Compound
One Roxer tablet contains 5, 10, 15, 20, 30 or 40 mg of rosuvastatin in the form of rosuvastatin calcium and auxiliary components:
- microcrystalline cellulose;
- lactose anhydrous;
- crospovidone;
- anhydrous colloidal silicon dioxide;
- magnesium stearate.
The shell that covers the tablets contains:
- butyl methacrylate, dimethylaminoethyl methacrylate and methyl acrylate copolymer in a ratio of 1:2:1;
- macrogol 6000;
- titanium dioxide;
- lactose monohydrate.
Release form
Roxer is available in the form of tablets coated with a white film coating, which differ in appearance depending on the concentration of the active substance in them:
- Tablets containing rosuvastatin in a dose of 5, 10 or 15 mg are round, biconvex, and chamfered. On one side there is a marking corresponding to the dose of the active substance: “5”, “10” and “15”, respectively.
- Tablets containing rosuvastatin at a dose of 20 mg are round, biconvex, with a chamfer.
- Tablets containing rosuvastatin at a dose of 30 mg are biconvex, capsule-shaped and scored on both sides.
- Tablets containing rosuvastatin at a dose of 40 mg are biconvex and capsule-shaped.
On the cut of the tablet, two layers are clearly visible, the inner one is white.
Use during pregnancy and breastfeeding
Roxera® is contraindicated during pregnancy and lactation.
Women of reproductive age should use adequate methods of contraception.
Since cholesterol and substances synthesized from cholesterol are important for fetal development, the potential risk of inhibiting HMG-CoA reductase to the fetus outweighs the benefit of using the drug during pregnancy.
If pregnancy occurs during therapy, use of the drug should be discontinued immediately.
There is no data on the excretion of rosuvastatin in breast milk (it is known that other HMG-CoA reductase inhibitors can be excreted in breast milk), therefore the use of the drug must be discontinued during breastfeeding.
pharmachologic effect
The pharmacological action of the drug Roxera is aimed at:
- Suppression of the activity of the microsomal enzyme hydroxymethylglutaryl-CoA reductase , which acts as a catalyst for the rate-limiting early stage of cholesterol .
- Normalization of lipid profile indicators ( hypolipidemic effect ) by reducing the concentration of total cholesterol , triglycerides , lipoproteins the blood , as well as increasing the concentration of lipoproteins .
The medicine belongs to the pharmacological group “ Statins ”.
Pharmacodynamics and pharmacokinetics
Once in the body, rosuvastatin provokes the following effects:
- Helps reduce elevated concentrations of low-density lipoprotein cholesterol ;
- Helps reduce elevated concentrations of total cholesterol ;
- Helps reduce elevated triglyceride concentrations;
- Helps increase high-density lipoprotein cholesterol ;
- Helps reduce the concentration of low-density lipoprotein apolipoprotein ( apoliprotein B );
- Helps reduce the concentration of low-density lipoprotein cholesterol ;
- Helps reduce the concentration of very low density lipoprotein cholesterol ;
- Helps reduce the concentration of very low density lipoprotein triglycerides ;
- Helps increase the concentration of plasma apoliprotein A1 ;
- Reduces the ratio of low-density lipoprotein to high-density lipoprotein cholesterol ;
- Reduces the ratio of total cholesterol to high-density lipoprotein cholesterol ;
- Reduces the ratio of low-density lipoprotein cholesterol to high-density lipoprotein cholesterol;
- Reduces the ratio of low-density lipoprotein apolipoprotein ( apoliprotein B ) to apolipoprotein A1 .
A pronounced clinical effect from the use of Roxera develops a week after the start of treatment with the drug. Approximately 90% of the maximum effect of therapy is observed after two weeks.
It usually takes four weeks to achieve maximum effect, after which it is maintained throughout the subsequent treatment period.
The maximum plasma concentration of rosuvastatin is observed five hours after taking the tablet; the absolute bioavailability rate is 20%.
Rosuvastatin is extensively biotransformed in the liver , which is the primary center that synthesizes cholesterol and metabolizes low-density lipoprotein cholesterol .
The distribution index of the substance is approximately 134 l. About 90% of rosuvastatin binds to plasma proteins (mainly albumin ).
Rosuvastatin is metabolized to a limited extent (about 10%). studies metabolism using human hepatocytes have shown that it is subject to only minimal metabolism based on the cytochrome P450 enzyme system . Moreover, this metabolism cannot be considered clinically important.
The main isoenzyme involved in the metabolism of rosuvastatin is CYP 2C9. To a slightly lesser extent, isoenzymes 2C19, 3A4 and 2D6 take part in the process.
During the metabolization process, two main metabolites :
- N-desmethyl;
- lactone.
N-desmethyl is characterized by approximately half the activity compared to rosuvastatin . As for lactone , it is considered a clinically inactive form.
Rosuvastatin has more than 90% inhibitory activity against hydroxymethylglutaryl-CoA reductase (HMG-CoA reductase), which circulates in the human body in the general bloodstream.
Most of the rosuvastatin (approximately 90%) is excreted unchanged in the intestinal . In this case, both absorbed and unabsorbed active substances are excreted.
The remainder of rosuvastatin is excreted by the kidneys along with urine (approximately 5% unchanged).
The half-life of the substance is about 20 hours and does not depend on increasing the dose of the drug. The average clearance from blood plasma is about 50 liters per hour. The indicator of variability relative to the average value (coefficient of variation) is 21.7%.
As with other drugs that inhibit the activity of hydroxymethylglutaryl-CoA reductase , the uptake of rosuvastatin promotes the recruitment of the membrane transporter OATP-C, which plays an important role in the process of excretion of the substance from the liver .
Rosuvastatin is characterized by dose-dependent systemic exposure, which increases in proportion to the dose of the substance.
Repeated daily use of the drug does not provoke any changes in the pharmacokinetic characteristics of its active substance.
The patient's age and gender do not affect the pharmacokinetics of the drug. However, studies have shown that in patients of the Mongoloid race, the AUC and maximum plasma concentration of rosuvastatin are approximately twice as high as in patients belonging to the Caucasian race.
For Indians, similar indicators exceed those for Caucasians by approximately 1.3 times. There are no clinically significant differences in indicators for representatives of the Negroid race and Caucasians.
