Make an appointment by phone: +7 (343) 355-56-57
+7
- About the disease
- Cost of services
- Sign up
- About the disease
- Prices
- Sign up
Paroxysmal ventricular tachycardia (PVT)
is an absolutely life-threatening rhythm disorder that requires immediate hospitalization.
Along with ventricular fibrillation, ventricular tachycardia is the leading cause of circulatory arrest and sudden death in Russia and in the world.
REASONS FOR THE DEVELOPMENT OF PAROXYSMAL VENTRICULAR TACHYCARDIA
Reasons for the development of PVT:
1. severe diseases of the cardiovascular system:
- myocardial infarction
- cardiomyopathy
- heart defects
- heart failure
- myocarditis (severe)
2. toxic factors:
- frequent alcohol consumption in significant quantities
- inhalation of glue fumes
- narcotic substances
3. cardiac injury
4. medications: cardiac glycosides, antidepressants, flecainide, fluoroquinolones
5. congenital anomalies of the cardiac conduction system (Brugada syndrome)
6. idiopathic VT – the cause of development is unclear
Causes
Torsade de pointes, characterized by a prolonged QT interval, may be congenital or acquired as a result of the action of drugs. Genetic variants include:
- hereditary syndromes that may be accompanied by deafness;
- gene pathology - today scientists have discovered six more hereditary defects associated with prolongation of the PQ interval. These genes encode transmembrane K and/or Na channels.
Hereditary factors are rare; more often the occurrence of pathology is influenced by the use of drugs. These include:
- antiarrhythmic medications;
- phenothiazines, butyrophenones;
- antifungal drugs;
- antihistamines;
- some are antiviral;
- antibiotics, especially macrolides;
- antidepressants;
- organophosphorus compounds (OPS);
- cocaine.
Provoking factors may be poor nutrition or starvation, alcoholism, endocrine and cardiovascular diseases, subarachnoid hemorrhage. Existing genetic pathologies, congenital heart defects, and concomitant somatic defects can cause an attack. The most common causes are listed above, but each case should be considered individually by your doctor.
SYMPTOMS OF PAROXYSMAL VENTRICULAR TACHYCARDIA AND FIRST AID
If circulatory arrest develops in such patients, resuscitation measures must be started immediately and carried out until doctors arrive. The only effective way to interrupt this arrhythmia is defibrillation
(that is, the application of electric current by a special defibrillator device). But while waiting for the resuscitation team, everyone should be able to help such patients.
Clinically, PVT is manifested by a sudden loss of consciousness and circulatory arrest, that is, such patients do not breathe, they have no pulse and consciousness. In this situation, you must immediately punch the patient's sternum (the narrow, flat bone in the center of the chest) and begin chest compressions (CCM).
.
How is NMS performed:
- the patient should lie on a hard surface
- the person providing assistance intensively presses on the patient’s chest with a frequency of 100 compressions per minute and to a depth of 5-6 cm
- resuscitation is carried out until the arrival of the medical team
Indirect cardiac massage performs the function of a pump and the hands of the resuscitator, in essence, replace the patient’s stopped heart.
Often paroxysms of VT are manifested by recurrent (that is, repeated) fainting, with spontaneous (that is, independent) restoration of consciousness.
Follow-up therapy and prevention
Subsequent therapy is aimed at preventing the recurrence of ventricular fibrillation. After all, the result can be fatal without timely help. International heart health organizations recommend regular use of β-blockers. The effectiveness of their use is 68–90%. Sodium channel blockers, such as Meksitylen, also have a good effect.
If syncope persists during β-blocker therapy, implantation of a pacemaker-defibrillator is indicated. It must be remembered that this operation does not mean the abolition of drug treatment.
The main advice to patients and their relatives is to know the list of drugs that prolong the QT interval and avoid taking them.
The last resort treatment is left-sided sympathectomy at the level of the cervicothoracic spine.
MECHANISMS OF DEVELOPMENT OF PAROXYSMAL VENTRICULAR TACHYCARDIA
Why does a patient's heart stop during PVT?
