1.What is arachnoiditis and its causes?
Arachnoiditis
is a pain syndrome caused by inflammation of the arachnoid membrane of one of the membranes surrounding and protecting the nerves of the spinal cord. The main signs of arachnoiditis are severe stinging and burning pain, neurological problems.
Causes of arachnoiditis.
Inflammation of the arachnoid membrane - arachnoiditis - can lead to the formation of scar tissue and failure of the spinal nerves. Arachnoiditis can develop for one of the following reasons:
- Direct damage to the spine.
- Chemical exposure. It is believed that certain chemicals that were previously used for myelograms and injected into the area adjacent to the spinal cord and nerves could cause arachnoiditis. A similar effect is attributed to the substances included in the epidural injection.
- Bacterial or viral infection. Some infections such as viral and fungal meningitis and tuberculosis can affect the spine.
- Chronic compression of the spinal nerves. The cause of such compression may be osteochondrosis or extended spinal stenosis (narrowing of the spinal column).
- Complication after spinal surgery or other invasive procedures in the back area.
A must read! Help with treatment and hospitalization!
Arachnoiditis
It is necessary to eliminate the source of infection (otitis media, sinusitis, etc.). Antibiotics are prescribed in therapeutic doses. Desensitizing and antihistamine drugs are indicated (diphenhydramine, diazolin, suprastin, tavegil, pipolfen, calcium chloride, histaglobulin). Pathogenetic therapy is designed for long-term course treatment with absorbable agents, normalization of intracranial pressure, improvement of cerebral circulation and metabolism. Biogenic stimulants (aloe, vitreous, FiBS) and iodide preparations (bioquinol, potassium iodide) are used. Lidase is also used in the form of subcutaneous injections of 0.1 g of dry matter, dissolved in 1 ml of 0.5% novocaine solution every other day, for a course of 15 injections. The courses are repeated after 4–5 months. Pyrogenal has a resolving effect. The first intramuscular injections of pyrogenal begin with a dose of 25 MTD, in subsequent days the dose is increased daily by 50 MTD and brought to 1000 MTD; for a course of treatment up to 30 injections. When intracranial pressure increases, decongestants and diuretics are used (mannitol, furosemide, diacarb, glycerin, etc.). For convulsive syndromes, antiepileptic drugs are used. Metabolic therapy is carried out (glutamic acid, piracetam, aminalon, cerebrolysin). Symptomatic agents are used according to indications. Lack of improvement after treatment, increase in intracranial pressure and focal symptoms, opticochiasmatic arachnoiditis with a steady decrease in vision are indications for surgical intervention.
Forecast. In relation to life, usually favorable. Arachnoiditis of the posterior cranial fossa with occlusive hydrocephalus may pose a danger. The labor prognosis worsens with frequent relapses or a progressive course with frequent hypertensive crises, epileptic seizures, and the optico-chiasmatic form.
Work ability. Patients are recognized as group III disabled if employment or transfer to light work leads to a decrease in the volume of production activity. Group II disability is established in the presence of frequent epileptic seizures, a significant decrease in visual acuity in both eyes (from 0.04 to 0.08 with correction). Group I disabilities are patients with optico-chiasmatic arachnoiditis, accompanied by blindness. Patients with liquorodynamic disorders, epileptic seizures and vestibular crises are contraindicated from working at heights, near fire, near moving machinery, or in transport. Work in unfavorable meteorological conditions, in noisy rooms, in contact with toxic substances and in conditions of altered atmospheric pressure, as well as work associated with constant vibration and changes in head position are contraindicated.
2. Symptoms of the disease
Symptoms of arachnoiditis can manifest in different ways. But often this disease affects the nerves leading to the lower back and legs. The most common symptom of arachnoiditis
is pain, but possible signs of inflammation of the arachnoid membrane may be:
- Tingling, numbness and weakness in the legs;
- Sensation as if insects were crawling on the skin or water running down the legs;
- Severe shooting pain in the legs that feels like an electric shock;
- Muscle cramps, spasms, and uncontrollable leg jerking;
- Bladder, bowel or sexual problems.
As arachnoiditis progresses, symptoms may become more severe or even permanent. Many people with arachnoiditis are unable to work and become disabled because they experience constant pain.