In patients with mild or moderate renal failure plasma N-desmethyl
In severe forms of renal failure, the highest plasma concentration of rosuvastatin increases approximately threefold, and the highest plasma concentration of N-desmethyl increases by approximately nine times compared to the values observed in healthy volunteers.
Plasma concentrations of rosuvastatin in patients on hemodialysis were approximately twice as high as those in healthy volunteers.
In liver failure caused by chronic alcoholic liver diseases, plasma concentrations of rosuvastatin are moderately increased.
In patients whose disease is class A on the Child-Pugh scale , the highest plasma of rosuvastatin and the AUC are increased by 60 and 5%, respectively, compared with patients liver is healthy.
If the liver belongs to category B on the Child-Pugh scale , the indicators increase by 100 and 21%, respectively. For patients whose disease belongs to category C, there are no data, which is due to the lack of experience with the use of rosuvastatin for them.
Pharmacodynamics
The drug Roxera® is a hypolipidemic agent. The active ingredient of the drug, rosuvastatin, is a selective, competitive inhibitor of HMG-CoA reductase, an enzyme that converts 3-hydroxy-3-methylglutaryl coenzyme A into mevalonic acid, a cholesterol precursor. The main target of rosuvastatin is the liver, where cholesterol (C) synthesis and LDL catabolism occur. Increases the number of hepatic LDL receptors on the cell surface, increasing the uptake and catabolism of LDL, which in turn leads to inhibition of VLDL synthesis, thereby reducing the total amount of LDL and VLDL. Rosuvastatin reduces elevated plasma concentrations of LDL cholesterol (LDL-C), total cholesterol, triglycerides (TG), and increases the concentration of high-density lipoprotein cholesterol (HDL-C). It also reduces the concentration of apolipoprotein B (ApoB), non-HDL-C, VLDL-C, VLDL-TG and increases the concentration of apolipoprotein AI (ApoA-1) in the blood plasma.
Rosuvastatin reduces the ratio of LDL-C/HDL-C, total cholesterol/HDL-C and non-HDL-C/HDL-C and the ApoB/ApoA-1 ratio. The therapeutic effect develops within one week after the start of therapy, after 2 weeks of treatment it reaches 90% of the maximum possible effect. The maximum therapeutic effect is usually achieved by the 4th week of therapy and is maintained with further regular use of the drug.
Clinical effectiveness
Rosuvastatin is effective in adult patients with hypercholesterolemia with or without concomitant hypertriglyceridemia, regardless of race, gender or age, incl. in patients with diabetes mellitus or familial hypercholesterolemia.
In 80% of patients with Fredrickson type IIa and IIb hypercholesterolemia (average initial LDL-C concentration of approximately 4.8 mmol/l), while taking rosuvastatin at a dose of 10 mg, the LDL-C concentration reaches values of less than 3 mmol/l. In patients with homozygous familial hypercholesterolemia, rosuvastatin was used in doses of 20–40 mg, with an average reduction of 22%. An additive effect is observed in combination with fenofibrate in relation to TG content and with nicotinic acid in lipid-lowering doses in relation to HDL-C concentration.
Indications for use
Rocker shown:
- For the treatment of patients suffering from primary type hypercholesterolemia (including familial hypercholesterolemia type II-A Fredrickson ) or dyslipidemia (type II-b). It is advisable to prescribe the drug when the expected therapeutic effect cannot be achieved by prescribing non-drug treatment methods: diet, correction of the patient’s weight, physical exercise, etc.
- For the treatment of patients diagnosed with familial homozygous hypercholesterolemia . Roxera is prescribed as an addition to therapy, the purpose of which is to lower lipid , as an addition to the diet, and also in cases where previously prescribed treatment does not produce positive results.
- For the treatment of patients diagnosed with atherosclerosis . The drug is used as a supplement to the prescribed diet to slow the progression of the disease, as well as to reduce total cholesterol and low-density lipoprotein cholesterol to the required level.
- As a prophylactic agent to prevent the development of complications of heart and vascular in patients with a predisposition to the development of atherosclerotic vascular lesions .
Nosological classification (ICD-10)
- E78.0 Pure hypercholesterolemia
- E78.1 Pure hyperglyceridemia
- E78.2 Mixed hyperlipidemia
- E78.5 Hyperlipidemia, unspecified
- I10 Essential (primary) hypertension
- I15 Secondary hypertension
- I21 Acute myocardial infarction
- I25.9 Chronic ischemic heart disease, unspecified
- I64 Stroke not specified as hemorrhage or infarction
- I70 Atherosclerosis
- Z72.0 Tobacco use
- Z82.4 Family history of coronary heart disease and other diseases of the cardiovascular system
Contraindications
Contraindications to the use of Roxera tablets containing rosuvastatin in doses of 5, 10 and 15 mg are:
- hypersensitivity to one or more components of the drug;
- active forms of liver pathologies (including diseases of unknown origin), as well as conditions characterized by a sustained increase in the level of liver transaminases , and conditions in which any of the liver transaminases increases at least three times;
- kidney pathologies , in which creatinine does not exceed 30 ml/min;
- chronic progressive hereditary neuromuscular diseases , which are characterized by primary muscle damage ( myopathies );
- simultaneous use of the antidepressant Cyclosporine ;
- the patient is diagnosed with an increased risk of developing myotoxic complications ;
- lactose intolerance ;
- lactase deficiency;
- glucose-galactose malabsorption;
- pregnancy (also the drug is not prescribed to women of reproductive age if they do not use contraceptives );
- lactation;
- age up to 18 years.
Tablets with a dosage of rosuvastatin 30 and 40 mg are contraindicated:
- patients with hypersensitivity to one or more components of the drug;
- patients with active forms of liver pathologies (including diseases of unknown origin), as well as conditions characterized by a persistent increase in the level of liver transaminases , and conditions in which any of the liver transaminases increases at least three times;
- kidney pathologies , in which creatinine does not exceed 60 ml/min;
- chronic progressive hereditary neuromuscular diseases , which are characterized by primary muscle damage ( myopathies );
- hypothyroidism;
- simultaneous use of the antidepressant Cyclosporine ;
- the patient is diagnosed with an increased risk of developing myotoxic complications (when the patient’s history contains a note of muscle toxicity, which was provoked by another hydroxymethylglutaryl-CoA reductase or a drug that is a derivative of fibric acid );
- alcohol addiction;
- severe forms of liver failure ;
- the patient belongs to the Mongoloid race;
- simultaneous use of fibrates ;
- lactose intolerance ;
- lactase deficiency;
- glucose-galactose malabsorption;
- pregnancy (the drug is also not prescribed to women of reproductive age if they do not use contraceptives);
- lactation;
- age under 18 and over 70 years.