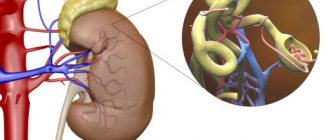
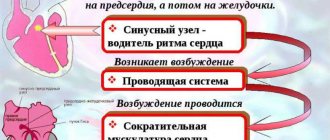
The mechanism of development of this cardiac arrhythmia is as follows. Due to the damaging factor, foci of damage appear in the myocardium (heart muscle), similar to microinfarctions, changing the overall “electrical background” of the heart.
In this regard, around such foci or in them themselves there are paroxysms of ventricular tachycardia. They cause the heart to beat at a high frequency and the main source of this arrhythmia is in the myocardium of the ventricles of the heart. Unlike the atria, the ventricles are “designed” to work at a frequency of 60-80-100 per minute. With VT, the heart rate exceeds 200 per minute and the heart, of course, cannot work in this mode for a long time. And then it stops. This is sudden cardiac death.
Such a patient can be saved by a timely applied current discharge to the chest through a defibrillator. Many countries around the world have launched a program to prevent sudden cardiac death and train the population in first aid, including in case of sudden cardiac arrest. Unfortunately, in our country only medical workers are skilled in this manipulation.
Pathophysiology: mechanism of occurrence of disorders
Ari develops by prolonging the repolarization phase. The electrocardiogram, in addition to prolongation of the QT interval, shows the presence of noticeable U waves at rest. These ECG changes reflect prolonged repolarization with the development of early subsequent depolarization.
Pathology can lead to hemorrhages into the ventricular tissue, causing myocardial infarction.
Repolarization occurs in the myocardium when the number of positive ions (mainly potassium) exceeds the number of sodium and calcium ions, the concentration of which should decrease. Potassium channel dysfunction causes intracellular excess positive charge, which delays ventricular repolarization. This state of the myocardium leads to the emergence of a specific type of recurrent arrhythmic tachycardia.
TREATMENT OF PAROXYSMAL VENTRICULAR TACHYCARDIA
If VT develops, emergency hospitalization and immediate restoration of sinus rhythm are necessary.
The rhythm is restored either with medication or by
electropulse therapy (EPT)
.
An antiarrhythmic drug (amiodarone (cordarone)) is administered intravenously. Then, to prevent the re-development of arrhythmia, the patient takes this drug in monotherapy or with other drugs.
EIT uses a current discharge through the chest. The patient is put into medicated sleep, then defibrillator electrodes are applied and a shock is applied. This method is based on the fact that the basis for the development of PVT is the electrical instability of the myocardium.
The current discharge produces a kind of “shake-up” of the myocardium, suppressing “unauthorized” sources of arrhythmia. After EIT, also to prevent relapse (re-development) of arrhythmia, the patient takes antiarrhythmic drugs.
of implantable cardioverter-defibrillators (ICDs) is based on the principle of EIT.
with PVT.
A small device resembling a pacemaker is implanted under the skin, and electrodes from it “descend” into the heart through the blood vessels. If there is no arrhythmia, then this device is “silent”. If a paroxysm of ventricular tachycardia develops, the ICD is triggered and delivers a current discharge to the heart, thereby suppressing the source of the arrhythmia. Thanks to the ICD, the patient is protected from the risk of sudden cardiac arrest and, in fact, carries a small defibrillator with him at all times. The implantation of these devices is carried out by cardiovascular surgeons in specialized arrhythmology centers, which include the New Hospital.
ICD implantation does not require anesthesia; it is performed through a small incision in the skin; the patient can engage in normal activities the very next day after surgery. However, after ICD implantation, the patient must be under the supervision of a cardiac surgeon-arrhythmologist, and such supervision is also available in our clinic.
Paroxysmal ventricular tachycardia can be unstable, i.e. short-term, and go away on its own. But observation and treatment are required, since there is a risk of its re-development and threat to the patient’s life.
Sometimes cardiac surgeons resort to ablation of PVT foci, that is, they “cauterize” the arrhythmogenic focus using cold exposure (cryodestruction) or laser. These manipulations are also performed in cardiac surgery hospitals. And further observation and treatment is required under the guidance of a cardiac surgeon-arrhythmologist.
