pharmachologic effect
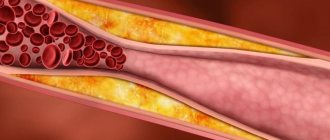
Belongs to the group of statins and has a lipid-lowering effect . Inhibits selectively and competitively the enzyme involved in cholesterol .
Triglycerides and cholesterol become components of atherogenic lipoproteins in the liver, after which they are transported to the periphery by the blood. By interacting with lipoprotein , they are converted into these lipoproteins.
Due to inhibition of HMG-CoA reductase, the level of lipoproteins and cholesterol in the blood decreases. The synthesis of LDL decreases and the activity of their receptors increases.
The drug is able to reduce the amount of LDL in cases of homozygous hereditary hypercholesterolemia
The medicine reduces cholesterol levels by 30-46%, atherogenic lipoproteins by 41-61%, triglycerides by 14-33% and increases the content of lipoproteins with antiatherogenic properties.
Pharmacological properties of the drug Torvacard
Atorvastatin is a selective competitive inhibitor of methylglutaryl-coenzyme A (HMG-CoA) reductase, an enzyme that regulates the rate of conversion of HMG-CoA to mevalonate, a precursor of sterols (including cholesterol). In patients with homo- and heterozygous hereditary hypercholesterolemia, non-hereditary forms of hypercholesterolemia and mixed dyslipidemia, the use of atorvastatin reduces the total level of cholesterol, LDL cholesterol and apolipoprotein B. Atorvastatin also reduces the concentration of VLDL and TG. The drug reduces the level of cholesterol and lipoproteins in the blood plasma by inhibiting HMG-CoA reductase, cholesterol synthesis in the liver and increasing the number of LDL receptors on the surface of hepatocytes, which enhances the uptake and catabolism of LDL. Atorvastatin is rapidly absorbed after oral administration; the maximum concentration in the blood plasma is achieved after 1–2 hours. The rate of absorption and concentration in the blood plasma increase in proportion to the dose of the drug. The absolute bioavailability of atorvastatin is about 12%, and the systemic availability of HMG-CoA reductase inhibitory activity is about 30%. Atorvastatin is metabolized into ortho- and parahydroxylated derivatives and various β-oxidation products. In vitro, inhibition of HMC-CoA reductase by ortho- and para-hydroxyl metabolites is equivalent to inhibition by atorvastatin. Approximately 70% of the circulating inhibitory activity of HMG-CoA reductase belongs to the active metabolites. In vitro studies indicate the importance of hepatic metabolism of atorvastatin by cytochrome P450 3A4, corresponding to increased plasma concentrations of atorvastatin in people concomitantly receiving erythromycin, which is a known isoenzyme inhibitor. In vitro studies have also shown that atorvastatin is a weak inhibitor of cytochrome P450 3A4. The simultaneous use of atorvastatin and terfenadine, a compound that is mainly metabolized by cytochrome P450 3A4, did not significantly increase the concentration of terfenadine in the blood plasma. Therefore, it is unlikely that atorvastatin will significantly alter the pharmacokinetics of other cytochrome P450 3A4 substrates. Atorvastatin and its metabolites are partially excreted in bile after hepatic and extrahepatic metabolism. However, the drug probably does not pass through enterohepatic recirculation. The average half-life of atorvastatin from human plasma is about 14 hours. The half-life of the inhibitory activity of HMG-CoA reductase is approximately 20–30 hours due to the presence of active metabolites. Less than 2% of an oral atorvastatin dose is excreted in the urine.
Pharmacodynamics and pharmacokinetics
In the blood, the maximum concentration of the drug occurs within 60-120 minutes. Eating reduces the duration of absorption, but the reduction in cholesterol is comparable to that without food. When used in the evening, the concentration of the drug is lower than when taken in the morning.
98% bound to blood proteins. Metabolized in the liver to form active metabolites.
It is excreted in bile, the half-life is 14 hours. The effectiveness of the drug is maintained due to active metabolites for up to 30 hours. It is not excreted during hemodialysis.