Roxera®
Renal dysfunction
In patients receiving high doses of rosuvastatin (particularly 40 mg/day), tubular proteinuria was observed, which was detected using test strips and in most cases was intermittent or short-term. Such proteinuria does not indicate acute illness or progression of concomitant renal disease. The incidence of serious renal dysfunction observed in post-marketing studies of rosuvastatin is higher when taking a dose of 40 mg/day.
In patients taking Roxera® at a dose of 30 or 40 mg/day, it is recommended to monitor kidney function indicators during treatment (at least once every 3 months).
Effect on the musculoskeletal system
The following musculoskeletal effects have been reported with rosuvastatin at all doses, but particularly at doses greater than 20 mg/day: myalgia, myopathy, and in rare cases, rhabdomyolysis. Very rare cases of rhabdomyolysis have been reported with the simultaneous use of HMG-CoA reductase inhibitors and ezetimibe. This combination should be used with caution, as pharmacodynamic interactions cannot be excluded.
As with other HMG-CoA reductase inhibitors, the incidence of rhabdomyolysis with post-marketing use of rosuvastatin is higher when using a dose of 40 mg/day.
Determination of serum CPK activity
Serum CPK activity cannot be determined after intense physical exercise and in the presence of other possible reasons for an increase in its activity; this may lead to incorrect interpretation of the results obtained. If the initial serum CPK activity is significantly exceeded (5 times higher than the upper limit of normal), a repeat analysis should be performed after 5-7 days. Therapy should not be started if the results of a repeat analysis confirm the initial high serum CPK activity (more than 5 times the upper limit of normal).
Before starting therapy
Depending on the daily dose, Roxera® should be administered with caution to patients with existing risk factors for myopathy/rhabdomyolysis.
These factors include:
- renal dysfunction,
- hypothyroidism,
- history of muscle diseases (including family history),
- history of myotoxic effects when taking other HMG-CoA reductase inhibitors or fibrates,
- excessive alcohol consumption,
- age over 65 years,
- conditions in which the concentration of rosuvastatin in the blood plasma may increase,
- simultaneous use of fibrates.
In such patients, it is necessary to evaluate the risks and possible benefits of therapy. Clinical monitoring is also recommended. If the initial serum CPK activity is more than 5 times higher than the upper limit of normal, therapy with Roxera® cannot be started.
During drug therapy
The patient should be informed to immediately report to the doctor if muscle pain, muscle weakness or spasms occur unexpectedly, especially in combination with malaise and fever. In such patients, serum CPK activity should be determined. Therapy should be discontinued if serum CPK activity is significantly increased (more than 5 times the upper limit of normal), or if muscle symptoms are severe and cause daily discomfort (even if serum CPK activity is no more than 5 times the upper limit of normal). exceeds the upper limit of normal). If symptoms disappear and serum CPK activity returns to normal, consideration should be given to resuming the use of Roxera® or other HMG-CoA reductase inhibitors in lower doses with careful medical supervision. Monitoring serum CPK activity in the absence of symptoms is impractical.
Very rare cases of immune-mediated necrotizing myopathy have been reported with clinical manifestations in the form of persistent weakness of the proximal muscles and increased CPK activity in the blood serum during therapy or upon discontinuation of the use of HMG-CoA reductase inhibitors, including rosuvastatin. Additional studies of the muscular and nervous system, serological studies, and therapy with immunosuppressive drugs may be required.
There were no signs of increased effects on skeletal muscles when taking rosuvastatin and concomitant therapy. However, an increase in the number of cases of myositis and myopathy has been reported in patients taking other HMG-CoA reductase inhibitors in combination with fibric acid derivatives (for example, gemfibrozil), cyclosporine, nicotinic acid in lipid-lowering doses (more than 1 g / day), antifungals - azole derivatives, HIV protease inhibitors and macrolide antibiotics.
When used simultaneously with certain HMG-CoA reductase inhibitors, gemfibrozil increases the risk of developing myopathy. Thus, the simultaneous use of Roxera® and gemfibrozil is not recommended. The benefits of further changes in plasma lipid concentrations with the combined use of Roxera® with fibrates or nicotinic acid in lipid-lowering doses must be carefully weighed taking into account the possible risks. Roxera® at a dose of 30 mg/day is contraindicated for combination therapy with fibrates.
Roxera® should not be used simultaneously or within 7 days after stopping therapy with systemic fusidic acid preparations. In patients in whom the use of fusidic acid is considered necessary, statin therapy should be discontinued for the entire duration of fusidic acid therapy. There have been reports of rhabdomyolysis (including death in some cases) in patients receiving fusidic acid concomitantly with statins. The patient should seek immediate medical attention if any symptoms of muscle weakness, pain, or tenderness occur.
Therapy with Roxera® can be resumed 7 days after the last dose of fusidic acid.
In exceptional cases, when long-term use of systemic fusidic acid is required, for example, in the treatment of severe infections, the need for simultaneous use of Roxera® and fusidic acid should be considered individually and subject to careful medical supervision.
Due to the increased risk of rhabdomyolysis, Roxera® should not be used in patients with acute conditions that may lead to myopathy or conditions predisposing to the development of renal failure (for example, sepsis, arterial hypotension, major surgery, trauma, severe metabolic, endocrine or electrolyte disorders, uncontrollable seizures).
2-4 weeks after the start of treatment and/or when increasing the dose of Roxera®, monitoring of lipid metabolism parameters is necessary (dose adjustment is required if necessary).
Liver
Depending on the daily dose, Roxera® should be used with caution in patients with excessive alcohol consumption and/or in patients with a history of liver disease, or its use is contraindicated (see sections “Contraindications” and “With caution”).
It is recommended to determine liver function tests before the start of therapy and 3 months after its start. The use of Roxera® should be discontinued or the dose of the drug should be reduced if the activity of “liver” transaminases in the blood serum is 3 times higher than the upper limit of normal.