Visit our Neurology page
Arachnoiditis of the brain: diagnosis
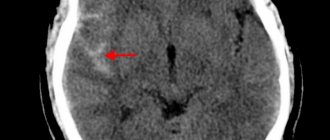
To diagnose this disease, a comprehensive examination of the patient and comparison of all identified data is required. Diagnosis of arachnoiditis begins with anamnesis (questioning of the patient). Close attention should be paid to past infectious diseases and traumatic brain injuries, mnestic and psycho-emotional disorders. Using skull radiography, the presence of hypertension is detected, according to Echo-EG data, the presence of hydrocephalus is judged, EEG reveals focal irritation and epileptic activity. If arachnoiditis is suspected, the patient must be examined by an ophthalmologist. The presence of congestion in the area of the optic nerve head only confirms the diagnosis. The otolaryngologist should also examine the patient for tinnitus and hearing impairment - all of this is diagnosed using threshold audiometry. In addition, it is recommended to conduct electrocochleography to determine the level of damage to the hearing aid. Computed tomography and magnetic resonance imaging of the brain are used to identify morphological changes that are a consequence of arachnoiditis (the process of formation of adhesions, atrophic changes, the presence of cysts), and to exclude various volumetric processes: abscess, hematoma, tumor. Using CT cisternography, changes in the shape of the subarachnoid spaces are determined. To differentiate arachnoiditis from other cerebral diseases, cerebrospinal fluid studies are performed, revealing an increase in protein up to 0.6 g/l and an increased concentration of neurotransmitters.
4. Treatment of the disease
There is no cure as such for arachnoiditis. Treatment may be the same as for other chronic pain, where the goal is to relieve pain and other symptoms that directly affect quality of life
. Doctors often recommend a pain treatment program in combination with physiotherapy, exercise therapy and psychotherapeutic sessions. Surgical treatment for arachnoiditis is a controversial option because the results of surgery may not be as expected and will provide only short-term relief. Some patients benefit from steroid injections and electrical stimulation.
Arachnoiditis: treatment
Treatment of this disease is usually carried out in a hospital, and the choice of treatment method depends on the intensity of arachnoiditis and the causes of its occurrence. There are two treatment methods: medication and surgery. The medicinal method, as a rule, includes: - anti-inflammatory drugs (glucocorticosteroids: prednisolone, methylprednisolone...); — absorbable drugs (pyrogenal, rumanol, lidase...); — digration agents (furosemide, mannitol...); - antiepileptic drugs (keppra, finlepsin...); - metabolites and neuroprotectors (nootropil, ginkgo biloba, mildronate...); - antiallergens; - psychotropics. If there is a source of infection, its sanitation is mandatory. Attention! Remember that all of the above-mentioned medications have contraindications and cause quite serious side effects. That is why they must be taken only with the permission of the appropriate doctor. In severe forms of arachnoiditis, surgical intervention is resorted to, which consists of restoring the patency of the cerebrospinal fluid tract, removing cysts, “separation” of the corresponding areas of the brain, and creating alternative pathways for the outflow of cerebrospinal fluid. Transfer factor is required as a complex therapy. This immune drug is a component of our immune system; it is an “extract” from cow colostrum and chicken egg yolks of transfer factors - immune molecules that are carriers of immune “memory”. Once in the body, these particles perform the following functions: - Restore the normal functioning of the human immune system and metabolic processes; — Synergistically enhances the therapeutic effect of medications taken, while neutralizing their side effects on the body (which is very important); — Transfer factors “record” all cases of invasion of foreign bodies into the body, information about these agents and methods for neutralizing them. When these foreign agents invade again, transfer factors “extract” information about them and the immune system, using this information, destroys them. Such a unique algorithm of action is available only for this immunomodulator, which, today, has no analogues in the world, either in terms of effectiveness or safety for humans. Our immune system is closely intertwined with the nervous system, and they are interdependent, so eliminating any failures of the immune system often eliminates pathologies of the nervous system, and therefore Transfer Factor is the best preventive remedy for arachnoiditis, as well as for recovery in the postoperative period.
Symptomatic picture
The disease has an acute onset. Patients experience severe headaches and bilateral vision impairment. Analgesics do not relieve cephalalgia. With visual stress (watching TV shows, reading, working at the computer), increased fatigue appears. As the pathology develops, it leads to severe pain in the periorbital region. Pain sensations radiate to the bridge of the nose, forehead, temples and superciliary areas. May be localized in the orbit of the eye. In complex cases, dysfunction reaches its greatest strength after several hours. With a milder course, the process takes 2-3 days. Individual areas begin to disappear from the visual field. Color vision, especially the sense of red and green, may be affected. Often the patient's pupils become different sizes. This period is accompanied by dyspeptic disorders: nausea, vomiting. The acute phase can turn into chronic. In addition, the cranial nerves responsible for the sense of smell may be affected. Patients experience literal drooping of the mouth or eye due to impaired innervation of the facial nerve.