A special type of VT is paroxysms of this rhythm disorder against the background of congenital anomalies of the conduction system of the heart (for example, with Brugada syndrome). Cardiac conduction system (CCS)
- “electrical wiring” in the heart that converts an electrical impulse into myocardial contraction. With Brugada syndrome, the patient is born “prepared” to develop life-threatening arrhythmias, incl. PVT.
The “wiring” in such patients “sparks.” This is a paroxysm of arrhythmia
. Before exposure to a provoking factor (for example, taking medication), the patient is healthy, but in the event of contact with this factor, the preparation for arrhythmia is realized and it develops. Often the first and last time in my life.
Therefore, cardiologists and arrhythmologists pay such attention to family history. In the presence of congenital anomalies of PSS, the fact of death at a young age from unknown causes of one of the relatives, especially the first or second degree of kinship, is alarming.
The presence of an electrocardiogram (ECG) taken at a speed of 50 mm/sec is a mandatory part of any consultation with a cardiologist and arrhythmologist. Already when analyzing a regular ECG, the doctor recognizes the signs of Brugada syndrome and helps his patient in a timely manner.
Introduction
Polymorphic ventricular tachycardia, or torsade de pointes (TdP), is a potentially life-threatening tachyarrhythmia that can lead to sudden cardiac death (SCD), and is closely associated with prolongation of the QT interval [1, 2]. There are two large etiological groups that determine the development of prolongation of the QT interval and TdP: congenital and acquired [3]. Among acquired causes, the most common drug-related development of QT interval prolongation and TdP [4].
Prevalence
To date, it is known that drugs that contribute to prolongation of the QT interval and the development of TdP are available in almost all existing groups of drugs, accounting for 2 to 3% of the total number of drugs used [5]. However, the prevalence of drug-induced prolongation of the QT interval and TdP in the general population remains unknown and requires further study. The literature contains only data regarding the prevalence of drug-induced prolongation of the QT interval and the development of TdP in individual countries. Thus, a study by the Swedish Medical Products Agency (MPA; Swedish) [6] attempted to determine the total number of cases of drug-induced ventricular arrhythmias by monitoring 4.2 million patients for 28 days. patients in 32 medical institutions. All episodes of ventricular arrhythmias caused by drugs and identified upon admission, as well as during ECG monitoring during treatment, were recorded. The resulting figure was 3.3 cases per 1 million patients during a 28-day observation period, or 4 cases per 100 thousand people per year. Another Swedish study by S. Astrom-Lilja et al. [7], having analyzed data from the system of reporting drug side effects from 1991 to 2006, revealed that out of 61,788 recorded cases, 101 were drug-induced TdR. A study by G. Sarganas et al. [8] showed that in 2014 in Berlin there were 2.5 cases of drug-induced prolongation of QT/TdP per 1 million male population of the city and 4 per 1 million female population. And in a population-based study in southwestern France, the incidence of drug-induced TdR was estimated at 5–7% of all cases of ventricular tachyarrhythmias or SCD [9].
There is evidence that QT prolongation is most common among hospitalized patients, especially among intensive care unit patients [10], ranging from 28 to 52% [11, 12]. The incidence of TdP among hospitalized patients has been much less studied. D. Pickhamm et al. [13], who observed patients in intensive care units for 2 months, reported 1 case in 154 patients (0.6%), which amounted to 1 of 16 cases of cardiac arrest in these departments.