In patients with hypercholesterolemia due to hypothyroidism or nephrotic syndrome, treatment of underlying diseases should be carried out before starting treatment with Roxera®.
Ethnic characteristics
During pharmacokinetic studies, an increase in the plasma concentration of rosuvastatin was noted in representatives of the Mongoloid race compared to representatives of the Caucasian race.
Interstitial lung disease
Isolated cases of interstitial lung disease have been reported with the use of certain HMG-CoA reductase inhibitors, especially over long periods of time. Manifestations of the disease may include shortness of breath, non-productive cough and deterioration in general health (weakness, weight loss and fever).
If interstitial lung disease is suspected, therapy with HMG-CoA reductase inhibitors should be discontinued.
Diabetes mellitus type 2
In patients with glucose concentrations between 5.6 and 6.9 mmol/L, rosuvastatin therapy was associated with an increased risk of developing type 2 diabetes mellitus.
HIV protease inhibitors
Concomitant use of the drug with HIV protease inhibitors is not recommended (see section “Interaction with other drugs”).
Special information on excipients
Roxera® contains lactose and is therefore contraindicated in patients with lactose intolerance, lactase deficiency, and glucose-galactose malabsorption syndrome.
Side effects
During treatment with Roxera, the following side effects may occur:
- dysfunction of the immune system , including reactions caused by hypersensitivity to rosuvastatin or other ingredients of the drug, including the development of angioedema ;
- dysfunction of the digestive system , expressed in the form of frequent constipation, pain in the epigastric region, attacks of nausea; pancreatitis may develop ;
- disorders arising from the skin and subcutaneous tissues and expressed in the form of skin rashes, itching, urticaria ;
- dysfunction of skeletal muscles, which manifests itself as myalgia (often) and sometimes myopathy and rhabdomyolysis ;
- general disorders, the most common of which is asthenia ;
- dysfunction of the kidneys and urinary tract , which are most often accompanied by an increase in the concentration of protein in the urine.
Rocker may influence changes in laboratory parameters. Thus, after taking the drug, the activity of creatine kinase , the concentrations of glucose , bilirubin , the liver enzyme gamma-glutamyl transpeptidase , alkaline phosphatase , and the plasma concentrations of thyroid .
The frequency and severity of side effects are dose-dependent.
Indications for Roxera®
primary hypercholesterolemia according to Fredrickson (type IIa) or mixed dyslipidemia (type IIb) as an addition to diet when diet and other non-drug treatment methods are ineffective (for example, exercise, weight loss);
familial homozygous hypercholesterolemia as an addition to diet and other lipid-lowering therapy (eg LDL apheresis) or if such therapy is ineffective;
hypertriglyceridemia (Fredrickson type IV) as an addition to the diet;
to slow the progression of atherosclerosis as an addition to diet in patients who are indicated for therapy to reduce plasma concentrations of cholesterol and LDL-C;
primary prevention of major cardiovascular complications (stroke, myocardial infarction, arterial revascularization) in adult patients without clinical signs of coronary heart disease (CHD), but with an increased risk of its development (age over 50 years for men and over 60 years for women, increased plasma concentration of C-reactive protein (≥2 g/l) in the presence of at least one of the additional risk factors, such as: arterial hypertension, low plasma concentration of HDL-C, smoking, early onset of coronary artery disease in the family history).
Roxer tablets: instructions for use, method of administration and dosage regimen
Before prescribing the drug, the patient is recommended to switch to a standard diet, the purpose of which is to reduce cholesterol . It is necessary to adhere to this diet throughout the entire course of treatment.
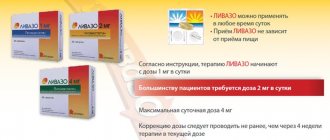
The dose is selected individually by the attending physician depending on the purpose of therapy and its effectiveness. The drug can be taken at any time of the day, without being tied to meal times.
The tablet is swallowed whole, without crushing or chewing, and with a sufficient amount of water.
Patients with hypercholesterolemia should start taking the drug with doses equal to 5 or 10 mg of rosuvastatin . The tablets are taken orally, one per day. Moreover, this condition persists both for patients who have not been treated with statins , and for patients who have already undergone treatment with drugs that suppress the activity of hydroxymethylglutaryl-CoA reductase .
cholesterol concentrations , and also assesses the risks of developing cardiovascular complications and side effects.
In cases where this is necessary, the dose may be adjusted to the next level, however, such an adjustment should be made no earlier than 4 weeks after the first prescription.
Considering that adverse reactions are dose-dependent and occur more often when taking 40 mg of rosuvastatin than when taking it in smaller quantities, increasing the daily dose to 30 or 40 mg should be carried out with particular care for:
- patients with severe forms of hypercholesterolemia ;
- patients who are at high risk of developing complications in the function of the heart and vascular system (in particular, if the patient is diagnosed with familial hypercholesterolemia ).
If taking smaller doses of rosuvastatin in these categories of patients did not give the expected result, after prescribing Roxera at a dosage of 30 or 40 mg per day, patients must be constantly monitored by their doctor.
Also, regular monitoring by a doctor is indicated in cases where treatment is started immediately with a dose of 30 or 40 mg.
In accordance with the instructions for use, Roxera 20 mg is indicated as an initial dose for the prevention of heart and vascular diseases in patients who have an increased risk of developing such pathologies.
renal dysfunction do not need to adjust the dose; however, the drug is prescribed to this group of patients with caution.
For renal , when creatinine is within 60 ml/min, treatment begins with a dose of 5 mg. High doses of the drug (30 and 40 mg) are contraindicated.
renal dysfunction are prohibited from prescribing the drug in any dosage.
When Roxera is prescribed to patients with liver pathologies whose Child-Pugh do not exceed 7, there is no increase in systemic exposure to rosuvastatin .
liver dysfunction scores are 8 or 9 on the Child-Pugh scale , systemic exposure is increased. Therefore, before prescribing the drug to such patients, additional testing of renal function is required.
experience in treating patients whose scores exceed 9 points on the Child-Pugh scale .
Roxera, 30 pcs., 20 mg, film-coated tablets
Renal dysfunction
In patients receiving high doses of rosuvastatin (particularly 40 mg/day), tubular proteinuria was observed, which was detected using test strips and in most cases was intermittent or short-term. Such proteinuria does not indicate acute illness or progression of concomitant renal disease. The incidence of serious renal dysfunction observed in post-marketing studies of rosuvastatin is higher when taking a dose of 40 mg/day.
