Causes
The causes of hypercapnia are varied; they are divided into several large groups:
- Disturbances in the mechanics of respiratory movements in certain pathological conditions [with botulism, multiple sclerosis, poliomyelitis, muscular dystrophy, myasthenia gravis, the use of muscle relaxants, Pickwick's syndrome, morbid obesity, fractures of the sternum and (or) ribs, scoliosis, severe pneumosclerosis].
- Inhibition of the respiratory center in the brain stem (with the use of narcotic analgesics and general anesthetics, circulatory arrest, damage to the central nervous system, prolonged oxygen inhalation).
- Gas exchange disorders in the lung tissue (with Hamman-Rich disease, pneumothorax, Mendelssohn syndrome, respiratory distress syndrome, pulmonary edema, chronic obstructive pulmonary diseases, acute pneumonia).
Hypercapnia can develop when forced to spend a long time in a closed room without ventilation.
Hypercapnia is most dangerous for newborns and children in the first months of life. It can cause the development of severe neurological disorders.
Why is hypercapnia dangerous?
Hypercapnia is an increased level of carbon dioxide in arterial blood and body tissues. Not many people are familiar with this term, but almost everyone has felt the state characterized by this word.
Remember what you experienced in large crowds of people - in queues, in stuffy offices. Or a condition during respiratory diseases, when the nose is stuffy and the bronchi are clogged with mucus. The head begins to feel dizzy or hurt, there is severe weakness, nausea, the heart beats faster, and sweat appears.
In the article about the benefits of carbon dioxide, we already touched on the concept of hypercapnia. Let's take a closer look at what this term means?
Carbon dioxide in our body can be both beneficial and harmful. It all depends on the amount of its content. There is a concept of balance, the norm for this indicator is 4.7-6%.
The normal mechanism for removing carbon dioxide from the human body is through the lungs, by penetrating from the blood vessels into the alveoli. If for some reason this process is disrupted, hypercapnia
– increase in carbon dioxide content.
Then the CO2 pressure in the gas mixture rises to 55–80 mm Hg, and the oxygen level decreases. Simply put, carbon dioxide poisoning occurs.
exogenous in nature
and
endogenous.
Exogenous develops with an increased content of carbon dioxide in the air. It arises, one might say, for external reasons beyond your control: queues, stuffy rooms.
And endogenous hypercapnia is caused by internal reasons:
- Impaired breathing mechanism due to weakness of skeletal muscles, chest injuries (compression, fractures), morbid obesity, scoliosis.
- Depression of the respiratory center (less frequent breathing) associated with damage to the central nervous system, the use of pharmaceuticals (anaesthetics, narcotic analgesics), circulatory arrest, etc.
- Gas exchange disorders: pulmonary edema, COPD (chronic obstructive pulmonary disease), pleurisy (inflammation of the lining of the lungs), pneumothorax (accumulation of air in the pleural cavity), etc.
An increase in CO2 may also be a consequence of its increased formation in the body itself. The cause may be fever, sepsis, polytrauma, malignant hyperthermia.
The form of hypercapnia can be mild, and a person will not particularly feel it. Having left the stuffy room, he will quickly forget about the sensations he experienced - slight dizziness, redness of the skin, rapid heartbeat and breathing.
The initial form of hypercapnia, especially if it “forms” gradually (over several days, even a month), is easier for the human body to cope with. Adaptation and compensation mechanisms are included.
With deep hypercapnia, the symptoms are more aggressive. Here deviations may appear from several body systems at once.
- From the nervous system: agitation appears, symptoms of increased intracranial pressure (nausea, headache, bruises under the eyes, swelling, etc.).
- From the cardiovascular system: blood pressure continues to rise, pulse reaches 150 beats/min., there is a risk of bleeding.
- From the respiratory system. Symptoms of acute respiratory failure increase: the rhythm of breathing is disrupted, it becomes shallow and rare, bronchosecretion increases, the skin tone is bluish, and sweating is severe.
The most severe degree of hypercapnia (it is also the most dangerous) is hypercapnic coma. A person in a coma has no reflexes and consciousness, blood pressure drops sharply, and the skin tone is cyanotic (cyanotic). The result may be respiratory and cardiac arrest, i.e. death.
Hypercapnia poses a very great danger to women during pregnancy. We may be talking about a miscarriage due to the development of respiratory failure, increased blood pressure and impaired placental gas exchange.