Medicines that are associated with the development of TdP
The most well-known and frequently used groups of drugs in both outpatient and inpatient practice, which have representatives that contribute to the development of prolongation of the QT/TdP interval, include antiarrhythmics (IA-, IC- and III classes), antipsychotics, antidepressants, antibacterial drugs (macrolides and fluoroquinolones), antihistamines, antitumor, antifungal drugs, prokinetics, lipid-lowering drugs, diuretics (except potassium-sparing). The list of drugs that contribute to the development of TdP is constantly updated, and the efforts of specialists from the University of Arizona (Arizona Center for Education and Research on Therapeutics, AzCERT), who developed the website CredibleMeds.org, allow you to monitor the current list of drugs associated with the development of TdP. All drugs presented on the site are divided into groups depending on whether they are associated with a known, possible or conditional risk of developing QT prolongation/TdP. Drugs with a known risk are those for which there is substantial evidence supporting their QT-prolonging effects and a clear association with the risk of TdP, even when the drugs are taken exactly as prescribed in the official labeling. The list of drugs with a possible risk includes drugs for which there is substantial evidence that they may cause QT prolongation, but at present there is insufficient evidence that these drugs, when used according to official labeling, are associated with a risk of TdP. Finally, for drugs with a conditional risk, there is substantial evidence that their use is associated with a risk of TdR, but only under certain conditions (eg, drug overdose, hypokalemia, congenital QT prolongation or drug interactions). Lists of drugs with known, probable and possible risks of developing TdP, as well as the number of cases of TdP associated with taking a particular drug, are presented in Table. 1–3.
The use of certain antipsychotics is known to be associated with an increased risk of SCD due to the development of TdP [10]. Thus, in a population-based case–control study, SM Straus et al. [14] reviewed 150 medical records and found that antipsychotic drug use was associated with a significantly increased risk of SCD (odds ratio [OR], 3.3; 95% confidence interval [CI], 1.8–6.2), with the risk was highest among patients receiving butyrophenone drugs (haloperidol).
An increased risk of SCD was reported by WA Ray et al. [15] according to a retrospective cohort study, and the risk was associated with the use of both typical and atypical antipsychotic drugs, similar results were obtained in other studies [16, 17], and CS Wu et al. [18] found that antipsychotic drugs with the greatest ability to inhibit IKr were associated with the highest risk of ventricular arrhythmias and/or SCD. Meta-analysis by F. Salvo et al. [19] showed that different antipsychotics were associated with different levels of risk for developing VVS and were distributed as follows: thioridazine > clozapine > rissperidone > haloperidol > olanzapine > quetiapine.
Macrolide antibiotics are also associated with an increased risk of SCD. JY Cheng et al. [20] conducted a meta-analysis of 33 studies, including almost 21 million patients, assessing the association between macrolide antibiotic use and cardiovascular risk. It was found that patients taking macrolides had an increased risk of VVS or ventricular tachyarrhythmias (2.42; 95% CI - 1.61-3.63), VVS (2.52; 95% CI - 1.91-3. 31) and cardiovascular death (1.31; 95% CI – 1.06–1.62) compared with persons not taking macrolide antibiotics.
In a study by W. A. Ray et al. [21] found that in the group of patients receiving erythromycin, the adjusted rate of SCD was 2 times higher than in individuals who did not use this drug. In addition, the adjusted incidence of SCD was 5 times higher among patients who, in addition to erythromycin, also used drugs that suppress the activity of cytochrome P450 enzymes. A similar study of patients taking azithromycin found an increased risk of cardiovascular death (hazard ratio [HR], 2.88; 95% CI, 1.79 to 4.63; p<0.001) and all-cause death (HR). – 1.85; 95% CI – 1.25–2.75; p<0.0021) compared with patients who did not take this antibiotic [22]. Clarithromycin is also associated with an increased risk of cardiovascular events (hospitalization for acute coronary syndrome, decompensated heart failure [HF], life-threatening cardiac arrhythmias, or SCD) [23].
Mechanisms of development of drug-induced TdP
It is known that the mechanism of development of TdP is based on prolongation of ventricular repolarization, which leads to an increase in the duration of the action potential (AP) and is manifested on the ECG by prolongation of the QTc interval [10]. Activation of inward depolarizing currents and prolongation of APs contribute to increased susceptibility to early afterdepolarization, manifested as depolarizing oscillations in membrane voltage during phase 2 or 3 of AP.
In turn, the occurrence of early post-depolarizations can lead to the generation of premature APs, which can initiate the development of TdP through the reentry mechanism.