In patients taking Roxera® at a dose of 30 or 40 mg/day, it is recommended to monitor kidney function indicators during treatment (at least once every 3 months).
Effect on the musculoskeletal system
The following musculoskeletal effects have been reported with rosuvastatin at all doses, but particularly at doses greater than 20 mg/day: myalgia, myopathy, and in rare cases, rhabdomyolysis. Very rare cases of rhabdomyolysis have been reported with the simultaneous use of HMG-CoA reductase inhibitors and ezetimibe. This combination should be used with caution, as pharmacodynamic interactions cannot be excluded.
As with other HMG-CoA reductase inhibitors, the incidence of rhabdomyolysis with post-marketing use of rosuvastatin is higher when using a dose of 40 mg/day.
Determination of serum CPK activity
Serum CPK activity cannot be determined after intense physical exercise and in the presence of other possible reasons for an increase in its activity; this may lead to incorrect interpretation of the results obtained. If the initial serum CPK activity is significantly exceeded (5 times higher than the upper limit of normal), a repeat analysis should be performed after 5-7 days. Therapy should not be started if the results of a repeat analysis confirm the initial high serum CPK activity (more than 5 times the upper limit of normal).
Before starting therapy
Depending on the daily dose, Roxera® should be administered with caution to patients with existing risk factors for myopathy/rhabdomyolysis.
These factors include:
- renal dysfunction,
- hypothyroidism,
- history of muscle diseases (including family history),
- history of myotoxic effects when taking other HMG-CoA reductase inhibitors or fibrates,
- excessive alcohol consumption,
- age over 65 years,
- conditions in which the concentration of rosuvastatin in the blood plasma may increase,
- simultaneous use of fibrates.
In such patients, it is necessary to evaluate the risks and possible benefits of therapy. Clinical monitoring is also recommended. If the initial serum CPK activity is more than 5 times higher than the upper limit of normal, therapy with Roxera® cannot be started.
During drug therapy
The patient should be informed to immediately report to the doctor if muscle pain, muscle weakness or spasms occur unexpectedly, especially in combination with malaise and fever. In such patients, serum CPK activity should be determined. Therapy should be discontinued if serum CPK activity is significantly increased (more than 5 times the upper limit of normal), or if muscle symptoms are severe and cause daily discomfort (even if serum CPK activity is no more than 5 times the upper limit of normal). exceeds the upper limit of normal). If symptoms disappear and serum CPK activity returns to normal, consideration should be given to resuming the use of Roxera® or other HMG-CoA reductase inhibitors in lower doses with careful medical supervision. Monitoring serum CPK activity in the absence of symptoms is impractical.
Very rare cases of immune-mediated necrotizing myopathy have been reported with clinical manifestations in the form of persistent weakness of the proximal muscles and increased CPK activity in the blood serum during therapy or upon discontinuation of the use of HMG-CoA reductase inhibitors, including rosuvastatin. Additional studies of the muscular and nervous system, serological studies, and therapy with immunosuppressive drugs may be required.
There were no signs of increased effects on skeletal muscles when taking rosuvastatin and concomitant therapy. However, an increase in the number of cases of myositis and myopathy has been reported in patients taking other HMG-CoA reductase inhibitors in combination with fibric acid derivatives (for example, gemfibrozil), cyclosporine, nicotinic acid in lipid-lowering doses (more than 1 g / day), antifungals - azole derivatives, HIV protease inhibitors and macrolide antibiotics.
When used simultaneously with certain HMG-CoA reductase inhibitors, gemfibrozil increases the risk of developing myopathy. Thus, the simultaneous use of Roxera® and gemfibrozil is not recommended. The benefits of further changes in plasma lipid concentrations with the combined use of Roxera® with fibrates or nicotinic acid in lipid-lowering doses must be carefully weighed taking into account the possible risks. Roxera® at a dose of 30 mg/day is contraindicated for combination therapy with fibrates.
Roxera® should not be used simultaneously or within 7 days after stopping therapy with systemic fusidic acid preparations. In patients in whom the use of fusidic acid is considered necessary, statin therapy should be discontinued for the entire duration of fusidic acid therapy. There have been reports of rhabdomyolysis (including death in some cases) in patients receiving fusidic acid concomitantly with statins. The patient should seek immediate medical attention if any symptoms of muscle weakness, pain, or tenderness occur.
Therapy with Roxera® can be resumed 7 days after the last dose of fusidic acid.
In exceptional cases, when long-term use of systemic fusidic acid is required, for example, in the treatment of severe infections, the need for simultaneous use of Roxera® and fusidic acid should be considered individually and subject to careful medical supervision.
Due to the increased risk of rhabdomyolysis, Roxera® should not be used in patients with acute conditions that may lead to myopathy or conditions predisposing to the development of renal failure (for example, sepsis, arterial hypotension, major surgery, trauma, severe metabolic, endocrine or electrolyte disorders, uncontrollable seizures).
2-4 weeks after the start of treatment and/or when increasing the dose of Roxera®, monitoring of lipid metabolism parameters is necessary (dose adjustment is required if necessary).
Liver
Depending on the daily dose, Roxera® should be used with caution in patients with excessive alcohol consumption and/or in patients with a history of liver disease, or its use is contraindicated (see sections “Contraindications” and “With caution”).
It is recommended to determine liver function tests before the start of therapy and 3 months after its start. The use of Roxera® should be discontinued or the dose of the drug should be reduced if the activity of “liver” transaminases in the blood serum is 3 times higher than the upper limit of normal.
In patients with hypercholesterolemia due to hypothyroidism or nephrotic syndrome, treatment of underlying diseases should be carried out before starting treatment with Roxera®.
Ethnic characteristics
During pharmacokinetic studies, an increase in the plasma concentration of rosuvastatin was noted in representatives of the Mongoloid race compared to representatives of the Caucasian race.
Interstitial lung disease
Isolated cases of interstitial lung disease have been reported with the use of certain HMG-CoA reductase inhibitors, especially over long periods of time. Manifestations of the disease may include shortness of breath, non-productive cough and deterioration in general health (weakness, weight loss and fever).