If the lesion extends to the hypothalamic region, patients experience:
- Vegetative-vascular crises;
- Convulsive muscle contractions;
- Violation of thermoregulation;
- Thirst;
- Increased sweating;
- Low-grade fever;
- Sleep disorders.
In the chronic form, clinical signs develop gradually. After diagnostic cisternography, vision in a number of patients is restored for a short period of time.
Possible risks
The most common complication is optic nerve atrophy. Dislocation of brain structures is possible. When cystic tissue grows, focal symptoms and tissue compression appear. If the process spreads to other membranes of the brain, meningitis and meningoencephalitis are noted. The course may be complicated by intracranial abscesses. If secondary damage to the ventricles occurs, ventriculitis appears. Such patients are at risk of acute cerebrovascular accident.
Treatment of post-traumatic arachnoiditis in Saratov, Russia
Sarklinik provides treatment for arachnoiditis in Saratov , Russia, treatment of post-traumatic arachnoiditis using hardware and non-hardware techniques. With complex treatment, a significant improvement in the condition is possible. Sarklinik knows how to effectively treat arachnoiditis. Consultations, comprehensive medical care.
In any case, it is necessary to carry out differential diagnosis and establish a true diagnosis, and only then carry out treatment. Differential diagnosis is varied, it is necessary to exclude various diagnoses: somatoform autonomic dysfunction, vegetative-vascular dystonia, cerebral vascular atherosclerosis, arterial hypertension, hypertension, cerebral aneurysm, age-related changes, stress, auditory neuritis, neurosis, depressive neurosis, cervical osteochondrosis spine, anemia, diseases of the cardiovascular system, arrhythmia, kidney disease, brain tumors, diseases of the endocrine system, taking a number of medications, consequences of brain injuries, concussions, otosclerosis, labyrinthitis, tumors of the tympanic cavity, Meniere's disease, acute trauma, exostoses , fistula, autoimmune diseases, exposure to loud noises at work or at home, the effects of ototoxic drugs, temporomandibular joint diseases.
Of course, it is necessary to conduct an MRI of the brain, REG, EEG, MRI of the cervical spine, vascular angiography, audiogram, CBC, TAM, glycated hemoglobin, cholesterol, lipoproteins (lipoproteins).
Tinnitus (tinnitus) and noise in the head make it very difficult to live a full life, so you should definitely consult a doctor.
Sign up for a consultation. There are contraindications. Specialist consultation is required.
Related posts:
Blinking, bending, twitching shoulders, obsessive movements: treatment
STOSN, anxious expectation of failure syndrome, erection weakened, disappeared
Urinary incontinence at night in a boy, what to do, how to treat it in Saratov, Moscow, Russia
Treatment of vascular erectile dysfunction in Saratov, Russia
VSD extrasystoles, panic attacks, fear, heart turns over in the chest, osteochondrosis
Comments ()
Diagnostic methods
In the early stages, it is difficult to detect the disease. Since it is most often caused by damage to the paranasal sinuses, radiography or MRI of the sinuses is indicated. During the examination, slight parietal swelling of the mucous membrane of the sphenoid sinus is revealed. Damage to the posterior cells of the ethmoidal labyrinth may also be detected. Hardware diagnostics include:
Visometry;- Perimetry;
- Study of pupillary reaction;
- Ophthalmoscopy;
- Craniography;
- Pneumocisternography.
In the case of a unilateral form, the examination is repeated after 2 weeks to exclude delayed damage to the second eye. The pathology may be accompanied by migrating defects. Individual changes are determined in other areas.
General information
Arachnoiditis is an infectious disease of the central nervous system and is a serous inflammation of the structures of the arachnoid membrane of the brain or spinal cord. The arachnoid membranes do not have their own vascular system, therefore the lesions are not isolated, and infectious processes spread from the dura or soft meninges, therefore the symptoms of arachnoiditis are conclusively attributed to the serous type of meningitis .
The pathology was described in most detail by the German doctor Benninghaus, and the term was first used in the dissertation of A.T. Tarasenkov, who studied the signs of cerebral inflammation and arachnoiditis in particular. Some scientists call this disease serous meningitis, but according to ICD-10 it is assigned the code G00 and the name bacterial arachnoiditis , G03 - which includes meningitis due to other or unspecified causes, including arachnoiditis , meningitis , leptomeningitis , pachymeningitis , as well as G03 .9 – for unspecified meningitis – spinal arachnoiditis NOS (no additional instructions).
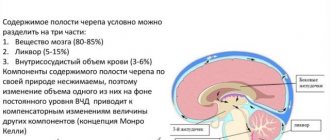
The brain has three membranes: hard, arachnoid and soft. Thanks to the hard one, sinuses are formed for the outflow of venous blood, the soft one provides trophism, and the arachnoid one is necessary for the circulation of cerebrospinal fluid . It is located above the gyri, but does not penetrate the sulci of the brain and separates the subarachnoid and subdural space. Its structure contains arachnoidendothelial cells, as well as bundles of collagen fibrils of varying thickness and quantity.
Histology of the meninges
Diet for arachnoiditis
Diet for the nervous system
- Efficacy: therapeutic effect after 2 months
- Timing: constantly
- Cost of food: 1700-1800 rubles per week
Treatment of arachnoiditis is best combined with a diet based on the principles of healthy eating:
- limited consumption of seasonings and salt;
- products containing refined sugar, butter, flour are excluded;
- meat should be of dietary grades - rabbit, turkey, chicken, etc.;
- no sausages or smoked meats;
- there should be fresh vegetables and fruits on the table;
- You need to enrich your diet with baked potatoes, cabbage and carrot salads, spicy and leafy greens;
- you need to add currants, sea buckthorn, persimmons, grapes, and raisins to dishes and teas.
Pathogenesis of arachnoiditis
With injuries and bruises of the brain, subarachnoid hemorrhages and damage to the soft meninges occur, as a result of which tissue decay products enter the subarachnoid space. Subsequently, the arachnoid membrane becomes denser and thickens. Adhesions and adhesions appear between the arachnoid membrane and the pia mater. Then the circulation of cerebral fluid is disrupted, cyst-like expansions are formed, and the ventricles of the brain enlarge.
Development mechanism
Pathogenesis is associated with the influence of an infectious agent on the membranes of the brain, most often viruses. In this case, the arachnoid membrane is affected first, and then the soft membrane. The most pronounced changes in the structure of nervous tissues are in the optic nerves and the chiasm zone. The local inflammatory process leads to increased vascular permeability and dilation. In the meninges, exudation and the formation of cellular infiltrates begin. This leads to hypoxia and allergic reactions.
Subsequently, inflammation leads to fibroplastic changes in the arachnoid in the area of the optic nerve and optic chiasm. The connective tissue grows, causing extensive synechiae to form between the arachnoid and dura mater. Cysts with serous contents and fibrous cords are also formed. Cystic formations can be either large single or multiple small ones. If they surround the chiasma on all sides, this causes compression of the optic nerves. Compression is the main cause of degenerative changes and atrophy.
Tests and diagnostics
When making a diagnosis, a differential diagnosis must be made with abscesses and neoplasms in the posterior cranial fossa or other parts of the brain. To determine arachnoiditis, it is important to conduct a comprehensive and detailed examination of the patient.
Electroencephalography , angiography , pneumoencephalogram , scintigraphy , survey craniograms , skull x-ray, myelography , CT, MRI are indicative These studies make it possible to identify intracranial hypertension, local changes in biopotentials, expansion of the subarachnoid space, cisterns and ventricles of the brain, cystic formations and focal changes in the brain substance. Only if there is no congestion in the fundus, then a lumbar puncture to detect moderate lymphocytic pleocytosis and slight protein-cell dissociation. In addition, it may be necessary to perform an index and finger-nose test.
Diagnosis of arachnoiditis
The diagnosis of cerebral arachnoiditis is made based on the results of the following studies:
1. Neurological examination. Identify symptoms of brain damage.
2. Cerebrospinal fluid analysis. Performed under local anesthesia. A special needle is used to make a puncture in the lumbar region and take 1-2 milliliters of cerebrospinal fluid.
3. Electroencephalography. With arachnoiditis, signs of brain irritation are detected.
4. MRI or CT scan of the spinal cord or brain. They allow you to study the structure of these organs layer by layer and identify their condition at the current time.
Cerebral arachnoiditis usually does not have specific signs (except for hydrocephalus), but using these techniques, other diseases, such as a brain tumor, can be excluded.
Prevention of arachnoiditis
Arachnoiditis, the symptoms and treatments for which are described above, can be prevented. In order to reduce the likelihood of developing the disease to a minimum, the following recommendations must be followed:
- strengthen the immune system, harden the body;
- to refuse from bad habits;
- Healthy food;
- observe the work and rest schedule;
- If possible, avoid getting into stressful situations;
- walk more, move, play sports;
- promptly treat diseases of a traumatic or infectious nature;
- periodically sanitize foci of chronic infection in the body;
- undergo regular preventive examinations with an ophthalmologist and ENT specialist.
Health to you!