Instructions for use VALSACOR®
Hyperkalemia
Concomitant use with potassium supplements, potassium-sparing diuretics, salt substitutes containing potassium and other substances that may increase potassium concentrations (heparin) is not recommended. Potassium concentrations should be monitored if necessary.
Renal dysfunction
In patients with creatinine clearance <10 ml/min and patients on hemodialysis, valsartan should be used with caution due to the fact that there is currently no data on the safety of use in this category of patients. Patients with CC >10 ml/min do not require dose adjustment.
Patients with liver failure
In patients with mild to moderate hepatic impairment without cholestasis, valsartan should be prescribed with caution.
Patients with sodium and/or fluid deficiency
In patients with severe sodium deficiency and/or reduced blood volume (for example, due to taking diuretics in high doses), in rare cases, severe arterial hypotension may develop at the beginning of valsartan therapy. Before starting treatment with valsartan, it is recommended to restore the electrolytes and fluid levels in the body, in particular by reducing the doses of diuretics.
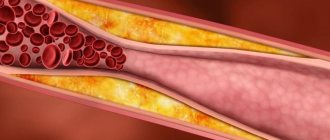
Renal artery stenosis
In patients with bilateral renal artery stenosis or renal artery stenosis of a solitary kidney, the safety of treatment with valsartan has not been established. Short-term administration of valsartan to 12 patients with secondary renovascular hypertension did not reveal significant changes in renal hemodynamics, creatinine concentrations, or blood urea nitrogen compared with patients with unilateral renal artery stenosis. However, other substances that affect the RAAS may increase blood urea and creatinine in patients with unilateral renal artery stenosis, so monitoring of renal function is recommended during treatment with valsartan.
Kidney transplant
There are currently no data on the use of valsartan in patients who have recently undergone kidney transplantation.
Primary hyperaldosteronism
Valsartan should not be prescribed to patients with primary hyperaldosteronism, because their RAAS is not active.
Aortic and mitral valve stenosis, obstructive hypertrophic cardiomyopathy
When using valsartan, as with other vasodilators, special caution should be exercised in patients suffering from aortic and mitral valve stenosis or obstructive hypertrophic cardiomyopathy.
Recent myocardial infarction
Caution should be exercised when prescribing valsartan to patients who have recently suffered a myocardial infarction. The use of valsartan in such patients may lead to some reduction in blood pressure, but discontinuation of therapy due to ongoing symptomatic hypotension is usually not required, provided the dose is adjusted according to the instructions. The combination of captopril and valsartan does not have additional clinical benefits and increases the risk of side effects. Therefore, the combination of valsartan and ACE inhibitors is not recommended. The evaluation of patients after myocardial infarction should always include an assessment of renal function.
Heart failure
In patients with heart failure, the triple combination of an ACE inhibitor, beta blocker and valsartan has no clinical benefit, increases the risk of side effects and is therefore not recommended. Caution should be exercised when prescribing valsartan to patients with this pathology. Evaluation of patients with heart failure should always include assessment of renal function. The use of valsartan in such patients may lead to some reduction in blood pressure, but discontinuation of therapy due to ongoing symptomatic hypotension is usually not required, provided the dose is adjusted according to the instructions.
In patients whose renal function may be dependent on the activity of the RAAS (for example, patients with severe congestive heart failure), oliguria and/or progressive azotemia and, in rare cases, acute renal failure and/or death have been observed during treatment with ACE inhibitors. Because valsartan is an angiotensin II antagonist, it cannot be excluded that renal dysfunction may be associated with the use of valsartan.
The risk of adverse reactions, especially hypotension, hyperkalemia and decreased renal function (including acute renal failure), may increase when Valsacor® is used in combination with ACE inhibitors. The triple combination of ACE inhibitors, mineralocorticoid receptor antagonists and valsartan is also not recommended. The use of such combinations should be carried out under specialist supervision, subject to frequent close monitoring of renal function, electrolytes and blood pressure. ACE inhibitors and angiotensin II receptor antagonists should not be used concomitantly in patients with diabetic nephropathy.
Quincke's edema
In patients receiving valsartan, angioedema was observed, which was accompanied by swelling of the larynx, glottis, which led to airway obstruction, and/or swelling of the face, lips, pharynx and/or tongue; in some of these patients, angioedema was observed previously when taking other drugs, incl. ACE inhibitors. If there are signs of developing Quincke's edema, valsartan should be stopped immediately. In such patients, its repeated use is not allowed.
Double blockade of the RAAS
Dual blockade of the RAAS is associated with an increased risk of hypotension, hyperkalemia and renal dysfunction (including acute renal failure) compared with monotherapy.
Due to dual blockade of the RAAS, the combined use of ACE inhibitors, angiotensin II receptor antagonists or aliskiren is not recommended.
Due to its absolute necessity, the prescription of dual RAAS blockade therapy should only occur under the supervision of a specialist and subject to frequent careful monitoring of renal function, electrolytes and blood pressure. Carrying out double blockade of the RAAS under the careful supervision of a specialist and mandatory monitoring of renal function, water-electrolyte balance and blood pressure is possible in patients with chronic heart failure with intolerance to aldosterone antagonists (spironolactone), who have persistence of symptoms of chronic heart failure, despite other adequate therapy .