If interstitial lung disease is suspected, therapy with HMG-CoA reductase inhibitors should be discontinued.
Diabetes mellitus type 2
In patients with glucose concentrations between 5.6 and 6.9 mmol/L, rosuvastatin therapy was associated with an increased risk of developing type 2 diabetes mellitus.
HIV protease inhibitors
Concomitant use of the drug with HIV protease inhibitors is not recommended (see section “Interaction with other drugs”).
Special information on excipients
Roxera® contains lactose and is therefore contraindicated in patients with lactose intolerance, lactase deficiency, and glucose-galactose malabsorption syndrome.
Overdose
Clinical manifestations that may occur when the recommended dose of the drug is exceeded are not described. After a single dose of Roxera at a dose several times greater than the established daily dose, no clinically significant changes in the pharmacokinetics of rosuvastatin were observed.
In case of overdose and the appearance of symptoms of intoxication of the body, symptomatic treatment and, if necessary, a set of supportive measures are prescribed.
It is also recommended to monitor the level of creatine kinase and perform a test to assess liver .
The feasibility of prescribing hemodialysis is considered unlikely.
Directions for use and doses
Inside, do not chew or crush the tablet, swallow it whole with water, can be taken at any time of the day, regardless of meals.
Before starting therapy with Roxera®, the patient should begin to follow a standard cholesterol-lowering diet and continue to follow it during treatment. The dose of the drug should be selected individually, depending on the goals of therapy and the therapeutic response to treatment, taking into account recommendations for target plasma lipid concentrations.
The recommended initial dose for patients starting to take the drug, or for patients transferred from taking other HMG-CoA reductase inhibitors, should be 5 or 10 mg of Roxera® 1 time per day.
When using the drug simultaneously with gemfibrozil, fibrates, nicotinic acid at a dose of more than 1 g/day, an initial dose of 5 mg is recommended for patients. When choosing the initial dose, you should be guided by the individual concentration of cholesterol in the blood plasma and take into account the possible risk of developing cardiovascular complications; the potential risk of side effects must also be taken into account. If necessary, the dose can be increased after 4 weeks.
Due to the possible development of side effects when using a dose of 40 mg / day, compared with lower doses of the drug, increasing the dose to 40 mg / day after additional use of a dose higher than the recommended initial dose for 4 weeks of therapy can only be carried out in patients with severe degree of hypercholesterolemia and a high risk of developing cardiovascular complications (especially in patients with familial hypercholesterolemia) who have not achieved the desired result of therapy when using a dose of 20 mg/day and who will be under medical supervision. Particularly careful monitoring of patients receiving the drug at a dose of 40 mg/day is recommended.
It is not recommended to use a dose of 40 mg/day in patients who have not previously consulted a doctor. After 2–4 weeks of therapy and/or when increasing the dose of Roxera®, monitoring of lipid metabolism parameters is necessary (dose adjustment is required if necessary).
Patients with renal failure. No dosage adjustment is required in patients with mild or moderate renal impairment. In patients with severe renal failure (creatinine clearance less than 30 ml/min), the use of Roxera® is contraindicated. The use of the drug in a dose of more than 30 mg/day in patients with moderate to severe renal failure (creatinine clearance less than 60 ml/min) is contraindicated. For patients with moderate renal failure, the recommended initial dose of the drug is 5 mg/day.
Patients with liver failure. Roxera® is contraindicated in patients with active liver disease. There is no experience with the use of the drug in patients with liver failure above 9 points (class C) on the Child-Pugh scale.
Use in elderly patients. Patients over the age of 65 years are recommended to start using the drug with a dose of 5 mg/day.
Ethnic groups. When studying the pharmacokinetic parameters of rosuvastatin in patients belonging to different ethnic groups, an increase in the systemic concentration of rosuvastatin was noted among the Japanese and Chinese. This fact should be taken into account when using the drug Roxera® in these groups of patients. When using doses of 10 and 20 mg/day, the recommended initial dose for patients of the Mongoloid race is 5 mg/day. For patients of the Mongoloid race, the use of Roxera® at a dose of 40 mg is contraindicated.
Genetic polymorphism. Carriers of the SLCO1B1 (OATP1B1) c.521CC and ABCG2 (BCRP) c.421AA genotypes had an increase in rosuvastatin exposure (AUC) compared to carriers of the SLCO1B1 c.521TT and ABCG2 c.421CC genotypes. For patients carrying genotypes c.521CC or c.421AA, the recommended maximum dose of Roxera® is 20 mg once a day.
Patients predisposed to myotoxic complications. The use of Roxera® in a dose of 40 mg is contraindicated in patients predisposed to the development of myotoxic complications. If it is necessary to use doses of 10 and 20 mg/day, the recommended initial dose for this group of patients is 5 mg.
Concomitant therapy. Rosuvastatin binds to various transport proteins (in particular OATP1B1 and BCRP). When using Roxera® with drugs (such as cyclosporine, some human immunodeficiency virus (HIV) protease inhibitors, including a combination of ritonavir with atazanavir, lopinavir and/or tipranavir) that increase the concentration of rosuvastatin in the blood plasma due to interaction with transport proteins, the risk of developing myopathy (including rhabdomyolysis) may increase. In such cases, the possibility of using alternative therapy or temporarily stopping taking Roxera® should be assessed. If it is necessary to use the above drugs, the benefit-risk ratio of concomitant therapy with Roxera® should be assessed and the possibility of reducing its dose should be considered.
Interaction
When Roxera is prescribed in combination with Cyclosporine of rosuvastatin increases significantly (approximately seven times), while the plasma concentration of cyclosporine remains unchanged.
When co-administered with drugs that are vitamin K or drugs that suppress the activity of hydroxymethylglutaryl-CoA reductase , at the beginning of the course of treatment, as well as when increasing the daily dose by titrating it, an increase in INR (international normalized ratio) may be observed.
As a rule, when the dose is reduced by titration or complete withdrawal of the drug, this indicator decreases.
Concomitant use with the lipid-lowering drug Ezetimibe does not provoke changes in the AUC and maximum plasma concentrations of both drugs, however, the possibility of pharmacodynamic interaction cannot be excluded.
In combination with Gemfibrozil and other drugs that help lower lipid , it provokes a twofold increase in AUC and maximum plasma concentrations of rosuvastatin .
