What's happened
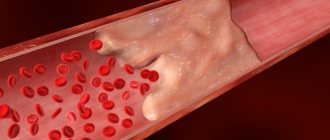
First, it’s worth understanding what a carotid artery is: in the human body there are two carotid arteries, running from the chest through the sides of the neck to the head. Their main task is to nourish the brain. Like any artery, they are confirmed by atherosclerosis - a serious disease, the nature of which is not fully understood, as well as the causes. This disease manifests itself in the deformation of the walls of blood vessels, when the tissues lining the vessel grow, cholesterol deposits appear between them, and the lumen of the vessel becomes smaller and smaller until it becomes completely blocked (obstruction). Oxygen-enriched blood flows through the carotid arteries for brain cells, so narrowing the lumen of the vessel is very dangerous - it can cause a stroke.
4.Treatment
With confirmed dissection of the carotid artery, long-term treatment with anticoagulants and antiplatelet agents is prescribed as a measure to prevent thrombus formation. In most cases, it is also indicated and advisable to prescribe drugs that stimulate trophism and strengthen vascular walls.
Precautions and necessary restrictions in terms of physical activity must be explained: in approximately 10% of cases, a relapse of RSA occurs within a year.
Despite this, the prognosis is generally favorable. Timely request for help and qualified provision of it allows you to completely restore the patency of the artery and the associated brain functions in approximately half of the patients; in other cases, as a rule, it is possible to achieve significant and lasting improvement.
Causes and prevention
The causes of vasoconstriction are being actively studied, but there is still no clear understanding. A hereditary cause is identified, and everything else can be attributed to risk factors. Among them:
- arterial injuries,
- obesity,
- smoking,
- diabetes,
- sedentary lifestyle,
- older age,
- high level of “bad cholesterol” in the blood (low-density lipoproteins are a combination of cholesterol and protein that do not take excess cholesterol from the vessels, but, on the contrary, attach them to the walls, forming cholesterol plaques).
Prevention of carotid artery stenosis, like any other arteries, consists of maintaining a healthy active lifestyle and a balanced diet to prevent an imbalance in the ratio of low- and high-density lipoproteins, and therefore the development of atherosclerosis.
Stenoses in oncology
Malignant tumors often block the lumen of hollow organs, disrupting their functions. In this case, the patient’s condition always worsens significantly, and the prognosis becomes more serious. If radical surgery for a malignant neoplasm is not possible, then the doctor performs palliative surgery to eliminate stenosis, restore organ function, and improve the patient’s condition.
The patient's condition improves when the tumor begins to disintegrate - it no longer blocks the lumen of the organ. The tumor disintegrates under the influence of chemotherapy, less often on its own. Substances that are released into the blood during massive decay of tumor cells poison the body and can lead to serious complications.
Symptoms of carotid artery stenosis
The disease is dangerous because the symptoms are practically invisible, and only when stenosis becomes the cause of other pathological conditions does a person consult a doctor. Among such conditions, ischemic attacks (mini-stroke, small stroke) are primarily distinguished, when the blood supply to the brain is disrupted for a short period of time. This condition manifests itself as follows:
- numbness of hands/arms,
- speech distortion,
- temporary loss of vision, visual acuity,
- temporary disorientation,
- numbness of the face.
And more general symptoms
- headache,
- nausea,
- weakness.
Carotid artery stenosis develops slowly, often asymptomatically, and people attribute general fatigue and increased fatigue to excessive stress or the weather. Therefore, doctors recommend carefully monitoring your condition, and, if you experience prolonged general weakness without obvious reasons, contact a specialist. Some diseases are so dangerous if not diagnosed promptly that the risk of their presence justifies an unplanned trip to the doctor, who will reassure you if there is no cause for concern, or carry out the necessary diagnostics if suspicions arise.
In which organs can stenosis occur?