Torvacard overdose, symptoms and treatment
There is no specific treatment for atorvastatin overdose. In case of overdose, symptomatic and supportive therapy is carried out (gastric lavage, administration of activated charcoal or laxatives). If myopathy is noted with the further development of rhabdomyolysis and acute renal failure (a rare but serious side effect), immediate discontinuation of the drug and the administration of diuretics and sodium bicarbonate are required. Rhabdomyolysis can lead to hyperkalemia; in this case, intravenous administration of calcium chloride or calcium gluconate, infusion of glucose with insulin, and ion exchange agents are necessary to normalize potassium metabolism. Since atorvastatin binds to plasma proteins, hemodialysis does not lead to a significant decrease in the concentration of the drug in the blood plasma.
Indications for use of Torvacard
Torvacard tablets - what are they for?
The medicine is used in combination with a diet for:
- reducing the level of cholesterol , atherogenic lipoproteins, triglycerides, apolipoprotein B and increasing the amount of HDL in hypercholesterolemia, heterozygous and combined hypercholesterolemia (types IIa and IIb according to Fredrickson);
- treatment of patients who have increased triglycerides in the blood (Fredrickson type IV) and Fredrickson type III (dysbetalipoproteinemia), if the diet does not bring results;
- reducing the amount of cholesterol and LDL in homozygous familial hypercholesterolemia ;
- treatment of heart and vascular diseases in the presence of increased factors for coronary heart disease ( arterial hypertension , patients over 55 years of age, history of stroke albuminuria , left ventricular hypertrophy, smoking, peripheral vascular disease, family history of coronary artery disease diabetes mellitus ).
The most common indications for the use of Torvacard are secondary prevention of myocardial infarction , death, revascularization , stroke due to dyslipidemia .
Contraindications
- severe liver damage;
- increased levels of transaminases in the blood;
- hereditary glucose and lactose intolerance, lactase deficiency;
- women of reproductive age who do not use contraception ;
- pregnancy and breastfeeding ;
- children under 18 years of age;
- individual intolerance.
Use cautiously for metabolic and metabolic disorders, arterial hypertension , alcoholism , past liver disease, sepsis , changes in water-electrolyte balance, diabetes , epilepsy , trauma and major operations.
Contraindications to the use of Torvacard
Hypersensitivity to any component of the drug; acute liver disease; liver failure; increased level of liver transaminases in the blood serum (more than 3 times); During pregnancy and breastfeeding. Due to the lack of experience in treating children with atorvastatin, it should be prescribed only by specialists for the treatment of serious forms of hypercholesterolemia in children, as well as homozygous forms of hereditary hypercholesterolemia, especially in the presence of a high risk of developing early atherosclerosis and its clinical complications.
Side effects
Nervous system: insomnia, headache, depression , sleep disorders , paresthesia , ataxia , neuropathies .
Digestive tract: stomach pain, dyspepsia , nausea and vomiting, stool disorders, changes in appetite, pancreatitis and hepatitis , jaundice .
Musculoskeletal system: pain in the joints and muscles, in the back, cramps in the leg muscles, myositis .
Allergic manifestations: urticaria , itching, anaphylactic shock , erythema multiforme, angioedema , Lyell's syndrome.
Laboratory abnormalities: changes in glucose , increased activity of liver enzymes and creatine phosphokinase in the blood.
Other manifestations may include swelling of peripheral tissues, chest pain, tinnitus, baldness, weakness, weight gain, impotence , secondary renal failure, and a decrease in platelet count.
Cholesterol pills in some cases led to depression , sexual dysfunction, rare cases of damage to the connective tissue of the lungs, and diabetes mellitus (development depends on risk factors - fasting glucose levels, arterial hypertension, body mass index, hypertriglyceridemia ).
Side effects of the drug Torvacard
The most common side effects (1% or more) noted during treatment with Torvacard were: general: headache, asthenia, abdominal pain, allergic reactions, back pain, chest pain, general fatigue; Gastrointestinal tract: dyspepsia, nausea, vomiting, anorexia, hepatitis, pancreatitis, cholestatic jaundice, flatulence, constipation, diarrhea; CNS: myalgia, paresthesia, peripheral neuropathy, dizziness, amnesia; musculoskeletal system: myalgia, myositis, myopathy, arthralgia, rhabdomyolysis; skin and mucous membranes: itching, alopecia, vesicular rash, urticarial rash, erythema multiforme, toxic epidermal necrolysis, Stevens-Johnson syndrome; genitourinary system: erectile dysfunction; metabolic and nutritional disorders: hypoglycemia, hyperglycemia, peripheral edema/edema, weight gain; hematological and lymphatic systems: thrombocytopenia.