Dual blockade of the RAAS using an ACE inhibitor, angiotensin II receptor antagonist, or aliskiren cannot be recommended in any patient, especially in patients with diabetic nephropathy.
Use in pediatrics
There is no data on the use of valsartan in children with creatinine clearance <30 ml/min and on dialysis. Patients with CC >30 ml/min do not require dose adjustment. During treatment with valsartan, renal function and serum potassium concentrations should be carefully monitored, especially in conditions that impair renal function (fever, dehydration).
As in adults, valsartan is contraindicated in children with severe liver dysfunction, biliary cirrhosis and cholestasis. There is limited experience with the use of valsartan in pediatrics in patients with moderate to severe liver dysfunction. In such patients, the dose of valsartan should not exceed 80 mg.
Excipients
Valsacor® contains lactose, therefore the drug is not recommended for patients with lactase deficiency, galactosemia or glucose-galactose malabsorption syndrome.
Impact on the ability to drive vehicles and operate machinery
There is no data on the effect on the ability to drive a car or drive potentially dangerous machinery. When driving or operating machinery, be aware that while taking valsartan there may be a risk of dizziness or fatigue.
Pharmacological properties of the drug Valsacor
The active hormone of the renin-angiotensin-aldosterone system is angiotensin II, which is formed from angiotensin I with the participation of ACE. Angiotensin II binds to specific receptors that are located on the cell membranes of various tissues. It has a whole range of physiological effects, exhibiting both direct and indirect effects on the regulation of blood pressure. As a powerful vasoconstrictor, angiotensin II has a direct pressor effect. In addition, it promotes sodium retention and aldosterone secretion. Valsartan is an oral, potent and specific angiotensin II receptor antagonist. Selectively acts on receptors of the AT1 subtype, which are responsible for the action of angiotensin II. When the concentration of angiotensin II in the blood plasma increases after blockade of AT1 receptors by valsartan, stimulation of unblocked AT2 receptors occurs, which regulate the action of AT1 receptors. Valsartan does not exhibit any agonistic activity towards AT1 receptors and has a significantly greater affinity (approximately 20,000 times) for AT1 receptors than for AT2 receptors. Valsartan does not inhibit the activity of ACE, also known as kininase II, an enzyme that converts angiotensin I into angiotensin II and catalyzes the breakdown of bradykinin. Angiotensin II antagonists do not cause cough because they do not affect the activity of ACE and do not increase the production of bradykinin and substance P. In clinical studies in which valsartan was compared with other ACE inhibitors, the incidence of dry cough in patients taking valsartan was significantly lower (P ≤0.05) than in patients using an ACE inhibitor (2.6% compared with 7.9%). In a clinical trial, dry cough was reported in 19.5% of patients taking valsartan, 19.0% of patients taking a thiazide diuretic, compared with 68.5% of patients taking an ACE inhibitor (P≤0.05). Valsartan does not bind to or block other hormonal receptors or ion channels important for the regulation of the cardiovascular system. Treatment of patients with hypertension (arterial hypertension) with valsartan helped reduce blood pressure without affecting heart rate. In most patients, the hypotensive effect develops within 2 hours after a single oral dose, and the maximum effect on blood pressure is observed after 4–6 hours and lasts 24 hours. With repeated administration of the drug at any dose, the maximum reduction in blood pressure is achieved after 2–4 weeks and persists throughout the entire treatment period. With the combined use of hydrochlorothiazide, a significant additional reduction in blood pressure occurs. Discontinuation of valsartan does not cause a sudden increase in blood pressure and other undesirable clinical events in patients. In a long-term study of the use of valsartan in patients with heart failure, it was noted that in patients taking valsartan, there was a decrease in plasma norepinephrine and brain natriuretic peptide levels compared to the initial level. Valsartan produced significant improvements in pulmonary capillary wedge pressure, systemic vascular resistance, cardiac output, and systolic blood pressure. Patients using valsartan experience a significant increase in ejection fraction and a decrease in the internal diameter of the left ventricle compared to the initial state, and a significant decrease in the severity of symptoms of heart failure, including shortness of breath, fatigue, swelling and breath sounds. Valsartan is rapidly absorbed after oral administration, but the amount absorbed varies significantly. The average absolute bioavailability of valsartan is 23%. Valsartan is characterized by multi-exponential elimination kinetics (half-life in the α phase ≤1 hour and half-life in the β phase ≈9 hours). The pharmacokinetics of valsartan in the studied dose range is linear. With repeated administration of the drug, the pharmacokinetic parameters do not change; When the drug is administered once a day, only a slight accumulation of valsartan is observed. Valsartan binds well to serum proteins (94–97%), mostly to albumin. The volume of distribution at steady state is low (≈17 l). Plasma clearance occurs relatively slowly (≈2 L/h) compared to hepatic blood flow (≈30 L/h). The drug is excreted mainly unchanged: 70% of the absorbed amount is in feces, 30% in urine. When valsartan is taken with food, AUC decreases by 48%; however, after 8 hours, the concentration of valsartan in the blood plasma is the same both when taken on an empty stomach and when taken with food. This indicates the possibility of using valsartan regardless of food intake.