Stenosis can occur in any organs that have a lumen, in the heart and in vessels of different diameters, in various anatomical canals. Symptoms of stenosis are very diverse - they depend on the affected organ and impaired functions.
Common types of stenoses:
- Stenoses of the digestive system organs: esophagus, stomach, intestines, bile ducts, pancreatic duct, papilla of Vater (the place where the bile duct and pancreatic duct enter the duodenum).
- Stenosis of the respiratory tract: larynx, trachea, bronchi.
- Stenoses of organs of the cardiovascular system: heart valves, aorta, arteries and veins of different diameters.
- Stenoses of the urinary system organs: ureters, urethra, bladder neck, renal arteries.
- Spinal stenosis. Frequent causes are previous spinal injuries, osteophytes, tumors, herniated intervertebral discs.
- Stenoses in the nervous system: the most striking example is non-communicating hydrocephalus; Among the causes may be tumor processes in the brain and spinal cord.
Book a consultation around the clock +7+7+78
Diagnostics
Diagnosing a narrowed blood vessel may require one or more types of tests because the location of the narrowing is not always easy to find. For this purpose, our center uses:
- ultrasound - as the main method - since modern equipment provides maximum information not only about the presence of stenosis, but also the degree of deformation of the vessel, while being a non-invasive safe diagnostic method;
- MRI or CT;
- angiography - thanks to the introduction of a contrast agent, a complex diagnostic device monitors blood flow throughout the body, noting even minor deviations from the norm).
To diagnose atherosclerosis (which is the cause of narrowing), a laboratory method is also used - a blood test.
Diagnostic program for the disease
First of all, a timely start to the diagnostic search is necessary. It is better to rule out the disease and continue to live peacefully than to postpone a visit to the doctor “for later.” For symptoms that cause concern, professional medical attention is necessary. The doctor begins making a diagnosis by interviewing the patient and general clinical examinations. If there are neurological symptoms, reflexes, sensitivity, motor activity, muscle and analyzer function are assessed. The following instrumental methods are used:
- Ultrasound of the arteries of the head and neck with Doppler sonography - triplex scanning. A safe, fast and inexpensive method that allows you to exclude or confirm the diagnosis;
- Functional tests during ultrasound examination;
- Computed tomography angiography - visualization of blood flow through vessels using a contrast agent;
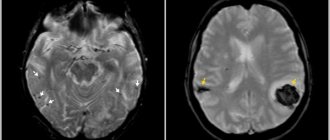
- Magnetic resonance imaging of the brain.
To diagnose atherosclerosis, a laboratory method is used - the patient donates blood for a lipid profile. Also, it is necessary to evaluate the blood coagulation system and its coagulation properties. It is mandatory to measure pulse and blood pressure. To identify systemic vasculitis, specific laboratory tests and immunological studies are used.
MRI and CT are the “gold standard” in the diagnosis of ischemic disorders, including stroke. Depending on the location and extent of the lesion, treatment is prescribed.
Treatment of carotid artery stenosis
The most common treatment for stenosis is artery stenting. Stenting is a surgical treatment method, therefore, like any other surgical intervention, it requires a highly qualified doctor in diagnosis, deciding on the need/possibility of surgery and direct insertion of the stent. A stent is a metal frame inserted directly into an artery. At the point of narrowing, it unfolds and expands the walls of the vessel as necessary. The stent remains in the artery. Only in the first days its presence can be inconvenient due to changes in blood flow, but over time the patient stops feeling it and returns to normal life without the risk of a stroke. But of course, the doctor will give certain recommendations for further lifestyle in order to prevent re-stenosis.
Our doctors understand the importance of high-quality patient management and postoperative monitoring, so by contacting us, you can count on an integrated approach to diagnosis, treatment and the postoperative period. To implement this approach, the neurology department of the Federal Scientific Research Center has a powerful diagnostic base and a strong team of specialists with extensive experience in the treatment of stenosis, who additionally undergo advanced training courses on a regular basis. The department closely cooperates with the cardiac surgery service and the department of vascular surgery, which is separated into a separate unit.