The second scenario is that a child may be born with a pathology (mental and psychomotor development delay, cerebral palsy, epilepsy, etc.). High levels of CO2 negatively affect the baby’s nervous system, which is not yet fully developed.
How to stabilize the condition of a person suffering from hypercapnia?
The amount of assistance to the victim depends, of course, on the degree of carbon dioxide poisoning. To stabilize a person’s condition and reduce the risks of complications, it is necessary, firstly, to ensure a sufficient flow of oxygen. This is the simplest and at the same time the most important action.
If a person is unable to leave the stuffy room himself, he needs to be taken out into the air. Most often, this is enough to eliminate mild hypercapnia of an exogenous nature.
With endogenous (internal) origin, we are talking about eliminating the underlying disease or mitigating the severity of its symptoms. Some patients are prescribed systematic cleaning of the airways, liquefaction and removal of viscous bronchial secretions.
A good effect is obtained by keeping the patient in a cool room with a humidity level of more than 50%. To improve lung ventilation, bronchodilators are used - a group of drugs that can relax the muscular wall of the bronchi and thereby increase their clearance, as well as respiratory stimulants. Thanks to these measures, the patient's condition normalizes.
In case of severe carbon dioxide poisoning, you cannot do it on your own; you will need medical help, sometimes emergency. Otherwise the person may die.
In especially severe cases, doctors perform tracheal intubation (insertion of a special tube for intensive care), oxygen therapy (the patient breathes a balanced oxygen-nitrogen mixture), and resort to artificial ventilation.
In case of endogenous hypercapnia, which appears due to internal disturbances in the functioning of the body, it is contraindicated to do breathing exercises or conduct classes on breathing simulators.
But despite this, it was important for us to talk about this phenomenon and its consequences in the blog. After all, we often talk about the benefits of carbon dioxide, so it would be simply dishonest to remain silent about its harm.
If your doctor has diagnosed you with hypercapnia or acidosis, under no circumstances should you start using breathing machines. This may make the situation worse.
If you do not have such a diagnosis, and the carbon dioxide content is below normal, then you can purchase a breathing simulator. At the same time, there is no need to be afraid that you will develop serious endogenous hypercapnia.
Firstly, the simulator cannot lead to such a result; it is aimed only at improving the health of the body. Secondly, you can always measure the level of carbon dioxide using a special camera that comes with the simulator.
Carefully monitor your health, listen to all the “signals” of your body and subscribe to our blog to recognize them in time.
You can learn more about the Samozdrav breathing simulator by clicking on the link.
Signs
Clinically, hypercapnia can manifest as a slow increase in symptoms over a long period of time, and sometimes develops at lightning speed.
Signs of hypercapnia:
- rapid breathing (tachypnea);
- feeling of lack of air;
- excitement, followed by depression of consciousness;
- marbling of the skin, which then turns into pronounced cyanosis;
- participation in the act of breathing of auxiliary muscles;
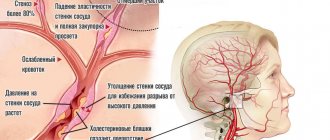
- increased blood pressure and tachycardia, which, as the condition worsens, are replaced by hypotension and bradycardia;
- increased sweating (hyperhidrosis);
- heart rhythm disturbances;
- headache, dizziness;
- decreased performance;
- convulsive seizures.
Symptoms of hypercapnia
Causes and symptoms of hypoxemia
Hypoxemia develops when arterial blood is not saturated with oxygen in the lungs. The level of oxygen in the blood is indicated by an indicator such as PaO2. Its normal level is 80 mm. Hg Art., but no less.
Causes of hypoxemia:
- Alveolar hypoventilation, which most often develops when there is insufficient oxygen in the air. However, other reasons can also lead to it.
- Disturbances in ventilation-perfusion connections, which is observed in various lung diseases.
- Right-to-left shunting occurs when venous blood enters the left atrium, bypassing the lungs. The cause of this condition is often one or another heart defect.
- Impaired diffusion in the alveolar-capillary membrane.
Causes of disruption of ventilation-perfusion connections in the lungs and the diffusion capacity of the alveolar-capillary membrane
Gas exchange in the lungs is ensured by ventilation of the lungs and blood flow in a small circle. But perfusion and ventilation occur in different proportions. Thus, some areas of the lungs are better ventilated, but are not supplied with blood. In some areas, on the contrary, blood is actively flowing, but there is no ventilation, for example, this is observed in the alveoli of the apexes of the lungs. If there are many such areas that take part in gas exchange, but are not sufficiently washed by blood, then this entails first hypoxemia and then hypercapnia. Such relationships are called ventilation-perfusion.