Data from special studies have shown that administration with Fenofibrate potentially does not lead to changes in pharmacokinetic parameters, however, the possibility of pharmacodynamic drug interactions cannot be excluded.
Drugs such as Gemfibrozil and Fenofibrate , as well as nicotinic acid , when prescribed simultaneously with hydroxymethylglutaryl-CoA reductase increase the likelihood of developing myopathy (which is most likely due to their ability to provoke a similar effect when prescribed as a monotherapeutic agent).
When Roxera is used simultaneously with fibrates , rosuvastatin in doses of 30 and 40 mg is not prescribed. The initial daily dose of rosuvastatin for patients taking fibrates is 5 mg.
Concomitant use of the drug with serine protease provokes a change in the exposure of rosuvastatin . For this reason, Roxer is not prescribed HIV -infected patients who are undergoing treatment with serine protease .
When taken simultaneously with antacid drugs, the plasma concentration of rosuvastatin is reduced by approximately half. To reduce the severity of this effect , it is recommended to take antacids two hours after taking the Roxera tablet.
During the simultaneous administration of rosuvastatin with Erythromycin , the AUC of rosuvastatin is reduced by 20%, and its plasma concentration by about a third. This may be due to increased mobility of the intestinal tract , which is provoked by taking Erythromycin .
When Roxera is prescribed in combination with hormonal contraceptives for oral administration, the AUC of ethinyl estradiol increases by 26%, and the same indicator for norgestrel by 34%.
This increase in AUC levels must be taken into account when selecting the optimal dose of oral contraceptive
There are no pharmacokinetic data regarding simultaneous use with drugs for hormone replacement therapy, but the possibility of interaction and an increase in AUC cannot be excluded.
Studies of the combination of rosuvastatin with the pacemaker Digoxin showed no clinically significant interaction.
Rosuvastatin has neither a suppressive nor a stimulating effect on isoenzymes the cytochrome P450 system . In addition, the metabolization of rosuvastatin under their influence is minimal and is not clinically significant.
No significant interaction was observed rosuvastatin and the antifungal agents Fluconazole and Ketoconazole
The combination with the antifungal drug Intraconazole, which inhibits the activity isoenzyme , provokes an increase in the AUC of rosuvastatin by 28%. However, this increase is not considered clinically important.
Rocker
special instructions
Impaired renal function
In patients receiving high doses of rosuvastatin (in particular 40 mg / day), tubular proteinuria was observed, which was detected using test strips and in most cases was intermittent or short-term. Such proteinuria does not indicate acute or progression of concomitant renal disease. The incidence of serious renal dysfunction observed in post-marketing studies of rosuvastatin is higher when taking a dose of 40 mg/day. In patients taking Roxera® at a dose of 30 or 40 mg/day, it is recommended to monitor kidney function indicators during treatment (at least once every 3 months).
Effect on the musculoskeletal system
The following musculoskeletal effects have been reported with rosuvastatin at all doses, but particularly at doses greater than 20 mg/day: myalgia, myopathy, and in rare cases, rhabdomyolysis. Very rare cases of rhabdomyolysis have been reported with the simultaneous use of HMG-CoA reductase inhibitors and ezetimibe. This combination should be used with caution, as pharmacodynamic interactions cannot be excluded. As with other HMG-CoA reductase inhibitors, the incidence of rhabdomyolysis during post-marketing use of Roxera® is higher when using a dose of 40 mg/day.
Determination of CPK activity
CPK activity cannot be determined after intense physical activity and in the presence of other possible reasons for the increase in its activity; this may lead to incorrect interpretation of the results obtained. If the initial CPK activity is significantly exceeded (5 times higher than the upper limit of normal), a repeat analysis should be performed after 5-7 days. Therapy cannot be started if the results of a re-analysis confirm the initial high activity of CPK (more than 5 times the upper limit of normal).
Before starting therapy
Depending on the daily dose, Roxera® should be administered with caution to patients with existing risk factors for myopathy/rhabdomyolysis, or the use of the drug is contraindicated (see sections “Contraindications” and “With caution”).
These factors include:
- renal dysfunction;
- hypothyroidism;
- history of muscle diseases (including family history);
- history of myotoxic effects when taking other HMG-CoA reductase inhibitors or fibrates;
- excessive alcohol consumption;
— age over 65 years;
- conditions in which the concentration of rosuvastatin in the blood plasma may increase;
- simultaneous use of fibrates.
In such patients, it is necessary to evaluate the risks and possible benefits of therapy. Clinical monitoring is also recommended. If the initial CPK activity is more than 5 times higher than the upper limit of normal, therapy with Roxera® cannot be started.
During drug therapy
The patient should be informed to immediately report to the doctor if muscle pain, muscle weakness or spasms occur unexpectedly, especially in combination with malaise and fever. In such patients, CPK activity should be determined. Therapy should be discontinued if CK activity is significantly increased (more than 5 times the upper limit of normal) or if muscle symptoms are severe and cause daily discomfort (even if CPK activity is no more than 5 times the upper limit norms). If symptoms disappear and CPK activity returns to normal, consideration should be given to resuming the use of Roxera® or other HMG-CoA reductase inhibitors in lower doses with careful medical supervision. Monitoring CPK activity in the absence of symptoms is impractical. Very rare cases of immune-mediated necrotizing myopathy have been reported with clinical manifestations in the form of persistent weakness of the proximal muscles and increased CPK activity in the blood serum during therapy or upon discontinuation of the use of HMG-CoA reductase inhibitors, including rosuvastatin. Additional studies of the muscular and nervous system, serological studies, and therapy with immunosuppressive drugs may be required.
There were no signs of increased effects on skeletal muscles when taking rosuvastatin and concomitant therapy. However, an increase in the number of cases of myositis and myopathy has been reported in patients taking other HMG-CoA reductase inhibitors in combination with fibric acid derivatives (for example, gemfibrozil), cyclosporine, nicotinic acid in lipid-lowering doses (more than 1 g / day), antifungal agents derivatives azole, HIV protease inhibitors and macrolide antibiotics.
