Liprimar 20mg No. 30 tablets
Release form
Film-coated tablets
Compound
1 tablet contains: Active substance: atorvastatin (in the form of calcium salt) 10, 20, 40 and 80 mg; Excipients: calcium carbonate, microcrystalline cellulose, lactose monohydrate, sodium carboxymethylcellulose, polysorbate 80, hydroxypropylcellulose, magnesium stearate, Opadry White YS-1-7040, simethicone emulsion, powdered wax.
Package
14 and 30 pcs.
pharmachologic effect
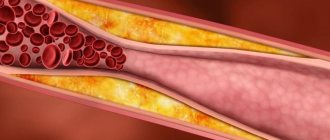
Liprimar is a lipid-lowering drug. Atorvastatin is a selective competitive inhibitor of HMG-CoA reductase, a key enzyme that converts 3-hydroxy-3-methylglutaryl-CoA into mevalonic acid, a precursor of steroids, including cholesterol. In patients with homozygous and heterozygous familial hypercholesterolemia, non-familial forms of hypercholesterolemia and mixed dyslipidemia, Liprimar reduces the level of total cholesterol (C), low-density lipoprotein cholesterol (LDL-C) and apolipoprotein B, as well as the content of very low-density lipoprotein cholesterol (VLDL-C) and triglycerides, causes an unstable increase in high-density lipoprotein cholesterol (HDL-C). In the liver, triglycerides and cholesterol are incorporated into very low-density lipoproteins (VLDL), enter the plasma and are transported to peripheral tissues. VLDL produces low-density lipoproteins (LDL), which are catabolized by interaction with high-affinity LDL receptors. Like LDL, cholesterol-rich and triglyceride-rich lipoproteins (VLDL, intermediate-density lipoproteins, and chylomicron remnants) may also contribute to the progression of atherosclerosis. An increase in plasma triglyceride levels is often combined with a decrease in HDL-C levels and the appearance of small LDL particles, as well as other non-lipid metabolic risk factors for coronary artery disease. In this regard, the independent role of hypertriglyceridemia as an independent risk factor for coronary artery disease has not been convincingly proven. The independent effect of increasing HDL levels or decreasing triglyceride levels on the risk of coronary or cardiovascular events and death from these causes has also not been established. Liprimar reduces the levels of cholesterol and lipoproteins in the blood plasma by inhibiting HMG-CoA reductase and cholesterol synthesis in the liver and increasing the number of “liver” LDL receptors on the cell surface, which leads to increased uptake and catabolism of LDL-C. Atorvastatin reduces the formation of LDL-C and the number of LDL particles. Causes a pronounced and persistent increase in the activity of LDL receptors, combined with favorable qualitative changes in LDL particles. Reduces the level of LDL-C in patients with homozygous hereditary hypercholesterolemia, resistant to therapy with other lipid-lowering drugs. Atorvastatin at a dose of 10-80 mg reduces the level of total cholesterol by 30-46%, LDL-C by 41-61%, apolipoprotein B by 34-50% and triglycerides by 14-33%. Treatment results are similar in patients with heterozygous familial hypercholesterolemia, non-familial forms of hypercholesterolemia and mixed hyperlipidemia, incl. in patients with non-insulin-dependent diabetes mellitus. In patients with isolated hypertriglyceridemia, atorvastatin reduces the level of total cholesterol, LDL-C, VLDL-C, apolipoprotein B, triglycerides and non-HDL-C and increases the level of HDL-C. In patients with dysbetalipoproteinemia, it reduces the level of intermediate-density lipoprotein cholesterol. In patients with hyperlipoproteinemia types IIa and IIb according to the Fredrickson classification, the average increase in HDL-C levels during treatment with atorvastatin (10-80 mg), compared with the initial value, is 5.1-8.7% and does not depend on the dose. There is a significant dose-dependent decrease in the ratios: total cholesterol/HDL-C and LDL-C/HDL-C by 29-44% and 37-55%, respectively. Atorvastatin at a dose of 80 mg significantly reduces the risk of ischemic complications and death by 16% after a 16-week course, and the risk of readmission for angina pectoris accompanied by signs of myocardial ischemia by 26%. In patients with different initial levels of LDL-C, atorvastatin causes a comparable reduction in the risk of ischemic complications and death (in patients with myocardial infarction without a Q wave and unstable angina, men and women, patients under and over 65 years of age). Liprimar (10 mg/day) significantly reduces the incidence of the following complications: ischemic heart disease (fatal + non-fatal heart attack) - by 36%, cardiovascular diseases and the use of revascularization procedures - by 20%, ischemic heart disease - by 29%, stroke (including fatalities) - by 26%. There was no significant reduction in overall mortality and mortality from cardiovascular complications with the use of Liprimar, but there was a trend towards a decrease in mortality.