A violation of this ratio can be observed in the following cases:
- Pulmonary hypertension.
- Sudden loss of blood in large volumes.
- Shock of various origins.
- DIC syndrome with the formation of small blood clots in the bloodstream.
- Pulmonary embolism.
- Vasculitis.
The diffusion capacity of the alveolar-capillary membrane can increase and decrease, depending on specific circumstances. For example, what is the intensity of compensatory-adaptive mechanisms in a particular person during physical activity, when changing body position, etc. The diffusion capacity of the alveolar-capillary membrane begins to decrease in people after 20 years of age, which is the physiological norm for every person. Its significant decrease is observed in pathologies of the respiratory system, for example, with pneumonia, emphysema or obstructive pulmonary disease. All this becomes prerequisites for the development of hypoxemia, hypercapnia and hypoxia.
Signs of hypoxemia
Hypoxemia can increase quickly or gradually.
Its symptoms are:
- Cyanosis of the skin. The more intense it is, the lower the level of oxygen in the blood. If hypoxemia is weak, then cyanosis of the skin does not develop, the person simply looks paler than usual.
- Tachycardia or rapid heartbeat is a compensatory mechanism of the body, which tries to compensate for the lack of oxygen in this way.
- Falling blood pressure levels.
- Fainting, which develops when PaO2 decreases to 30 mm. Hg Art.
Insufficient oxygen content in the blood leads to the development of chronic fatigue syndrome, deterioration of memory and attention, sleep disturbance, night snoring, etc.
Features of hypercapnia in children
In children, hypercapnia develops much faster and is more severe than in adults. This is explained by the anatomical and physiological characteristics of the child’s body, such as:
- narrowness of the respiratory passages - accumulations of mucus and swelling of the mucous membrane against the background of even minor inflammation can lead to a violation of their free patency;
- underdevelopment and weakness of the respiratory muscles;
- the ribs extend from the sternum almost at a right angle, which limits the excursion (mobility) of the chest in the act of breathing.
Features of hypercapnia in pregnant women
In pregnant women, especially in the third trimester, any breathing disorders can cause rapidly developing hypercapnia, which is associated with the following features:
- oxygen consumption during pregnancy increases by 20-23%;
- the type of breathing changes to the chest, the abdominal muscles cease to play the role of auxiliary respiratory muscles;
- there is a high standing of the diaphragm caused by the growing uterus, which prevents deepening of inspiration when the need arises.
In late pregnancy, hypercapnia can develop rapidly
Diagnostics
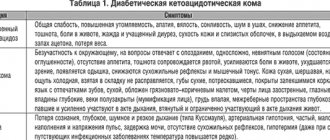
The primary diagnosis of hypercapnia is based on an analysis of the clinical picture. To confirm the diagnosis, as well as clarify the severity of respiratory failure, a study of the acid-base state of the blood is performed. Diagnostic signs of hypercapnia:
- increase in partial pressure of carbon dioxide - over 45 mm Hg. Art. (norm – 35–45 mm Hg);
- decrease in blood pH - less than 7.35 (normal - 7.35–7.45);
- an increase in bicarbonate content in the blood, which is compensatory in nature.
Hypercapnia can develop when forced to spend a long time in a closed room without ventilation.
The carbon dioxide content in exhaled air is also analyzed using a capnograph.
To diagnose hypercapnia, an acid-base state study is performed.
Pathogenesis of hypercapnia and hypoxemia
So, if the level of carbon dioxide in the blood is elevated, then a person is diagnosed with hypercapnia. When the oxygen level in the blood decreases, they speak of hypoxemia.
Oxygen, which enters the lungs along with the inhaled air, is carried through the bloodstream throughout the body using red blood cells, binding to hemoglobin. Hemoglobin, which carries oxygen to tissues, is called oxyhemoglobin. When it reaches its destination, oxyhemoglobin gives up oxygen, after which it becomes deoxyhemoglobin, which can again attach oxygen, or carbon dioxide, or water. However, normally, in the tissues where hemoglobin has delivered oxygen, carbon dioxide is already waiting for it. It picks it up and removes it from the tissues to the lungs, which, during exhalation, rid the body of carbon dioxide. Hemoglobin, which carries carbon dioxide, is called carbohemoglobin.
If we consider this process in the form of a diagram, it will look like this:
- Hb found in red blood cells + O2 from the air = HbO2 (this reaction occurs in the lungs, from which oxygenated hemoglobin is sent to the tissues).
- HbO2> Hb + O2, while oxyhemoglobin gives oxygen to tissues.
- Hb + CO2 (deoxyhemoglobin takes carbon dioxide from the tissues) = HbCO2 (this carohemoglobin is sent back to the lungs to get rid of carbon dioxide).
- HbCO2 from tissues breaks down in the lungs into Hb and CO2. In this case, CO2 is removed, and Hb takes a new O2 molecule to again deliver oxygen to the tissues.
- The cycle repeats again.
In this formula:
- Hb – hemoglobin.
- HbO2 is unstable oxyhemoglobin.
- O2 – oxygen.
- CO2 – carbon dioxide.
- HbO2 is an unstable carbohemoglobin.
This reaction of the exchange of oxygen and carbon dioxide occurs provided that a person inhales clean air, in this case, the tissues do not experience oxygen starvation. However, it is known that reduced hemoglobin can attach any molecule to itself, since it does not have strong bonds. In simple terms, he attaches any component that comes his way. If there are few oxygen molecules in the lungs, then hemoglobin will take carbon dioxide molecules and send them to the tissues along with arterial blood. As a result, a person develops hypoxia, that is, oxygen starvation.
Hypoxia, hypoxemia and hypercapnia are three symptoms that are characteristic of acute respiratory failure.
Treatment
Therapy for hypercapnia is aimed at eliminating the cause that caused it.
If symptoms of hypercapnia appear after staying in a stuffy room, it is enough to go outside or ventilate the room: this quickly leads to an improvement in the patient’s condition.
Treatment of hypercapnia against the background of inflammatory diseases of the respiratory system requires the prescription of antibacterial agents, bronchodilators, and anti-inflammatory drugs.
In case of hypercapnia caused by an overdose of narcotic analgesics, the administration of a specific antidote, Nalorphine, is indicated.
Sometimes, to get rid of the symptoms of hypercapnia, it is enough to ventilate the room
In acute hypercapnia, the patient is given humidified oxygen to breathe through nasal catheters or a face mask. In the case of a severe general condition of the patient, the issue of intubation and transfer to artificial ventilation is resolved.
Causes of oxygen starvation of the body
Many factors can provoke hypoxia.
However, depending on the nature of its origin, two types of hypoxic reactions are distinguished:
- Exogenous hypoxia. In this case, hypoxia develops as a result of the fact that the level of oxygen in the inhaled air becomes low. Therefore, human blood is not saturated with O2, which leads to oxygen starvation of tissues. Exogenous hypoxia develops in people who fly at high altitudes, rock climbers, mountain climbers, and scuba divers. Also, exogenous hypoxia develops in any person who inhales air with harmful inclusions.
- Hypoxia, which develops against the background of various pathologies of the respiratory organs or circulatory system.
This hypoxia is divided into 4 subtypes:
- Respiratory hypoxia, which manifests itself when the function of external respiration is impaired. At the same time, the actual volume of ventilation of the alveoli per unit of time is lower than the body needs. Respiratory hypoxia is caused by chest injuries, obstruction of the airways, a decrease in the working surface of the lung tissue, and suppression of the respiratory center (while taking medications, with pulmonary edema, with inflammation of the lung tissue). Respiratory hypoxia can be a consequence of diseases such as pneumonia, emphysema, pneumosclerosis, chronic obstructive pulmonary disease. It can also develop against the background of poisoning of the body with toxic substances.
- A circulatory form of hypoxia, which develops against the background of acute or chronic failure of the circulatory system. Congenital heart defects, such as a patent foramen ovale, can lead to such disorders.
- Tissue hypoxia develops during poisoning. In this case, the tissues simply refuse to accept the oxygen supplied by the blood.
- Blood hypoxia, which develops against the background of a drop in the level of red blood cells or hemoglobin in the blood. The most common cause is anemia, which is a consequence of acute blood loss or other pathological conditions.
Severe hypoxia is indicated by symptoms such as cyanosis of the skin, tachycardia, drop in blood pressure, convulsions, and fainting. With severe hypoxia, the patient's symptoms of heart failure quickly increase. If the victim is not given emergency assistance, he will die.