The advantage of our center is the provision of a full range of services to our patients in one place, starting with an initial consultation, which you can sign up for by phone or through a special form on the website.
Causes of the pathological condition
There are many reasons for the development of arterial occlusion. The most common is atherosclerosis. This disease is characterized by the formation of a plaque-growth on the inner side of the vascular wall. The object consists of a cholesterol substrate, fat cells, blood cells - platelets. Plaque growth occurs at a slow pace. As it grows, the internal vascular lumen decreases. The growth itself becomes the basis for the formation of a blood clot. With the blood flow, the thrombus can move into narrower sections of the canal and block the arterial lumen. If the plaque has resulted in only a partial occlusion of the bloodstream, the flow may cause the plaque itself to rupture. This also results in overlapping of narrower areas.
Other diseases of the vascular system and heart that contribute to thrombosis of the bloodstream also lead to narrowing or blocking of the ducts. The root cause of the abnormal condition can be a bacterial infection that develops in the heart muscle, internal parts, and valves. Often, congenital disorders, acquired defects, and tumor formations of various nature play a decisive role. Anatomical tortuosity and confused configuration of the vascular network become the basis for the risk of formation of wall closure. External injuries to intracranial structures, such as traumatic brain injuries of varying severity, can also lead to abnormal degeneration of the CC network.
Associated unfavorable factors are:
- bad habits (smoking, alcoholism);
- diabetic syndrome;
- constant consumption of “heavy” foods with a high concentration of animal fats;
- excess weight gain.
Forecast
Without treatment, atherosclerotic occlusion of the subclavian artery leads to a gradual decrease in working capacity, and the likelihood of ischemic stroke and gangrene of the hand increases.
After restoring blood circulation by any method, the problem is completely eliminated. Normal blood flow promotes normal hand function and eliminates brain steal syndrome.
Relapses after stenting of the subclavian artery occur in approximately 10% of cases, due to the development of new plaques inside the stent (restenosis). If a carotid-subclavian bypass operation was performed, then the probability of relapse is no more than 2% of cases.
Course of the disease
Atherosclerotic occlusion gradually leads to worsening symptoms of chronic arterial insufficiency of the arm. Gradual muscle atrophy occurs, and cerebrovascular accidents may develop.
In general, subclavian artery occlusion poses little threat to life expectancy, but has a serious impact on quality of life, so treatment is indicated when symptoms are present.
The disease can be divided into several stages:
I (compensation). Occasionally, the patient complains of increased sensitivity to cold, a feeling of numbness, and weakness during physical activity.
II (partial compensation). "Intermittent claudication of the arm." It is characterized by symptoms of blood flow insufficiency - weakness, pain, numbness, coldness in the fingers, hand, and forearm muscles during physical activity. Transient disturbances of cerebral circulation are possible.
III – (decompensation). Permanent arterial insufficiency of the arm. The patient complains of constant numbness of the arm, a decrease in the volume of the shoulder and forearm compared to the other side, a decrease in muscle strength, and the inability to perform fine movements with the fingers.
IV – (trophic ulcers and gangrene). There appears cyanosis of the hand, swelling of the phalanges, cracks, trophic ulcers, necrosis and gangrene of the fingers.
Fortunately, such extreme manifestations are quite rare.
Complications
The most common complication is the phenomenon of vertebral-subclavian steal (steal syndrome). To compensate for blood circulation in the arm, cerebral blood flow is used, which moves in the opposite direction from the brain to the arm through the vertebral artery. In this case, physical work with the hand can cause disruption of cerebral circulation, including loss of consciousness.
Occasionally, atheroembolic complications may occur. Pieces of atherosclerotic plaque may be carried downstream into the arm. This is manifested by a sharp deterioration in blood circulation in the hand, blueness and pain in the fingers. If help is not given in a timely manner, necrosis of the finger may develop, which will require its amputation.