The basis for prolongation of ventricular repolarization and increase in AP duration is a decrease in outgoing or increase in incoming current during the plateau phase or the slow phase of AP repolarization (or both) [10]. Drugs induce TdP by inhibiting the outward current through specific potassium channels (primarily the fast component of the delayed rectifying potassium current [ICr]), which leads to prolongation of AP [10]. Some drugs (for example, ibutilide) prolong ventricular PP also due to the activation of the slow sodium current (INa) during the 2nd phase of PP [10]. It is thought that the early afterdepolarization that triggers TdP may be caused by increased inward calcium current through calcium channels that become reactivated as a result of increased AP duration.
Although inhibition of IKr and/or activation of INa, as well as prolongation of ventricular repolarization are required for the development of TdP, the presence of these factors alone is not sufficient to cause arrhythmia. Many patients taking drugs that inhibit IKr develop QTc prolongation, but not TdP.
Currently, researchers believe that the main factor increasing the likelihood of developing TdP is repolarization heterogeneity (repolarization dispersion or refractoriness) [1]. It is known that cardiac muscle is characterized by electrical heterogeneity and the duration of AP varies according to three main types of ventricular cells (epicardial, myocardial, endocardial), which differ in repolarization characteristics in phases 1 and 3 of AP [10]. The risk of drug-induced TdP is thought to be increased in patients with increased transmural heterogeneity of ventricular repolarization [10]. In addition, the risk of TdP may depend on action potential instability (rapid fluctuations in action potential duration) and the degree of action potential triangulation (slow repolarization at which the AP becomes triangular in shape) [10].
Another important concept regarding drug-induced TdP is the so-called. repolarization reserve [24]. It is known that under normal conditions there are many redundant mechanisms that maintain normal ventricular repolarization: IKr and other repolarization currents (slow component of delayed rectifying potassium current, INa, abnormal rectifying current, transient outgoing current). Inhibition of IKr drugs in the presence of an unchanged repolarization reserve rarely leads to TdP, because redundancy of repolarization currents minimizes the effect of IKr inhibition. However, in the presence of factors that reduce repolarization reserve (risk factors for the development of TdP), IKr inhibition may have a much greater effect on prolonging ventricular repolarization and promoting the development of TdP.
Clinical presentation, diagnosis, differential diagnosis of drug-induced TdP
Clinical symptoms associated with the development of TdP are similar to those of other tachyarrhythmias and are based on an increase in heart rate (HR) with a subsequent change in blood pressure and cardiac output, manifesting itself in the form of episodes of dizziness, palpitations, shortness of breath, fainting, an episode of chest pain ( in patients with coronary artery atherosclerosis), as well as seizures, hypotension, or TdP does not have any clinical manifestations at all [10]. Transient episodes of TdP lasting more than 10 seconds are accompanied by the development of syncope, but failure to restore heart rhythm within 1-2 minutes can develop into ventricular fibrillation and lead to death - SCD. Over the past two decades, due to the development of SCD as a result of TdP, several drugs have been withdrawn from the US pharmaceutical market, including. terfenadine, astemizole, grepafloxacin, cisapride, levomethadyl and mesoridazine.
Diagnosis of TdP is based on an ECG pattern that registers polymorphic ventricular tachycardia with an irregular rhythm and wide polymorphic ventricular complexes with varying amplitude (as if twisting around the isoelectric line) at a speed of 160–240 per minute under conditions of an extended QTc interval [10]. In addition, the development of TdP is often preceded by alternating RR intervals of the “short-long-short” type, resulting from the development of premature ventricular contraction followed by a compensatory pause, which is followed by the first “volley” of TdP.
Determining the QT interval also has its own characteristics. It is considered necessary to determine not the absolute indicator of the duration of the interval, but the so-called. corrected QT (QTc) [10]. The need to correct the QT interval is due to its inverse dependence on heart rate: with an increase in heart rate, the duration of the QT interval decreases, and vice versa. To determine the value of QTc, the Bazett formula is most often used: QTc = QT√RR.