When used simultaneously with certain HMG-CoA reductase inhibitors, gemfibrozil increases the risk of developing myopathy. Thus, the simultaneous use of Roxera® and gemfibrozil is not recommended. The benefits of further changes in plasma lipid concentrations with the combined use of Roxera® with fibrates or nicotinic acid in lipid-lowering doses must be carefully weighed taking into account the possible risks. Roxera® at a dose of 30 mg/day is contraindicated for combination therapy with fibrates. Due to the increased risk of rhabdomyolysis, Roxera® should not be used in patients with acute conditions that may lead to myopathy or conditions predisposing to the development of renal failure (for example, sepsis, arterial hypotension, major surgery, trauma, severe metabolic, endocrine and electrolyte disturbances or uncontrolled seizures).
Liver
Depending on the daily dose, Roxera® should be used with caution in patients with excessive alcohol consumption and/or a history of liver disease, or its use is contraindicated (see sections “Contraindications” and “With caution”).
It is recommended to determine liver function tests before the start of therapy and 3 months after its start. The use of Roxera® should be discontinued or the dose of the drug should be reduced if the activity of “liver” transaminases in the blood serum is 3 times higher than the upper limit of normal.
In patients with hypercholesterolemia due to hypothyroidism or nephrotic syndrome, treatment of underlying diseases should be carried out before starting treatment with Roxera®.
Ethnic characteristics
During pharmacokinetic studies, an increase in the plasma concentration of rosuvastatin was noted in representatives of the Mongoloid race compared to representatives of the Caucasian race.
The drug Roxera® contains lactose, and therefore it should not be used in patients with lactose intolerance, lactase deficiency, or glucose-galactose malabsorption syndrome.
Interstitial lung disease
Isolated cases of interstitial lung disease have been reported with the use of certain HMG-CoA reductase inhibitors, especially over long periods of time. Manifestations
diseases may include shortness of breath, non-productive cough and deterioration in general health (weakness, weight loss and fever). If interstitial lung disease is suspected, therapy with HMG-CoA reductase inhibitors should be discontinued.
Diabetes mellitus type 2
In patients with glucose concentrations between 5.6 and 6.9 mmol/L, rosuvastatin therapy was associated with an increased risk of developing type 2 diabetes mellitus.
Analogues of Roxers
Level 4 ATX code matches:
Akorta
Atomax
Lipitor
Pravastatin
Simvastol
Owencore
Simgal
Tulip
Lovastatin
Liptonorm
Rozulip
Zokor
Rosart
Tevastor
Atorvastatin
Liprimar
Simvastatin
Atoris
Basilip
Rosecard
Analogs of the drug that have the same ATC code, active substance and release form as Roxera are:
- Klyvas 10;
- Klyvas 20;
- Crestor;
- Mertenil;
- Rovics;
- Rosart;
- Rozvator;
- Rosuvastatin Sandoz;
- Rosecard;
- Rozulip;
- Romazik;
- Fastong.
The price of Roxera analogues in Ukraine varies from 65 to 595 hryvnia, on the Russian pharmaceutical market - from 220 to 2100 rubles.
Reviews about Roxer
Roxer tablets - reviews left on forums by patients taking the drug confirm this fact - are an effective means for lowering cholesterol .
The main advantages of the drug, many of them include a pronounced result, which is observed in a shorter time than when taking drugs similar to Roxera in their pharmacological action.
At the same time, an improvement in the clinical picture often occurs against the background of prescribing an order of magnitude lower dose compared to analogues (for example, Sigmal ).
Rocker price
The price of Roxera depends on the dose of the active substance contained in it and the number of tablets in the package.
So, for example, tablets containing rosuvastatin 5 mg can be purchased on average for 295-450 Russian rubles per pack of 30 pieces. A package containing 90 Roxer 5 mg tablets will cost an average of 850-1100 Russian rubles.
The price of Roxera 10 mg is:
- 395-590 Russian rubles for a pack of 30 pieces;
- 1026-1500 Russian rubles per pack of 90 pieces.
The price of Roxera 20 mg is:
- 585-980 Russian rubles for a pack of 30 pieces;
- 1500-2175 Russian rubles per pack of 90 pieces.
- Online pharmacies in RussiaRussia
- Online pharmacies in UkraineUkraine
- Online pharmacies in KazakhstanKazakhstan
ZdravCity
- Roxera tab.
p/o captivity. 5mg No. 30 Krka-Rus LLC 470 rub. order - Roxera tab. p/o captivity. 10mg No. 30Krka-Rus LLC
RUR 569 order
- Roxera tab. p/o captivity. 5mg No. 90 Krka-Rus LLC
RUB 1,017 order
- Roxera tab. p/o captivity. 10 mg No. 90 Krka-Rus LLC
RUB 1,307 order
- Roxera tablets p.p.o 15 mg 90 pcs. Krka-Rus LLC
RUB 1,514 order
Pharmacy Dialogue
- Roxera tablets 10 mg No. 90KPKA
RUB 1,334 order
- Roxera tablets 20 mg No. 30KPKA
RUB 1,909 order
- Roxera tablets 15 mg No. 30KPKA
676 RUR order
- Roxera tablets 5 mg No. 30KPKA
RUR 439 order
- Roxera tablets 15 mg No. 90KPKA
RUB 1,457 order
show more
Pharmacy24
- Roxera 40 mg No. 30 tablets KPKA, d.d., Novo mesto, Slovenia
250 UAH. order - Roxera 30 mg No. 90 tablets KPKA, d.d., Novo Mesto, Slovenia
370 UAH. order
- Roxera 10 mg N90 tablets KPKA, d.d., Novo Mesto, Slovenia
298 UAH order
- Roxera 20 mg No. 30 tablets KPKA, d.d., Novo Mesto, Slovenia
166 UAH order
- Roxera 15 mg N30 tablets KRKA, Slovenia
98 UAH order
PaniPharmacy
- Roxera tablets Roxera tablets 10 mg No. 30 Slovenia, KRKA dd Novo Mesto
134 UAH order
- Roxer table 5mg No.90
219 UAH. order
- Roxera tablets Roxera tablets. 30 mg No. 90 Slovenia, KRKA dd Novo Mesto
396 UAH. order
- Roxera tablets Roxera tablets 15 mg No. 30 Slovenia, KRKA dd Novo Mesto
112 UAH order
- Roxera tablets Roxera tablets 20 mg No. 30 Slovenia, KRKA dd Novo Mesto
194 UAH order
show more