decrease in blood clotting. This can lead to the development of internal bleeding; the risk is especially high in patients with gastric or duodenal ulcers and blood diseases. Another group of drugs that change the rheological properties of blood are called antiplatelet agents (aspirin). These drugs inhibit platelet sticking (aggregation). Antiplatelet agents are among the standard treatments for stroke caused by cerebral atherosclerosis and various blood diseases, which are based on its tendency to form blood clots due to platelet aggregation. These drugs are often used to prevent the development of both first and recurrent strokes. Thrombolytics, anticoagulants, and antiplatelet agents help restore and improve cerebral blood flow.
Unfortunately, without receiving the necessary oxygen and nutrients, brain cells begin to die. At the same time, a whole cascade of biochemical reactions is launched in them. Protective medications help stop this mechanism. They are called neuroprotectors, or cytoprotectors (from the Latin cytos - “cell”). Currently, serious clinical trials of drugs from this group are being conducted. It will be shown exactly how much the cerebral infarction is reduced when using these drugs. In addition, neuroprotectors help the cells surrounding the dead survive this “stress.” They increase their activity and even help some “volunteers” who were not previously involved in providing movement and/or speech, reorganize and, to a certain extent, take on the responsibilities of the dead.
Surgical methods for treating ischemic stroke include carotid endarterectomy. This operation is the method of choice if the cause of the stroke is severe stenosis or blockage of the carotid artery by an atherosclerotic plaque. It is also used to prevent the occurrence of both first and recurrent strokes. However, there are clearly defined indications and contraindications for this operation.
2. In hemorrhagic stroke, the main goals are to control blood pressure and stop bleeding. Lowering blood pressure helps reduce blood pressure on the walls of blood vessels, and bleeding stops faster. Blood pressure correction is carried out with antihypertensive (pressure-lowering) drugs that the patient takes orally (tablets and capsules) and which are administered intravenously to the patient. It all depends on the general condition of the patient, his blood pressure level and its fluctuations. It would seem that it is possible to perform an operation and “sew up” the ruptured vessel. However, this is not always possible and should be done. First, the bleeding may stop on its own if your blood pressure is controlled. Secondly, unfortunately, there are inoperable cases when the hemorrhage is very deep in the depths of the brain and the surgeon’s path to it is not easy. A neurosurgical operation is performed when it is possible to remove a sufficiently large hematoma, more than forty cubic centimeters, which compresses adjacent brain structures. This intervention can be carried out in two ways, open and closed. In the first case, neurosurgeons open the patient’s skull (perform trepanation) - an open intervention, and in the second case, using a special technique, they insert a cannula through a small hole into the very center of the hemorrhage and remove the spilled blood. The second option is called closed, or stereotactic, intervention. If the hemorrhage occurs from a rupture of an aneurysm, most often a congenital saccular protrusion on the wall of a vessel, then it is “sutured” with special metal clips - the aneurysm is clipped.
Life goes on after a stroke. But even after a relatively mild stroke, there is no need to succumb to “rosy” optimism. Any stroke is a serious warning about trouble in the body. Some advice for a patient who has suffered a stroke: Start recovery measures as quickly as possible: as soon as the general well-being of the patient and his state of consciousness allow it (for more details, see the section on the rehabilitation of a patient with a stroke). The patient’s relatives and friends should actively help him in conducting additional classes (in relation to the main ones conducted by the methodologist of therapeutic gymnastics and speech therapist-aphasiologist) in therapeutic gymnastics, in learning to walk and self-care, in restoring speech, reading and writing. The care of loved ones and a favorable psychological climate in the family should at the same time exclude “overprotection.” The patient must be given maximum independence, he must be encouraged to have an active social life. Return to active life, and where possible, to work, can occur not only with complete restoration of impaired functions, but also against the background of remaining partial motor and speech defects. And it is necessary to take measures to prevent a recurrent stroke (carefully read the guidelines on stroke prevention).
Life after ischemic stroke - rehabilitation and prevention of recurrent stroke
Proper rehabilitation plays the main role in a person’s recovery after a stroke and his return to independent life.
Rehabilitation sets itself the task of restoring the patient’s lost functions to the extent possible and adapting him to the changed living conditions.
The principles of rehabilitation include several important aspects:
- early onset;
- A complex approach;
- individual rehabilitation program;
- intermediate and long-term goals;
- multidisciplinary team of doctors;
- a person’s motivation to recover;
- active patient participation;
- continuity;
- involving relatives and friends in the rehabilitation process.
You can learn more about why an integrated approach to rehabilitation is more effective and how doctors work in a multidisciplinary team here.
Ischemic stroke. Stages of rehabilitation
The consequences and recovery after an ischemic stroke depend on the time of initiation of rehabilitation. The sooner you start working with specialists, the better the result will be, and the likelihood of complications will decrease.
Rehabilitation after an ischemic stroke includes two stages: hospital, during hospitalization, and home, after discharge from the hospital. After leaving the hospital, a person can take quotas and go to a sanatorium, undergo rehabilitation procedures at a clinic, or seek help from specialists for rehabilitation at home.
Recovery periods after ischemic stroke