Differential diagnosis of drug-induced TdP involves the exclusion of other tachyarrhythmias (atrial fibrillation, atrial flutter, atrial tachycardia, recurrent AV node reentry tachycardia, non-TdR polymorphic ventricular tachycardia, sinus tachycardia, functional tachycardia, monomorphic ventricular tachycardia, ventricular fibrillation) and is based on analysis ECG [10]. Thus, the presence of QTc interval prolongation in a patient before or shortly after an episode of polymorphic ventricular tachycardia allows us to distinguish TdP from non-TdP polymorphic ventricular tachycardia.
An important criterion for suspecting the drug-induced nature of TdP is to study the list of medications used by the patient in order to determine the presence of a drug that can cause TdP or at least has the ability to induce prolongation of the QTc interval [10]. And here it is necessary to remember that the development of TdP associated with the use of a particular drug depends on the method of taking the drug. Thus, when intravenous drug therapy is used, the development of TdP, as a rule, coincides with the expected time of peak drug concentration in blood plasma [10]. For example, many cases of TdP caused by intravenous erythromycin have occurred during the infusion or within 30 minutes of completion of the infusion [10]. TdP induced by intravenous haloperidol occurs 15–220 minutes after infusion, and ibutilide induced 2–60 minutes after drug administration [10]. In turn, TdP caused by oral forms of drugs can be delayed. Thus, an analysis of 144 published articles describing a total of 249 patients who developed TdP [25] showed that the use of non-cardiac drugs was associated with the development of 18% of cases occurring within the first 72 hours after the start of oral therapy, 42% of cases occurred between days 3 and 30, and 40% occurred more than 30 days after initiation of oral therapy.
An equally important diagnostic point is to assess whether the patient has concomitant risk factors for the development of TdP, which significantly increase the likelihood of life-threatening tachyarrhythmia.
Risk factors for developing TdP
Drug-induced TdP is extremely rare in patients without underlying risk factors. Thus, D. Zeltser et al. [25], having analyzed cases of drug-induced TdP in 249 patients, showed that almost 100% of them had at least 1 risk factor, and 71% had at least 3 factors.
Currently, the following risk factors for the development of drug-induced TdP are known [26–29]: older age, bradycardia, simultaneous use of >1 drugs that contribute to the development of prolongation of the QTc/TdP interval, increased plasma concentrations of QT-prolonging drugs due to drug interactions or inadequate dose adjustment for renal/liver dysfunction, female gender, HF with reduced ejection fraction (EF), history of drug-induced TdP, hypocalcemia, hypokalemia, hypomagnesemia, increase in QTc interval by >60 ms compared with baseline, QTc interval > 500 ms, rapid intravenous infusion of drugs that prolong QTc, sepsis, and finally, self-prolongation of the QTc interval on the ECG is also identified as a risk factor for the development of TdP.
There are many studies in the literature demonstrating the significant influence of risk factors on the likelihood of developing TdP. Thus, the risk of TdP increases markedly when the QTc interval exceeds 500 ms, and when the QTc interval is <500 ms, TdP occurs quite rarely [26–29]. Also, the risk of TdP increases when the QTc interval during therapy increases by >60 ms compared with the baseline value [28]. Returning to the study [25], we can find that of the 249 patients who developed TdP induced by drugs, more than two thirds were women, 41% had diseases of the cardiovascular system (myocardial infarction, heart failure, cardiomyopathy), 28% had hypokalemia, 19 % – drug overdose or lack of dose adjustment for liver/kidney dysfunction, 18% – family history of long QT syndrome, drug-induced TdP/prolongation of the QT interval in history, 35% – drug interactions.
The reasons for the increased risk of drug-induced TdP in individuals with certain risk factors continue to be studied. In women, the increased risk of TdP is thought to be due to the proarrhythmogenic effects of estrogen, while men are protected by the antiarrhythmogenic effects of testosterone [30, 31]. It is known that the basic duration of the OTc interval in women is longer than in men, which manifests itself precisely during puberty [32, 33]. In a study by RR Makkar et al. [34] of 332 patients with TdP associated with antiarrhythmic drugs, 70% were women. Other studies have confirmed the predisposition of women to TdP associated with the use of azimilide, dofetilide, erythromycin, ibutilide, quinidine, sotalol and terfenadine [35–38].