Indications for use
In combination with diet to reduce elevated total cholesterol, LDL-C, apolipoprotein B and triglycerides and increase HDL-C in patients with primary hypercholesterolemia (heterozygous familial and non-familial hypercholesterolemia) and mixed hyperlipidemia (types IIa and IIb according to the Fredrickson classification), in whom diet therapy does not provide an adequate effect; in combination with diet for the treatment of patients with elevated serum triglyceride levels (Fredrickson type IV) and patients with dysbetalipoproteinemia (Fredrickson type III) in whom dietary therapy does not provide an adequate effect; to reduce the levels of total cholesterol and LDL-C in patients with homozygous familial hypercholesterolemia with insufficient effectiveness of diet therapy and other non-pharmacological treatments; to reduce the risk of fatal outcomes of coronary artery disease and the risk of developing myocardial infarction, angina pectoris, stroke and to reduce the need for revascularization procedures in patients with cardiovascular diseases and/or dyslipidemia, as well as if these diseases are not identified, but there are at least three risk factors for the development of IHD, such as age over 55 years, smoking, arterial hypertension, low concentrations of HDL-C in the blood plasma, cases of early development of IHD in relatives.
Contraindications
Active liver disease or increased serum transaminase activity (more than 3 times the upper limit of normal) of unknown origin; women of reproductive age who do not use adequate methods of contraception; pregnancy; lactation (breastfeeding); hypersensitivity to the components of the drug; in children and adolescents under 18 years of age, the effectiveness and safety of Liprimar have not been established. It should be used with caution in patients who abuse alcohol and/or have liver disease (history).
Directions for use and doses
Before starting treatment with Liprimar, an attempt should be made to control hypercholesterolemia through diet, exercise and weight loss in obese patients, as well as treatment of the underlying disease. When prescribing the drug, the patient must be recommended a standard lipid-lowering diet, which he must follow during treatment. The drug can be taken at any time of the day, regardless of meals. The dose of the drug (from 10 to 80 mg 1 time / day) is selected taking into account the initial levels of LDL-C, the purpose of therapy and the individual effect. At the beginning of treatment and/or during dose increases of Liprimar, plasma lipid levels should be monitored every 2-4 weeks and the dose adjusted accordingly. In case of primary hypercholesterolemia and combined (mixed) hyperlipidemia, in most patients the required effect can be achieved by using Liprimar at a dose of 10 mg 1 time / day. The therapeutic effect appears within 2 weeks and usually reaches a maximum within 4 weeks. With long-term treatment, the effect persists. For patients with homozygous familial hypercholesterolemia, the drug is prescribed at a dose of 80 mg 1 time / day (in most cases, therapy led to a decrease in LDL-C levels by 18-45%. Impaired renal function does not affect the plasma level of atorvastatin or the degree of reduction in LDL-C levels when using Liprimar, therefore no change in the dose of the drug is required. When using the drug in elderly patients, there were no differences in the safety, effectiveness or achievement of goals of lipid-lowering therapy compared with the general population.
Use during pregnancy and breastfeeding
Liprimar® is contraindicated during pregnancy. Women of reproductive age should use adequate contraception during treatment. Liprimar® can be prescribed to women of reproductive age only if the likelihood of pregnancy is very low and the patient is informed about the possible risk of treatment to the fetus. Liprimar® is contraindicated during breastfeeding. It is not known whether atorvastatin is excreted in breast milk. If it is necessary to prescribe the drug during lactation, breastfeeding should be stopped to avoid the risk of adverse events in infants.
Side effects
From the central nervous system: insomnia, headache, asthenic syndrome. From the gastrointestinal tract: nausea, diarrhea, abdominal pain, dyspepsia, constipation, flatulence. From the musculoskeletal system and connective tissue: myalgia. From the central nervous system and peripheral nervous system: malaise, dizziness, amnesia, paresthesia, peripheral neuropathy, hypoesthesia. From the gastrointestinal tract: vomiting, anorexia, hepatitis, pancreatitis, cholestatic jaundice. From the musculoskeletal system and connective tissue: back pain, muscle cramps, myositis, myopathy, arthralgia, rhabdomyolysis. Allergic reactions: urticaria, skin itching, rash, anaphylactic reactions, bullous rash, multiform exudative erythema (including Stevens-Johnson syndrome), toxic epidermal necrolysis (Lyell's syndrome). Metabolism: hypoglycemia, hyperglycemia, increased serum creatine phosphokinase (CPK). From the hematopoietic organs: thrombocytopenia. Other: impotence, peripheral edema, weight gain, chest pain, secondary renal failure, alopecia, tinnitus, increased fatigue.
special instructions
As with the use of other lipid-lowering drugs of the same class, after treatment with Liprimar, a moderate (more than 3 times compared to the upper limit of normal) increase in serum activity of liver transaminases was noted. A persistent increase in serum levels of hepatic transaminases (more than 3 times the upper limit of normal) was observed in 0.7% of patients receiving Liprimar in clinical studies. The incidence of such changes when using the drug in doses of 10, 20, 40 and 80 mg was 0.2%, 0.2%, 0.6% and 2.3%, respectively. Increased liver transaminase activity was not usually accompanied by jaundice or other clinical manifestations. When the dose of Liprimar was reduced, or the drug was temporarily or completely discontinued, the activity of liver transaminases returned to the original level. Most patients continued taking atorvastatin at a reduced dose without any side effects. Before starting, 6 weeks and 12 weeks after starting the drug or after increasing the dose, as well as during the entire course of treatment, liver function tests should be monitored. Liver function should also be examined if clinical signs of liver damage appear. If the level of liver transaminases increases, their activity should be monitored until it returns to normal. If an increase in AST or ALT activity by more than 3 times compared to the upper limit of normal persists, a dose reduction or discontinuation of the drug is recommended. Myalgia was observed in patients receiving Liprimar. The diagnosis of myopathy (muscle pain and weakness in combination with an increase in CPK activity by more than 10 times the upper limit of normal) should be considered in patients with widespread myalgia, muscle soreness or weakness and/or a marked increase in CPK activity. Liprimar therapy should be discontinued in the event of a marked increase in CPK activity or in the presence of confirmed or suspected myopathy. The risk of myopathy during treatment with other drugs in this class was increased with concomitant use of cyclosporine, fibrates, erythromycin, niacin, or azole antifungals. Many of these drugs inhibit metabolism mediated by the cytochrome P450 isoenzyme CYP3A4 and/or drug transport. Atorvastatin is biotransformed by CYP3A4. When prescribing Liprimar in combination with fibrates, erythromycin, immunosuppressants, azole antifungals or nicotinic acid in lipid-lowering doses, you should carefully weigh the expected benefits and risks of treatment and regularly monitor patients to identify pain or weakness in the muscles, especially during the first months of treatment and during periods of increasing the dose of any drug. In such situations, periodic determination of CPK activity can be recommended, although such monitoring does not prevent the development of severe myopathy. Atorvastatin may cause an increase in CPK activity. When using Liprimar, as well as other drugs of this class, cases of rhabdomyolysis with acute renal failure caused by myoglobinuria have been described. Liprimar therapy should be temporarily discontinued or completely discontinued if signs of possible myopathy appear or if there is a risk factor for the development of renal failure due to rhabdomyolysis (for example, severe acute infection, hypotension, major surgery, trauma, metabolic, endocrine and electrolyte disturbances, and uncontrolled seizures). Patients should be warned to seek immediate medical attention if they experience unexplained muscle pain or weakness, especially if accompanied by malaise or fever.
Drug interactions
The risk of myopathy during treatment with HMG-CoA reductase inhibitors increases with simultaneous use of cyclosporine, fibrates, erythromycin, clarithromycin, azole derivative antifungals, and nicotinic acid in lipid-lowering doses. Inhibitors of the cytochrome CYP3A4 isoenzyme. Since atorvastatin is metabolized by the cytochrome CYP3A4 isoenzyme, the combined use of atorvastatin with inhibitors of the cytochrome CYP3A4 isoenzyme may lead to an increase in the concentration of atorvastatin in the blood plasma. The degree of interaction and potentiation effect are determined by the variability of the effect on the cytochrome CYP3A4 isoenzyme. Inhibitors of the transport protein OATP1B1. Atorvastatin and its metabolites are substrates of the transport protein OATP1B1. OATP1B1 inhibitors (eg cyclosporine) may increase the bioavailability of atorvastatin. Thus, the combined use of atorvastatin at a dose of 10 mg and cyclosporine at a dose of 5.2 mg/kg/day leads to an increase in the concentration of atorvastatin in the blood plasma by 7.7 times
Overdose
Treatment: There is no specific antidote to treat an overdose of Liprimar. In case of overdose, symptomatic treatment should be provided as needed. Since the drug actively binds to plasma proteins, hemodialysis is ineffective.
Storage conditions
Store at a temperature not exceeding 25°C, out of the reach of children.
Best before date
3 years
Liprimar®
During treatment with HMG-CoA reductase inhibitors, with simultaneous use of cyclosporine, fibrates, nicotinic acid in lipid-lowering doses (more than 1 g / day) or inhibitors of the CYP3A4 isoenzyme / transport protein (for example, erythromycin, clarithromycin, antifungal agents - azole derivatives), the risk increases myopathy (see section “Special instructions”).
CYP3A4 isoenzyme inhibitors
Since atorvastatin is metabolized by the CYP3A4 isoenzyme, co-administration of atorvastatin with inhibitors of the CYP3A4 isoenzyme may lead to increased plasma concentrations of atorvastatin. The degree of interaction and potentiation effect is determined by the variability of the effect on the CYP3A4 isoenzyme.
It was found that potent inhibitors of the CYP3A4 isoenzyme lead to a significant increase in the concentration of atorvastatin in the blood plasma. The simultaneous use of strong inhibitors of the CYP3A4 isoenzyme (for example, cyclosporine, telithromycin, clarithromycin, delavirdine, stiripentol, ketoconazole, voriconazole, itraconazole, posaconazole and HIV protease inhibitors, including ritonavir, lopinavir, atazanavir, indinavir, darunavir, etc.) should be avoided whenever possible. . If concomitant use of these drugs is necessary, initiating therapy at the lowest dose should be considered and the possibility of reducing the maximum dose of atorvastatin should be evaluated.
Moderate inhibitors of the CYP3A4 isoenzyme (for example, erythromycin, diltiazem, verapamil and fluconazole) may lead to increased plasma concentrations of atorvastatin. With the simultaneous use of HMG-CoA reductase inhibitors (statins) and erythromycin, an increased risk of developing myopathy was noted. Interaction studies between amiodarone or verapamil and atorvastatin have not been conducted. Both amiodarone and verapamil are known to inhibit the activity of the CYP3A4 isoenzyme, and simultaneous use of these drugs with atorvastatin may lead to increased exposure to atorvastatin. In this regard, it is recommended to reduce the maximum dose of atorvastatin and carry out appropriate monitoring of the patient's condition when used simultaneously with moderate inhibitors of the CYP3A4 isoenzyme. Monitoring should be carried out after the start of therapy and against the background of changing the dose of the inhibitor.
Gemfibrozil/fibrates
With the use of fibrates in monotherapy, adverse reactions, including rhabdomyolysis, affecting the musculoskeletal system were periodically noted. The risk of such reactions increases with simultaneous use of fibrates and atorvastatin. If the simultaneous use of these drugs cannot be avoided, the minimum effective dose of atorvastatin should be used, and the patient's condition should be regularly monitored.
Ezetimibe
The use of ezetimibe is associated with the development of adverse reactions, including rhabdomyolysis, from the musculoskeletal system. The risk of such reactions increases with simultaneous use of ezetimibe and atorvastatin. For such patients, careful monitoring is recommended.
Erythromycin/clarithromycin
With the simultaneous use of atorvastatin and erythromycin (500 mg 4 times a day) or clarithromycin (500 mg 2 times a day), inhibitors of the CYP3A4 isoenzyme, an increase in the concentration of atorvastatin in the blood plasma was observed (see sections "Special instructions" and "Pharmacokinetics" ).
Protease inhibitors
The simultaneous use of atorvastatin with protease inhibitors, known as inhibitors of the CYP3A4 isoenzyme, is accompanied by an increase in the concentration of atorvastatin in the blood plasma.
Diltiazem
The combined use of atorvastatin at a dose of 40 mg with diltiazem at a dose of 240 mg leads to an increase in the concentration of atorvastatin in the blood plasma (see section “Pharmacokinetics”).
Cimetidine
No clinically significant interaction of atorvastatin with cimetidine was detected (see section “Pharmacokinetics”).
Itraconazole
The simultaneous use of atorvastatin in doses from 20 mg to 40 mg and itraconazole in a dose of 200 mg led to an increase in the AUC value of atorvastatin (see section "Pharmacokinetics").
Grapefruit juice
Since grapefruit juice contains one or more components that inhibit the CYP3A4 isoenzyme, its excessive consumption (more than 1.2 L per day) may cause an increase in the concentration of atorvastatin in the blood plasma (see section "Pharmacokinetics").
Transport protein inhibitors
Atorvastatin is a substrate of liver enzyme transporters (see section "Pharmacokinetics").
Co-administration of atorvastatin 10 mg and cyclosporine 5.2 mg/kg/day resulted in increased atorvastatin exposure (AUC ratio: 8.7) (see Pharmacokinetics section). Cyclosporine is an inhibitor of organic anion transport polypeptide 1B1 (OATP1B1), OATP1B3, multidrug resistance-associated protein 1 (MDR1) and breast cancer resistance protein, as well as CYP3A4, and therefore increases the exposure of atorvastatin. The daily dose of atorvastatin should not exceed 10 mg (see section “Dosage and Administration”).
Glecaprevir and pibrentasvir are inhibitors of OATP1B1, OATP1B3, MDR1 and breast cancer resistance protein, and therefore increase the exposure of atorvastatin. The daily dose of atorvastatin should not exceed 10 mg (see section “Dosage and Administration”).
Co-administration of atorvastatin 20 mg and letermovir 480 mg daily resulted in increased atorvastatin exposure (AUC ratio: 3.29) (see Pharmacokinetics section).
Letermovir is an inhibitor of the transporters P-gp, BCRP, MRP2, OAT2 and the hepatic transporter OATP1B1/1B3, thus increasing the level of exposure to atorvastatin. The daily dose of atorvastatin should not exceed 20 mg (see section “Dosage and Administration”). The magnitude of indirect drug interactions between CYP3A and OATP1B1/1B3 on co-administration of drugs may differ when letermovir is co-administered with cyclosporine. It is not recommended to use atorvastatin in patients receiving letermovir therapy in combination with cyclosporine.
Elbasvir and grazoprevir are inhibitors of OATP1B1, OATP1B3, MDR1 and breast cancer resistance protein and therefore increase the exposure of atorvastatin. Should be used with caution and at the lowest dose required (see section "Dosage and Administration").
Inducers of the CYP3A4 isoenzyme
The combined use of atorvastatin with inducers of the CYP3A4 isoenzyme (for example, efavirenz, rifampicin or St. John's wort preparations) may lead to a decrease in the concentration of atorvastatin in the blood plasma. Due to the dual mechanism of interaction with rifampicin (an inducer of the CYP3A4 isoenzyme and an inhibitor of the hepatocyte transport protein OATP1B1), simultaneous use of atorvastatin and rifampicin is recommended, since delayed administration of atorvastatin after taking rifampicin leads to a significant decrease in the concentration of atorvastatin in the blood plasma (see section “Pharmacokinetics”). However, the effect of rifampicin on the concentration of atorvastatin in hepatocytes is unknown and if concomitant use cannot be avoided, the effectiveness of this combination should be carefully monitored during therapy.
Antacids
Simultaneous oral administration of a suspension containing magnesium hydroxide and aluminum hydroxide reduced the concentration of atorvastatin in the blood plasma (change in AUC: 0.66), but the degree of reduction in the concentration of LDL-C did not change.
Phenazone
Atorvastatin does not affect the pharmacokinetics of phenazone, so interaction with other drugs metabolized by the same cytochrome isoenzymes is not expected.
Colestipol
With simultaneous use of colestipol, the concentration of atorvastatin in the blood plasma decreased (change in AUC: 0.74); however, the lipid-lowering effect of the combination of atorvastatin and colestipol was superior to that of each drug alone.
Digoxin
With repeated administration of digoxin and atorvastatin at a dose of 10 mg, the equilibrium concentrations of digoxin in the blood plasma did not change. However, when digoxin was used in combination with atorvastatin at a dose of 80 mg/day, digoxin concentrations increased (AUC change: 1.15). Patients receiving digoxin in combination with atorvastatin require appropriate monitoring.
Azithromycin
With simultaneous use of atorvastatin at a dose of 10 mg 1 time per day and azithromycin at a dose of 500 mg 1 time per day, the concentration of atorvastatin in the blood plasma did not change.
Oral contraceptives
With simultaneous use of atorvastatin and oral contraceptives containing norethisterone and ethinyl estradiol, increased concentrations of norethisterone (AUC change 1.28) and ethinyl estradiol (AUC change 1.19) were observed. This effect should be taken into account when choosing an oral contraceptive for a woman taking atorvastatin.
Terfenadine
With simultaneous use of atorvastatin and terfenadine, no clinically significant changes in the pharmacokinetics of terfenadine were detected.
Warfarin
In a clinical study in patients regularly receiving warfarin therapy, concomitant use of atorvastatin at a dose of 80 mg per day resulted in a slight increase in prothrombin time of approximately 1.7 s during the first 4 days of therapy. The indicator returned to normal within 15 days of atorvastatin therapy.
Although significant interactions affecting anticoagulant function have been observed only in rare cases, the prothrombin time should be determined before initiating atorvastatin therapy in patients receiving coumarin anticoagulant therapy and frequently enough during therapy to prevent a significant change in the prothrombin time. Once stable prothrombin time values are observed, its monitoring can be carried out in the same way as recommended for patients receiving coumarin anticoagulants.
When changing the dose of atorvastatin or discontinuing therapy, prothrombin time should be monitored according to the same principles as described above.
Atorvastatin therapy was not associated with bleeding or changes in prothrombin time in patients not receiving anticoagulant treatment.
Colchicine
Although studies have not been conducted on the simultaneous use of colchicine and atorvastatin, there are reports of the development of myopathy when using this combination. Caution should be exercised when atorvastatin and colchicine are used concomitantly.
Amlodipine
In a drug interaction study in healthy subjects, coadministration of atorvastatin 80 mg and amlodipine 10 mg resulted in a clinically nonsignificant increase in atorvastatin concentrations (AUC change: 1.18)
Fusidic acid
During post-marketing studies, cases of rhabdomyolysis have been reported in patients taking concomitant statins, including atorvastatin and fusidic acid. The mechanism of this interaction is unknown. In patients for whom the use of fusidic acid is considered necessary, statin treatment should be discontinued for the entire period of use of fusidic acid. Statin therapy can be resumed 7 days after the last dose of fusidic acid. In exceptional cases where long-term systemic therapy with fusidic acid is necessary, for example for the treatment of severe infections, the need for co-administration of atorvastatin and fusidic acid should be considered on a case-by-case basis and under close medical supervision. The patient should seek immediate medical attention if symptoms of muscle weakness, tenderness, or pain occur.
Other concomitant therapy
In clinical studies, atorvastatin was used in combination with antihypertensive agents and estrogens as part of hormone replacement therapy. There were no signs of clinically significant adverse interactions; No interaction studies with specific drugs have been conducted.
In addition, an increase in the concentration of atorvastatin was observed when used simultaneously with HIV protease inhibitors (combinations of lopinavir and ritonavir, saquinavir and ritonavir, darunavir and ritonavir, fosamprenavir, fosamprenavir with ritonavir and nelfinavir), hepatitis C protease inhibitors (boceprevir, elbasvir/grazoprevir, simeprevir) , clarithromycin and itraconazole.
Caution should be exercised when using these drugs together and the lowest effective dose of atorvastatin should be used.
Liprimar film-coated tablets 20 mg 30 pcs. in Novosibirsk
During treatment with HMG-CoA reductase inhibitors, with simultaneous use of cyclosporine, fibrates, nicotinic acid in lipid-lowering doses (more than 1 g / day) or inhibitors of the CYP3A4 isoenzyme / transport protein (for example, erythromycin, clarithromycin, antifungal agents - azole derivatives), the risk increases myopathy (see section “Special instructions”).
CYP3A4 isoenzyme inhibitors
Since atorvastatin is metabolized by the CYP3A4 isoenzyme, the combined use of atorvastatin with inhibitors of the CYP3A4 isoenzyme may lead to an increase in the concentration of atorvastatin in the blood plasma. The degree of interaction and potentiation effect is determined by the variability of the effect on the CYP3A4 isoenzyme.
It was found that potent inhibitors of the CYP3A4 isoenzyme lead to a significant increase in the concentration of atorvastatin in the blood plasma. The simultaneous use of strong inhibitors of the CYP3A4 isoenzyme (for example, cyclosporine, telithromycin, clarithromycin, delavirdine, stiripentol, ketoconazole, voriconazole, itraconazole, posaconazole and HIV protease inhibitors, including ritonavir, lopinavir, atazanavir, indinavir, darunavir, and others) should be avoided whenever possible. If concomitant use of these drugs is necessary, initiating therapy at the lowest dose should be considered and the possibility of reducing the maximum dose of atorvastatin should be evaluated.
Moderate inhibitors of the CYP3A4 isoenzyme (for example, erythromycin, diltiazem, verapamil and fluconazole) may lead to increased plasma concentrations of atorvastatin. With the simultaneous use of HMG-CoA reductase inhibitors (statins) and erythromycin, an increased risk of developing myopathy was noted. Interaction studies between amiodarone or verapamil and atorvastatin have not been conducted. Both amiodarone and verapamil are known to inhibit the activity of the CYP3A4 isoenzyme, and simultaneous use of these drugs with atorvastatin may lead to increased exposure to atorvastatin. In this regard, it is recommended to reduce the maximum dose of atorvastatin and carry out appropriate monitoring of the patient's condition when used simultaneously with moderate inhibitors of the CYP3A4 isoenzyme. Monitoring should be carried out after the start of therapy and against the background of changing the dose of the inhibitor.
Gemfibrozil/fibrates
During the use of fibrates in monotherapy, adverse reactions were periodically noted, incl. rhabdomyolysis affecting the musculoskeletal system. The risk of such reactions increases with simultaneous use of fibrates and atorvastatin. If the simultaneous use of these drugs cannot be avoided, the minimum effective dose of atorvastatin should be used, and the patient's condition should be regularly monitored.
Ezetimibe
The use of ezetimibe is associated with the development of adverse reactions, incl. rhabdomyolysis, from the musculoskeletal system. The risk of such reactions increases with simultaneous use of ezetimibe and atorvastatin. For such patients, careful monitoring is recommended.
Erythromycin/clarithromycin
With the simultaneous use of atorvastatin and erythromycin (500 mg 4 times / day) or clarithromycin (500 mg 2 times / day), inhibitors of CYP3A4, an increase in the concentration of atorvastatin in the blood plasma was observed (see sections “Special instructions” and “Pharmacokinetics”) .
Protease inhibitors
The simultaneous use of atorvastatin with protease inhibitors, known as CYP3A4 inhibitors, is accompanied by an increase in the concentration of atorvastatin in the blood plasma.
Diltiazem
The combined use of atorvastatin at a dose of 40 mg with diltiazem at a dose of 240 mg leads to an increase in the concentration of atorvastatin in the blood plasma (see section “Pharmacokinetics”).
Cimetidine
No clinically significant interaction of atorvastatin with cimetidine was detected (see section “Pharmacokinetics”).
Itraconazole
The simultaneous use of atorvastatin in doses from 20 mg to 40 mg and itraconazole in a dose of 200 mg led to an increase in the AUC value of atorvastatin (see section “Pharmacokinetics”).
Grapefruit juice
Since grapefruit juice contains one or more components that inhibit the CYP3A4 isoenzyme, its excessive consumption (more than 1.2 l / day) may cause an increase in the concentration of atorvastatin in the blood plasma (see section "Pharmacokinetics").
Transport protein inhibitors
Atorvastatin is a substrate of liver enzyme transporters (see section "Pharmacokinetics").
Co-administration of atorvastatin 10 mg and cyclosporine 5.2 mg/kg/day resulted in increased atorvastatin exposure (AUC ratio: 8.7) (see Pharmacokinetics section). Cyclosporine is an inhibitor of organic anion transport polypeptide 1B1 (OATP1B1), OATP1B3, multidrug resistance-associated protein 1 (MDR1) and breast cancer resistance protein, as well as CYP3A4, therefore increasing the exposure of atorvastatin. The daily dose of atorvastatin should not exceed 10 mg (see section "Dosage regimen").
Glecaprevir and pibrentasvir are inhibitors of OATP1B1, OATP1B3, MDR1 and breast cancer resistance protein and therefore increase exposure to atorvastatin. The daily dose of atorvastatin should not exceed 10 mg (see section "Dosage regimen").
Co-administration of atorvastatin 20 mg and letermovir 480 mg/day resulted in increased atorvastatin exposure (AUC ratio: 3.29) (see Pharmacokinetics section). Letermovir is an inhibitor of the transporters P-gp, BCRP, MRP2, OAT2 and the hepatic transporter OATP1B1/1B3, thus increasing the level of exposure to atorvastatin. The daily dose of atorvastatin should not exceed 20 mg (see section "Dosage regimen").
The magnitude of the mediated drug interaction between CYP3A and OATP1B1/1B3 on co-administration of drugs may differ when letermovir is co-administered with cyclosporine. It is not recommended to use atorvastatin in patients receiving letermovir therapy in combination with cyclosporine.
Elbasvir and grazoprevir are inhibitors of OATP1B1, OATP1B3, MDR1 and breast cancer resistance protein and therefore increase exposure to atorvastatin. It should be used with caution and at the lowest required dose (see section "Dosage regimen").
Inducers of the cytochrome CYP3A4 isoenzyme
The combined use of atorvastatin with inducers of the cytochrome CYP3A4 isoenzyme (for example, efavirenz or rifampicin or St. John's wort preparations) may lead to a decrease in the concentration of atorvastatin in the blood plasma. Due to the dual mechanism of interaction with rifampicin (an inducer of the cytochrome CYP3A4 isoenzyme and an inhibitor of the hepatocyte transport protein OATP1B1), simultaneous use of atorvastatin and rifampicin is recommended, since delayed administration of atorvastatin after taking rifampicin leads to a significant decrease in the concentration of atorvastatin in the blood plasma (see section “Pharmacokinetics”). However, the effect of rifampicin on hepatocyte concentrations of atorvastatin is unknown, and if concomitant use cannot be avoided, the effectiveness of the combination should be carefully monitored during therapy.
Antacids
Simultaneous oral administration of a suspension containing magnesium hydroxide and aluminum hydroxide reduced the concentration of atorvastatin in the blood plasma (change in AUC: 0.66), but the degree of reduction in the concentration of LDL-C did not change.
Phenazone
Atorvastatin does not affect the pharmacokinetics of phenazone, so interaction with other drugs metabolized by the same cytochrome isoenzymes is not expected.
Colestipol
With simultaneous use of colestipol, the concentration of atorvastatin in the blood plasma decreased (change in AUC: 0.74); however, the lipid-lowering effect of the combination of atorvastatin and colestipol was superior to that of each drug alone.
Digoxin
With repeated administration of digoxin and atorvastatin at a dose of 10 mg, the equilibrium concentrations of digoxin in the blood plasma did not change. However, when digoxin was used in combination with atorvastatin at a dose of 80 mg/day, digoxin concentrations increased by approximately 20%. Patients receiving digoxin in combination with atorvastatin require clinical monitoring.
Azithromycin
With simultaneous use of atorvastatin at a dose of 10 mg 1 time / day and azithromycin at a dose of 500 mg 1 time / day, the concentration of atorvastatin in plasma did not change.
Oral contraceptives
With simultaneous use of atorvastatin and oral contraceptives containing norethisterone and ethinyl estradiol, an increase in the concentrations of norethisterone (AUC change 1.28) and ethinyl estradiol (AUC change 1.19) was observed. This effect should be taken into account when choosing an oral contraceptive for a woman taking atorvastatin.
Terfenadine
With simultaneous use of atorvastatin and terfenadine, no clinically significant changes in the pharmacokinetics of terfenadine were detected.
Warfarin
In a clinical study in patients regularly receiving warfarin therapy, concomitant use of atorvastatin at a dose of 80 mg/day resulted in a slight increase in prothrombin time of approximately 1.7 seconds during the first 4 days of therapy. The indicator returned to normal within 15 days of atorvastatin therapy. Although significant interactions affecting anticoagulant function have been observed only in rare cases, the prothrombin time should be determined before initiating atorvastatin therapy in patients receiving coumarin anticoagulant therapy and frequently enough during therapy to prevent a significant change in the prothrombin time. Once the prothrombin time has stabilized, it can be monitored as recommended for patients receiving coumarin anticoagulants. When changing the dose of atorvastatin or discontinuing therapy, prothrombin time should be monitored according to the same principles as described above. Atorvastatin therapy was not associated with bleeding or changes in prothrombin time in patients not receiving anticoagulant treatment.
Colchicine
Although studies have not been conducted on the simultaneous use of colchicine and atorvastatin, there are reports of the development of myopathy when using this combination. Caution should be exercised when atorvastatin and colchicine are used concomitantly.
Amlodipine
In a drug interaction study in healthy subjects, coadministration of atorvastatin 80 mg and amlodipine 10 mg resulted in a clinically insignificant increase in atorvastatin concentrations (AUC change: 1.18).
Fusidic acid
During post-marketing studies, cases of rhabdomyolysis have been reported in patients taking concomitant statins, including atorvastatin and fusidic acid. The mechanism of this interaction is unknown. In patients for whom the use of fusidic acid is considered necessary, statin treatment should be discontinued for the duration of use of fusidic acid. Statin therapy can be resumed 7 days after the last dose of fusidic acid. In exceptional cases where long-term systemic therapy with fusidic acid is necessary, for example, for the treatment of severe infections, the need for combined use of atorvastatin and fusidic acid should be considered on a case-by-case basis and under close medical supervision. The patient should seek immediate medical attention if symptoms of muscle weakness, tenderness, or pain occur.
Other concomitant therapy
In clinical studies, atorvastatin was used in combination with antihypertensive agents and estrogens as part of hormone replacement therapy. There were no signs of clinically significant adverse interactions; No interaction studies with specific drugs have been conducted.
In addition, an increase in the concentration of atorvastatin was observed when used simultaneously with HIV protease inhibitors (combinations of lopinavir and ritonavir, saquinavir and ritonavir, darunavir and ritonavir, fosamprenavir, fosamprenavir with ritonavir and nelfinavir), hepatitis C protease inhibitors (boceprevir, elbasvir/grazoprevir, simeprevir) , clarithromycin and itraconazole. Caution should be exercised when using these drugs together and the lowest effective dose of atorvastatin should be used.