Instructions for use of Torvacard (Method and dosage)
During treatment, the patient must follow a lipid-lowering diet .
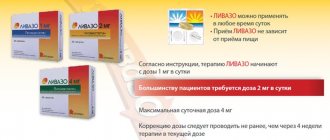
Therapy begins with 10 mg per day, subsequently increased to 20 mg. The daily therapeutic dose is from 10 to 80 mg. The dose is selected taking into account laboratory parameters and individual characteristics.
The drug is taken regardless of food.
Before starting treatment and if dose adjustment is necessary, laboratory monitoring of lipid levels is carried out.
The effect of use occurs after 14 days.
For the treatment of patients with homozygous hypercholesterolemia , one of the few drugs that has an effect is Torvacard; the instructions for use clearly define the daily dose, which is 80 mg.
Interaction
The use of drugs that inhibit metabolism mediated by the CYP450 enzyme, erythromycin , antifungal and immunosuppressive drugs, fibrates, cyclosporine , clarithromycin , nicotinamide , nicotinic acid , the concentration of Torvacard in the blood increases. This increases the likelihood of myopathy, so it is necessary to monitor the level of CPK in the blood.
Co-administration of products with aluminum hydroxide or magnesium reduces the concentration of Torvacard, but this does not affect the effectiveness.
The combination with colestipol reduces the concentration of atorvastatin , but their combined lipid-lowering effect is superior to each individually.
Cimetidine , C pyronolactone , ketoconazole increases the likelihood of a decrease in the level of steroid hormones.
Taking oral contraceptives and a daily dose of Torvacard 80 mg increases the content of ethinyl estradiol in the blood.
Use in combination with digoxin reduces the concentration of the latter by 20%.
Interactions of the drug Torvacard
The risk of myopathy as a side effect of statins is higher with simultaneous use of: cyclosporine, fibric acid and its derivatives, macrolide antibiotics, antimycotic azoles or niacin. Amlodipine : with simultaneous use of 80 mg of atorvastatin and 10 mg of amlodipine, no changes in the pharmacokinetics of Torvacard were detected. Antipyrine: Since Torvacard does not alter the pharmacokinetics of antipyrine, interactions between other drugs metabolized by cytochrome are unlikely. Erythromycin/clarithromycin : simultaneous use of atorvastatin and erythromycin (500 mg 4 times a day) or clarithromycin (500 mg 2 times a day), known inhibitors of cytochrome P450 3A4, led to an increase in the plasma concentration of atorvastatin. Digoxin: Concomitant repeated administration of digoxin and atorvastatin 10 mg did not change the plasma concentration of digoxin at steady state. However, digoxin concentrations increased by approximately 20% when digoxin was coadministered with atorvastatin 80 mg once daily. It is necessary to monitor patients receiving Torvacard and digoxin in order to adjust the dose of digoxin. Oral contraceptives: Concomitant use of oral contraceptives containing norethisterone and ethinyl estradiol increased the AUC value of norethisterone by approximately 30% and ethinyl estradiol by 20%. This increase in concentration must be taken into account when choosing oral contraceptives for women receiving Torvacard. Cholestipol: Plasma concentrations of atorvastatin decreased with simultaneous use of atorvastatin and cholestipol (by approximately 25%), with a more pronounced lipid-lowering effect than with one drug alone. Antacids: When antacids containing magnesium and aluminum hydroxide were taken simultaneously with Torvacard, the plasma concentrations of atorvastatin and its active metabolites decreased by approximately 35%, but the decrease in LDL cholesterol levels did not change. Warfarin: Comparative interaction studies between warfarin and atorvastatin did not reveal any clinically significant interactions. Phenazone: Since atorvastatin does not affect the pharmacokinetics of phenazone, there are no interactions with other drugs metabolized through the same cytochrome isoenzymes. Cimetidine: When studying the combined use of cimetidine and atorvastatin, no interaction was observed. Azithromycin: The plasma concentration of atorvastatin is not affected by the simultaneous use of atorvastatin (10 mg once daily) and azithromycin (500 mg once daily). Terfenadine: Concomitant use of atorvastatin and terfenadine did not cause a clinically significant effect on the pharmacokinetics of terfenadine. Protease inhibitors: simultaneous use of atorvastatin with protease inhibitors that inhibit the effect of cytochrome P450 3A4 is accompanied by an increase in the concentration of atorvastatin in the blood plasma. Concomitant therapy: During clinical studies, Torvacard was used concomitantly with antihypertensive agents and estrogen replacement drugs without significant interaction effects. Interaction with specific agents has not been studied.
special instructions
Before starting treatment, you should try to reduce cholesterol levels with diet, treatment of obesity and associated diseases, and increased physical activity.
During treatment, monitoring of AST and ALT levels is necessary. For the first time, monitoring is carried out before, 6 weeks and 3 months after the start of therapy, as well as after adjusting the dose and once every six months. If the enzyme level increases more than 3 times, the drug is discontinued.
Taking Torvacard can cause weakness and muscle pain ( myopathy ) and an increase in CPK in the blood. If muscle pain or weakness occurs in combination with a fever, you should consult a doctor.
The drug is discontinued if there is a risk of renal failure due to rhabdomyolysis . This may include trauma, major surgery, metabolic and electrolyte imbalance, arterial hypotension , severe infection, and convulsions .
Taking Torvacard may lead to the development of diabetes mellitus in patients who are at increased risk. But it is worth remembering that the benefits of taking statins are higher than the risk of diabetes, so there is no need to discontinue the drug, and patients at risk should be constantly under the supervision of a doctor.
Torvacard, 90 pcs., 20 mg, film-coated tablets
Effect of drugs on atorvastatin when used simultaneously
Atorvastatin is metabolized by the cytochrome P450 isoenzyme CYP3A4 and is a substrate for transport proteins, such as the hepatic uptake transporter OATP1B1. Concomitant use of drugs that are inhibitors of the CYP3A4 isoenzyme or transport proteins may lead to an increase in the concentration of atorvastatin in the blood plasma and an increased risk of myopathy. The risk may also be increased when atorvastatin is used concomitantly with other drugs that can cause myopathy, such as fibric acid derivatives and ezetimibe.
Inhibitors of the CYP3A4 isoenzyme. It has been shown that potent inhibitors of the CYP3A4 isoenzyme lead to a significant increase in plasma concentrations of atorvastatin. If possible, avoid the simultaneous use of strong inhibitors of the CYP3A4 isoenzyme (for example, cyclosporine, telithromycin, clarithromycin, delavirdine, stiripentol, ketoconazole, voriconazole, itraconazole, posaconazole and HIV protease inhibitors, including ritonavir, lopinavir, atazanavir, indinavir, darunavir, etc.) . In cases where concomitant use of these drugs and atorvastatin cannot be avoided, lower initial and maximum doses of atorvastatin are recommended. When using a daily dose of Torvacard® more than 40 mg, it is recommended to conduct careful clinical monitoring of the patient's condition.
Moderate inhibitors of the CYP3A4 isoenzyme (for example, erythromycin, diltiazem, verapamil and fluconazole) may increase the plasma concentration of atorvastatin. An increased risk of myopathy is observed when erythromycin is used in combination with HMG-CoA reductase inhibitors (statins).
Drug interaction studies evaluating the effect of amiodarone or verapamil on atorvastatin have not been conducted. Both amiodarone and verapamil are known to inhibit CYP3A4 activity, and coadministration with atorvastatin may result in increased plasma concentrations of atorvastatin. Therefore, a lower maximum dose of atorvastatin should be prescribed and appropriate clinical monitoring of the patient's condition should be carried out when used concomitantly with moderate inhibitors of the CYP3A4 isoenzyme. Close clinical monitoring is recommended after initiation of therapy or during dose titration of the inhibitor.
Grapefruit juice. Contains 1 or more components that inhibit the CYP3A4 isoenzyme and may increase the plasma concentration of drugs metabolized by the CYP3A4 isoenzyme. Drinking one glass of grapefruit juice (240 ml) also resulted in a 20.4% reduction in AUC for the active orthohydroxy metabolite. Large volumes of grapefruit juice (more than 1.2 L per day for 5 days) increased the AUC of atorvastatin by 2.5 times and the AUC of active (atorvastatin and metabolites). The combined use of large volumes of grapefruit juice and Torvacard® is not recommended.
Inducers of the CYP3A4 isoenzyme. Concomitant use of atorvastatin with inducers of the cytochrome P450 isoenzyme CYP3A4 (for example, efavirenz, rifampicin, St. John's wort) can lead to various decreases in the concentration of atorvastatin in the blood plasma. Due to the dual mechanism of interaction of rifampicin (induction of the CYP3A4 isoenzyme and inhibition of the hepatic uptake transporter OATP1B1), simultaneous administration of atorvastatin and rifampicin is recommended, since delayed administration of atorvastatin after administration of rifampicin was accompanied by a significant decrease in the concentration of atorvastatin in the blood plasma. There are no data yet on the effect of rifampicin on the concentration of atorvastatin in hepatocytes, and if concomitant therapy cannot be avoided, the patient should be carefully monitored to monitor the effectiveness of the drug.
Transport protein inhibitors. Transport protein inhibitors (eg, cyclosporine) may increase the systemic exposure of atorvastatin. The effect of inhibition of hepatic uptake transport proteins on atorvastatin concentrations in hepatocytes is unknown. If concomitant therapy cannot be avoided, the dose of atorvastatin should be reduced and the patient's condition should be closely monitored to achieve the therapeutic goal.
Gemfibrozil/fibric acid derivatives. Monotherapy with fibrates is sometimes accompanied by the occurrence of adverse effects from skeletal muscles, incl. rhabdomyolysis. The risk of these effects may therefore be increased when fibric acid derivatives are combined with atorvastatin. If concomitant therapy cannot be avoided, the lowest dose of atorvastatin should be used and the patient's condition should be closely monitored.
Ezetimibe. Monotherapy with ezetimibe is accompanied by the occurrence of adverse events from skeletal muscles, incl. rhabdomyolysis. The risk of these events may therefore be increased with concomitant therapy with ezetimibe and atorvastatin. If concomitant therapy cannot be avoided, the lowest dose of atorvastatin should be used and the patient's condition should be closely monitored.
Colestipol. Plasma concentrations of atorvastatin and its active metabolites were lower (by approximately 25%) when colestipol and atorvastatin were co-administered. However, the effect on lipids was greater with combination therapy with atorvastatin and colestipol than with either drug alone.
Fusidic acid. Drug interaction studies between atorvastatin and fusidic acid have not been conducted. As with other statins, skeletal muscle adverse events, including rhabdomyolysis, have been reported during post-marketing use of atorvastatin with fusidic acid. The mechanism of this interaction is unknown. Patients should be carefully monitored and, if possible, temporary discontinuation of co-treatment with these drugs should be considered.
The effect of atorvastatin on concomitant drug therapy
Digoxin. With repeated doses of digoxin and atorvastatin at a dose of 10 mg, Css of digoxin increased slightly. Patients taking digoxin should be under appropriate medical supervision.
Oral contraceptives. Concomitant use of atorvastatin and oral contraceptives led to increased plasma concentrations of norethisterone and ethinyl estradiol. This effect should be taken into account when choosing an oral contraceptive for women receiving Torvacard®.
Warfarin. In a clinical study conducted in patients receiving long-term warfarin, concomitant use of atorvastatin 80 mg daily and warfarin caused a slight decrease in PT (approximately 1.7 s) during the first 4 days of treatment, which returned to normal within 15 days of atorvastatin therapy.
Although clinically significant anticoagulant interactions have been very rarely reported, the PT should be determined in patients taking coumarin anticoagulants before initiating therapy and regularly during initiation of atorvastatin therapy to ensure that there is no significant change in PT. Once a stable PT value has been established, it can be monitored at standard intervals recommended for patients receiving coumarin anticoagulants. If the dose of atorvastatin is changed or discontinued, the same procedure should be repeated. Atorvastatin therapy was not associated with bleeding or changes in PT in patients not taking anticoagulants.
With the simultaneous use of atorvastatin and antacid drugs containing magnesium and aluminum hydroxides, the concentration of atorvastatin in the blood plasma decreased by approximately 35%, but the degree of reduction in the concentration of cholesterol/LDL did not change.
Effect of drugs on the pharmacokinetics of atorvastatin during concomitant use
Concomitantly used drugs and dosage regimen Atorvastatin Dose, mg Change in AUC* Clinical recommendations Tipranavir, 500 mg 2 times a day / Ritonavir, 200 mg 2 times a day, 8 days (14-21st) 40 mg on day 1, 10 mg on the 20th day ↑ 9.4 times In cases where simultaneous use with atorvastatin is necessary, do not exceed the daily dose of atorvastatin more than 10 mg. Clinical monitoring of these patients is recommended Cyclosporine, 5.2 mg/kg/day, stable dose 10 mg once daily for 28 days ↑ 8.7 times Lopinavir, 400 mg twice daily/Ritonavir, 100 mg twice daily day, 14 days 20 mg 1 time per day 2 for 4 days ↑ 5.9 times In cases where simultaneous use with atorvastatin is necessary, the use of the smallest maintenance doses of atorvastatin is recommended. At a dose above 20 mg, clinical monitoring of the condition of these patients is recommended Clarithromycin, 500 mg 2 times a day, 9 days 80 mg 1 time a day for 8 days ↑ 4.4 times Saquinavir, 400 mg 2 times a day / Ritonavir (300 mg 2 times per day, on days 5-7, increase to 400 mg 2 times a day on day 8), days 5-18 40 mg 1 time for 4 days ↑ 3.9 times In cases where simultaneous use with atorvastatin is necessary, the use of the lowest maintenance doses of atorvastatin is recommended.
30 minutes after taking atorvastatin
Darunavir 300 mg 2 times a day / Ritonavir 100 mg 2 times a day, 9 days 10 mg 1 time a day 4 days ↑ 3.3 times For doses above 40 mg, clinical monitoring of the condition of these patients is recommended Itraconazole 200 mg 1 time day, 4 days 40 mg once ↑ 3.3 times Fozamprenavir 700 mg 2 times a day/Ritonavir 100 mg 2 times a day, 14 days 10 mg 1 time a day 4 days ↑ 2.5 times Fosamprenavir 1400 mg 2 times per day, 14 days 10 mg once a day 4 days ↑ 2.3 times Nelfinavir 1250 mg 2 times a day, 14 days 10 mg once a day 28 days ↑ 1.7 times*** No special recommendations Grapefruit juice, 240 ml once a day** 40 mg once a day ↑ by 37% The combined use of large quantities of grapefruit juice and atorvastatin is not recommended Diltiazem 240 mg once a day, 28 days 40 mg once a day ↑ by 51% After initiation of treatment or dose adjustment diltiazem, appropriate clinical monitoring of these patients is recommended Erythromycin 500 mg 4 times a day, 7 days 10 mg once ↑ by 33%*** The use of the lowest maximum dose and clinical monitoring of these patients is recommended Amlodipine 10 mg, once 80 mg once ↑by 18% No special recommendations Cimetidine 300 4 times a day, 2 weeks 10 mg 1 time a day 4 weeks ↓ less than 1%*** No special recommendations Suspensions of antacids containing magnesium and aluminum hydroxides 30 ml 4 times a day, 2 weeks 10 mg once daily for 4 weeks ↓ by 35% No special recommendations Efavirenz 600 mg once daily for 14 days 10 mg once daily for 3 days ↓ by 41% No special recommendations Rifampicin 600 mg once daily for 7 days (simultaneous administration) 40 mg once a day ↑ by 30% If concomitant therapy cannot be avoided, simultaneous use of rifampicin with atorvastatin under clinical monitoring is recommended Rifampicin 600 mg once a day for 5 days (separate doses) 40 mg once a day ↓ by 80% Gemfibrozil 600 mg twice a day day, 7 days 40 mg once ↑ by 35% The use of the lowest initial dose and clinical monitoring of these patients is recommended Fenofibrate 160 mg once a day, 7 days 40 mg once ↑ by 3% The use of the lowest initial dose and clinical monitoring of these patients is recommended
*Data reported as fold change represent the simple ratio between concomitant use and atorvastatin monotherapy (ie, 1 time = no change). Data reported as percentage change reflect the percentage difference relative to atorvastatin monotherapy (ie, 0% = no change).
**Contains 1 or more components that inhibit the CYP3A4 isoenzyme and may increase the plasma concentration of drugs metabolized by the CYP3A4 isoenzyme. Drinking one glass of grapefruit juice (240 ml) also reduced the AUC of the active orthohydroxy metabolite by 20.4%. Large volumes of grapefruit juice (more than 1.2 L per day for 5 days) increased the AUC of atorvastatin by 2.5-fold and the AUC of active atorvastatin and metabolites.
***Total equivalent activity of atorvastatin. An increase is indicated as ↑, a decrease - ↓
Children. Drug interaction studies have been conducted in adults only. The extent of interaction in children is unknown. When treating children, the above interactions and precautions for adults should be taken into account.
Analogues of Torvacard
Level 4 ATX code matches:
Akorta
Atomax
Lipitor
Pravastatin
Simvastol
Owencore
Simgal
Tulip
Lovastatin
Liptonorm
Rozulip
Zokor
Rosart
Tevastor
Atorvastatin
Liprimar
Simvastatin
Atoris
Basilip
Rosecard
Analogues of Torvacard are presented on the market in large quantities: Zakor , Vasilip , Crestor , Lovastatin , Rovacor , Pravastatin , Rosuvastatin , Simvastatin , Atorvastatin , Liprimar , Atoris .
The price of analogues is from 120 rubles. for 30 tab. atorvastatin up to RUB 3,606. for 28 tablets of Crestor at a dose of 40 mg.
Reviews about Torvacard
Those reviews about Torvacard that are available on the forums allow us to conclude that the drug is quite effective. It is widely prescribed by cardiologists to lower cholesterol and protect patients from stroke and heart attack . After 1-2 months of use, a significant decrease in cholesterol levels is observed. Some women report a pleasant side effect: weight loss.
Among the disadvantages are that the cholesterol medicine can cause insomnia and an itchy rash on the body .
Torvacard price, where to buy
The cost of the drug in Russian pharmacies ranges from 276 to 320 rubles. for 30 tablets at a dose of 10 mg. The price of Torvacard 20 mg 90 tablets is on average 1025 rubles, and a package of 90 tablets with a dose of 40 mg costs 1286 rubles.
- Online pharmacies in RussiaRussia
- Online pharmacies in UkraineUkraine
- Online pharmacies in KazakhstanKazakhstan
ZdravCity
- Torvacard tablets p.p.o.
20 mg 90 pcs. Saneka Pharmaceuticals a.s. 1040 rub. order - Torvacard tablets p.p.o. 40 mg 30 pcs. SanekaSaneka Pharmaceuticals a.s.
RUR 577 order
- Torvacard tablets p.p.o. 40 mg 90 pcs. Zentiva a.s./Saneka Pharmaceuticals a.s.
RUB 1,460 order
Pharmacy Dialogue
- Torvacard (tab.p.pl/vol. 40 mg No. 90) Saneca
1420 rub. order
- Torvacard (tab.p.pl/vol. 20 mg No. 30)Zentiva ks
RUB 376 order
- Torvacard (tab.p.pl/vol. 20 mg No. 90) Saneca
RUR 978 order
- Torvacard (tablet p/o cap. 10 mg No. 90)Zentiva as/Zentiva ks
RUB 684 order
- Torvacard (tab.p.pl/vol. 10 mg No. 30) Saneca
RUB 249 order
show more
Pharmacy24
- Torvacard Crystal 20 mg N90 tablets TOV Zentiva, Czech Republic
367 UAH.order - Torvacard Crystal 40 mg N30 tablets TOV Zentiva, Czech Republic
247 UAH order
- Torvacard Crystal 10 mg N90 tablets TOV Zentiva, Czech Republic
331 UAH. order
- Torvacard Crystal 10 mg N30 tablets TOV Zentiva, Czech Republic
112 UAH order
- Torvacard Crystal 20 mg N30 tablets TOV Zentiva, Czech Republic
96 UAH order
PaniPharmacy
- Torvacard tablets Torvacard 20 tablets. p/o 20 mg No. 90, Saneca Pharmaceuticals
345 UAH. order
- Torvacard tablets Torvacard 40 tablets. p/o 40 mg No. 30, Saneca Pharmaceuticals
267 UAH order
- Torvacard tablets Torvacard 20 tablets. p/o 20 mg No. 30, Saneca Pharmaceuticals
107 UAH order
- Torvacard tablets Torvacard 10 tablets. p/o 10 mg No. 30, Saneca Pharmaceuticals
111 UAH order
show more