HF with reduced EF is one of the main risk factors for the development of drug-induced TdP [10]. The mechanisms underlying the increased risk of TdP in this group of patients continue to be studied. It is assumed that in individuals with HF with reduced EF, potassium channel activity is suppressed, which contributes to prolongation of ventricular repolarization [10].
The most important risk factor is an increase in the concentration of TdP-inducing drugs in the blood plasma. Most cases of TdP associated with the use of erythromycin or haloperidol occurred after intravenous administration of the drug as a result of higher peak plasma concentrations [10]. The development of TdP was also facilitated by the lack of adequate drug dose adjustment in the presence of kidney disease in cases of therapy with dofetilide, levofloxacin, procainamide and sotalol [10]. The list of drugs that contribute to the development of TdP and require dose adjustment when used in patients with kidney/liver diseases is presented in Table. 4.
Drug interactions are an important risk factor for the development of drug-induced TdP [10].
The literature describes numerous cases of TdP that developed as a result of an increase in the plasma concentration of a drug that was a substrate for the cytochrome P450 system when used in combination with a drug that inhibits its activity. Thus, the US FDA database contains information on 25 cases of TdP associated with terfenadine, with 9 patients receiving concomitant therapy with ketoconazole or itraconazole, which are known to inhibit the metabolism of terfenadine [38]. Drugs associated with the risk of developing TdP that are substrates for the cytochrome P450 system are listed in Table. 4.
It is believed that the use of combinations of drugs that prolong the QT interval may increase the risk of TdP, although the results of studies on this issue are highly inconsistent [39–42]. It is known that the simultaneous use of several drugs that prolong the QT interval is relatively common. Thus, a retrospective cohort study by LH Curtis et al. [39] showed that of 1.1 million patients with a prescription for a QT-prolonging drug, 9.4% received a prescription for a second drug that also prolongs the QT interval or impairs the metabolism of a QT-prolonging drug. And in the study by KY Tay et al. [40] found that 15% of prescriptions filled in the emergency department included drugs that prolong the QTc interval, and about 10% of these included ≥2 drugs that prolong the QTc interval.
JE Tisdale et al. [29], having analyzed data from intensive care unit patients who received ≥2 drugs that prolong the QTc interval, found that the OR for the development of TdP in such patients compared with those who did not receive therapy with QT-prolonging drugs was 2.6 (95% CI – 1.9–5.6; p=0.02). However, there was no evidence that the use of a combination of drugs that prolong the QTc interval or increase the risk of developing TdP was accompanied by a higher risk of developing QTc/TdP prolongation compared with monotherapy [10]. A review of the literature [41] showed that the use of several antipsychotic drugs was not associated with prolongation of the QTc interval. In a population-based cohort study of MN, Niemeijer et al. [42], which included 13,000 patients, found that adding a second or third drug that prolongs the QTc interval to initial therapy had very little additional prolonging effect on the QTc interval.
Data published in the literature suggest that some patients with drug-induced TdP have a genetic predisposition [43, 44]. To date, 15 specific genetic defects underlying congenital long QT interval syndrome have been identified [43]. Gene mutations that predispose to the development of congenital long QT syndrome have been found in 10–15% of patients who have experienced drug-induced TdP [44].
Prevention of drug-related TdR
The risk of developing drug-related TdP can be prevented by identifying and minimizing the influence of risk factors associated with the development of TdP [45]. In this case it is necessary [10]:
- carry out dose adjustments of QT-prolonging drugs metabolized by the kidneys/liver in patients with kidney/liver disease;
- avoid simultaneous administration of several QT-prolonging drugs;
- avoid simultaneous administration of QT-prolonging drugs with drugs that slow down their metabolism by inhibiting enzymes of the cytochrome P450 system;
- Avoid prescribing QT-prolonging drugs to patients with congenital long QT syndrome;
- Avoid prescribing QT-prolonging drugs in patients with a history of TdP;
- Avoid prescribing QT-prolonging drugs to patients with a baseline QT interval >450 ms;
- Discontinue the QT-prolonging drug if the patient's QTc interval increases to >500 ms;
- monitor and maintain serum calcium concentrations within normal limits;
- monitor and maintain serum magnesium concentrations ≥2 mg/dL;
- monitor and maintain serum potassium concentration ≥4 mEq/L;
- reduce dose or discontinue use of QT-prolonging drug if QTc increases > 60 ms from baseline;
- If possible, avoid the use of QT-prolonging drugs in persons with HF with reduced EF, especially in patients with EF <20%.