Use of the drug Valsacor
AH (arterial hypertension) The recommended dose of Valsacor is 80 mg 1 time per day, regardless of the patient’s age, gender or race. The hypotensive effect is achieved after 2 weeks, and the maximum antihypertensive effect is achieved after 4 weeks of treatment. For patients who do not achieve an adequate reduction in blood pressure, the daily dose can be increased to 160 mg or supplemented with diuretic therapy. There is no need to change the dose in patients with impaired renal or hepatic function of non-biliary origin in the absence of cholestasis. Valsacor can also be taken in combination with other antihypertensive drugs. Heart failure The recommended initial dose is 40 mg 2 times a day. This dose is gradually increased to 80 mg twice daily and then to 160 mg twice daily, the highest dose the patient can tolerate. The maximum daily dose of valsartan is 320 mg. For patients who are simultaneously treated with a diuretic, it is recommended to reduce the dose of Valsacor. Post-myocardial infarction Treatment with the drug can begin 12 hours after myocardial infarction. The initial dose of Valsacor is 20 mg 2 times a day. At the beginning of treatment, it is recommended to use Valsacor 40 mg tablets with a notch on one side. After a few weeks, the dose should be gradually increased to 40, 80 and 160 mg 2 times a day, depending on the patient’s tolerance to treatment. If symptomatic hypotension or renal failure occurs, the dose should be reduced.
Interactions of the drug Valsacor
For patients after myocardial infarction, Valsacor can be taken in combination with other drugs, such as thrombolytics, acetylsalicylic acid, beta-adrenergic blockers or statins. When Valsacor is used in combination with potassium-sparing diuretics (such as spironolactone, triamterene, amiloride), potassium preparations or salt substitutes that contain potassium, an increase in the concentration of potassium in the blood serum may occur. There were no signs of clinically significant interaction between Valsacor and other drugs. In clinical studies, drugs such as cimetidine, warfarin, furosemide, digoxin, atenolol, indomethacin, hydrochlorothiazide, amlodipine, and glibenclamide were studied. Since Valsacor does not undergo significant metabolism, it is unlikely that clinically significant interactions in the form of metabolic induction or inhibition of the cytochrome P450 system will occur. Valsartan binds well to plasma proteins, but in vitro did not indicate any interactions at this level with molecules that are also highly protein bound (diclofenac, furosemide or warfarin).
Mechanism of action of drugs
Valsacor provides a long-term reduction in the resistance of vascular walls, prevents their spasms, improves myocardial contractility, and increases the volume of blood pumped by the heart. As a result, unfavorable symptoms of deficiency disappear:
- think in your ears and head;
- swelling;
- dyspnea;
- physical weakness;
- dizziness.
Valsacor N maintains normal blood pressure, reduces the likelihood of valsartan side effects, and helps hypertensive patients maintain good health. Hydrochlorothiazide in its composition has a diuretic effect, stimulates the excretion of excess sodium and chlorine.
The medicine quickly dissolves in the stomach after administration and is absorbed into the blood. The effect of one dose of tablets develops over 30–60 minutes, reaches a maximum after 4–5 hours and lasts up to a day. With regular use, Valsacor provides an increasing antihypertensive effect after 3-4 weeks - it prevents the development of high blood pressure.
About 60% of hydrochlorothiazide ingested interacts with blood proteins; in combination with valsartan, it is less bioavailable. The components of the drugs do not accumulate in the body. Metabolism occurs in the liver, then the remaining substances are excreted through the intestinal contents and through the kidneys. Disintegration and release occur approximately 9 hours after the dose of the drug.
Side effects of the drug Valsacor
During treatment with the drug, viral infections, upper respiratory tract infections, rhinitis, sinusitis, and pharyngitis often occurred (≥1%). Nervous system and mental disorders; headache, dizziness; cough; nausea, diarrhea, abdominal pain; back pain and arthralgia; hyperkalemia; fatigue. Rarely (≤1%) rash, itching, insomnia, and swelling were noted; isolated cases of hypersensitivity reactions; very rarely - renal function disorders. The frequency of side effects does not depend on the dose and period of treatment, as well as the gender, race and age of the patient.
Dosage form and composition
The medication is intended for oral administration and is available in the form of yellow film-coated tablets:
- Valsacor: contains the active substance valsartan - an antagonist of hormone receptors that provokes an increase in pressure in blood vessels, prevents the development of hypertensive attacks;
- Valsacor N80, ND160: a combination drug containing two active ingredients: valsartan and hydrochlorothiazide, has a more pronounced and long-lasting therapeutic effect, reduces blood pressure.
In addition to active compounds, pills contain auxiliary components: MCC, lactose, silicon dioxide, stabilizing and form-building additives.