Before initiating therapy with a drug known to cause TdP, the patient should have a 12-lead ECG and QTc interval followed by ECG monitoring, avoiding QTc interval prolongation ≥500 ms [46]. In hospitalized patients receiving drugs known to cause TdP, the QTc interval should be monitored daily [46]. In patients receiving long-term oral therapy with drugs known to cause TdP, an ECG is performed regularly at 3 to 6 months, depending on the presence or absence of other risk factors [46].
An important preventive role is played by the awareness of the patient taking drugs that contribute to the development of TdP about their possible side effect, such as an increase in heart rate, and the need to consult a doctor if the heart rate increases to 100–120 per minute or episodes of dizziness, anxiety, fatigue, and weakness appear. , shortness of breath, chest pain [10]. Patients taking medications that may cause TdP should be warned about the dangers of using over-the-counter medications without first consulting their physician.
Treatment of drug-related TdR
If TdR develops, therapy with drugs that contribute to its development should be discontinued [47]. Hypokalemia, hypomagnesemia, or hypocalcemia should be corrected with intravenous potassium, magnesium, or calcium, respectively. Electropulse therapy is indicated for hemodynamically unstable patients with TdP [47]. In patients with TdP and stable hemodynamics, intravenous magnesium sulfate is indicated [10]. Temporary pacing is effective in reversing TdP secondary to bradycardia; intravenous isoprenaline can also reverse TdP by increasing the heart rate and shortening the QT interval [10].
Conclusion
The development of TdP poses a serious threat to the lives of patients, being associated with an increased risk of developing SCD. Most of the currently known pharmacological groups have representatives that have the ability to cause TdP. It is precisely because of the TdP-inducing effect and the development of SCD that the use of some of them has been limited and even prohibited (terfenadine, astemizole, grepafloxacin, etc.), while research on others is ongoing. The presence of risk factors for TdP plays a huge role in increasing the risk of developing polymorphic ventricular tachycardia in individuals taking drugs that have a TdP-inducing effect, which must be taken into account when prescribing such drugs. Most of the risk factors are modifiable and should be corrected, which is of critical preventive value, helping to prevent the development of TdP. In addition, timely informing patients, aimed at creating alertness regarding the possibility of development, features of manifestation and ways to prevent the development of drug-induced TdP, is of no less preventive importance and requires appropriate knowledge and alertness from practicing physicians.
PREVENTION OF PAROXYSMAL VENTRICULAR TACHYCARDIA
- Knowledge of family history.
If there have been sudden deaths in the family (especially in first- or second-degree relatives at a young age), then contact a cardiologist to identify the risk of developing PVT. - Prevention of the development of cardiovascular diseases
(heart attack, cardiomyopathy): blood pressure control, smoking cessation, prevention and treatment of viral diseases - Healthy lifestyle
(no smoking, alcohol) - Taking antiarrhythmic drugs and installing implantable cardioverter defibrillators
Patients with this pathology are observed and treated by cardiologists, arrhythmologists and cardiac surgeons. All these services are available at our New Hospital clinic.
Diagnostics
If you feel a sudden increase in heart rate, you should immediately consult a doctor. After a physical examination, the patient is sent for an ECG to accurately determine the diagnosis.
As additional diagnostics use:
- daily ECG monitoring;
- EPI (electrophysiological study of the heart);
- ECHO;
- Coronary angiography is a radiopaque research method.
The doctor may order laboratory tests, the results of which will indicate concomitant pathologies.
Timely diagnosis is a fundamental factor in successful treatment of the disease. Do not ignore your ailments - seek help from the specialists of the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency!