Treatment of blood clots in the arteries of the brain
It is necessary to immediately begin a set of therapeutic measures.
Medication
Drugs that directly affect the rheological properties of blood:
- Anticoagulants - have an effect on the coagulation process, inhibiting the adhesion of platelets to each other and preventing small clots from forming one large one. Clopidogrel, indobufen, ditazol, ticlopidine;
- Thrombolytics – used for moderate and higher degrees of thrombosis: they dissolve the clot and initiate fibrinolysis. Streptokinase, tenecteplase;
- Antiplatelet agents – suppress blood clotting, reduce thrombus formation. Warfarin, heparin, dicoumarin, hirudin and drugs from other medicinal groups. Aspirin (acetylsalicylic acid) is the most popular of these.
Drugs acting on the walls of the vessel:
- Vasodilators;
- Antihypertensives – reduce blood pressure;
- Pentoxifylline derivatives enhance microcirculation in brain tissue.
- Nootropics are medications that stimulate metabolism in nervous tissue, increase resistance to oxygen deficiency, and help improve intellectual abilities and memory.
Surgical
To prevent a stroke, the following can be done:
- Carotid endarterectomy – removal of blood clots and atherosclerotic plaques on the carotid artery when 70% stenosis is detected and in patients who have suffered a transient ischemic attack (TIA). Surgery is often used to prevent future strokes.
- Stenting and angioplasty is an expansion of the diameter of narrowed sections of arteries, with atherosclerotic changes in those that are located in hard-to-reach areas. A balloon is inserted into the narrowing areas, which, when inflated, increases the diameter of the vessel. A mesh element, a stent, is placed in the artery to prevent the narrowing of the vessel. Allows you to avoid dangerous consequences such as stroke and ischemic attack.
Risk factors
- smoking (the most dangerous factor);
- hyperlipoproteinemia (total cholesterol > 5 mmol/l, LDL > 3 mmol/l, Lp(a) > 50 mg/dl);
- arterial hypertension (high blood pressure) (systolic blood pressure > 140 mm Hg; diastolic blood pressure > 90 mm Hg);
- diabetes;
- obesity;
- physical inactivity (sedentary lifestyle).
Without correction of risk factors, in the presence of a predisposition to atherosclerosis, cholesterol deposits gradually increase in the walls of the arteries. For clinical manifestations of atherosclerosis, a narrowing of any large artery by more than 50% is necessary. It is at this stage that patients most often seek medical help. Plaques in the carotid arteries are most often located in the cervical segment of the artery, over a short distance. The key point in determining the severity of damage to the internal carotid artery is the percentage of narrowing (stenosis) of its lumen, in relation to the normal lumen located behind the plaque. Numerous studies have proven that stenosis of the internal carotid artery by more than 70% increases the risk of ischemic stroke by 5 times, compared with a lesser degree of stenosis. The brain receives its main blood supply from two internal carotid and two vertebral arteries. Stenosis of the artery by more than 70% leads to a change in the local parameters of the blood flow - they can be compared with the flow of river water in places where the channel narrows - seething, turbulence, chaotic impacts of blood into the vessel wall lead to microthrombosis, trauma to the vessel wall, destruction of unstable plaques and its detachment particles. Particles of plaques and blood clots freely located in the bloodstream are called emboli. Following the bloodstream, the embolus gets stuck in smaller branches located in the brain, causing ischemia of areas of the brain and leading to its death.
Symptoms of atherosclerotic plaques in the carotid artery
The presence of atherosclerotic plaques in the vessels supplying the brain is often difficult to suspect, because complaints are varied and inconsistent. In addition, for clear symptoms to appear, there must be pronounced narrowing of the arteries. It is necessary to suspect the presence of atherosclerosis of the carotid arteries in the presence of risk factors, as well as diseases of the heart and blood vessels of the lower extremities. Currently, the main symptoms are considered to be the presence of small and large ischemic strokes, as well as general cerebral symptoms.
- Transient ischemic attacks (TIA)
occur when small fragments of an atherosclerotic plaque break off and enter small vessels of the brain, causing brain death in a small area. In this case, transient paralysis of the arms and/or legs (from several minutes to several hours), speech impairment, transient or sudden blindness in one eye, memory loss, dizziness, and fainting are possible. The presence of a TIA is a serious sign of a high risk of developing a severe stroke in the near future and requires immediate medical attention.
- Acute ischemic cerebrovascular accident (ACVA)
– a consequence of acute blockage of a large branch of the internal carotid artery, which led to the death of neurons and loss of some functions in the brain. In a third of all cases, a stroke leads to death. In most all cases, severe disability after a stroke forever changes the life of a person and his relatives.
- Chronic cerebrovascular insufficiency
– a decrease in blood flow to the brain due to narrowing of the arteries, forcing brain cells to be in constant tension of all intracellular systems and intercellular connections. Symptoms are non-specific, they can be noise in the head, dizziness, flashing “spots” before the eyes, unsteadiness when walking, etc.
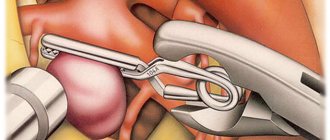
Surgery to remove plaque from the internal carotid artery (eversion carotid endarterectomy)
Unfortunately, there are no drugs yet that can “dissolve” or eliminate plaques in blood vessels. Modern drugs can only stop the growth of atherosclerotic plaques and reduce the likelihood of blood clots. The main and only effective treatment for narrowing of the arteries is surgery. Numerous studies involving many countries have indisputably proven the effectiveness of preventive surgical methods in preventing stroke. It is important to understand that surgical intervention is performed if there are strict indications for surgery, and does not replace the treatment of systemic atherosclerosis.
One of the ways to eliminate stenosis of the internal carotid artery is the operation of eversion carotid endarterectomy.
- Under the safest anesthesia (usually a local anesthetic), a small incision (4-6 cm) is made in the neck in the area of the carotid artery.
- Under threefold magnification, with the help of special instruments, the arteries are separated from the surrounding structures (nerves, veins).
- The resistance of the brain to temporary compression of the carotid artery is checked using several techniques. If there is the slightest suspicion that the brain will not be able to withstand clamping of the carotid artery, a special temporary shunt is installed to ensure blood supply to the area of the operated artery. The arteries are pinched.
- The internal carotid artery is dissected transversely and the outer layer of the artery is everted from the plaque like removing a stocking from a leg, after which the atherosclerotic plaque is removed from the vessel along with the inner layer.
- All plaque remnants freely lying in the lumen of the vessel are carefully removed and the outer layer of the artery is returned to its previous position.
- The integrity of the vessel is restored with a continuous suture. The threads used for sutures are thinner than 1/10 mm and are non-absorbable.
- Once the suture is completed, air is released from the artery and blood flow is restored. After checking the sutures for tightness and the absence of sources of bleeding, the wound is sutured layer-by-layer with a cosmetic suture.
Throughout the operation, the patient remains conscious, and verbal and eye contact is always maintained. The duration of the entire operation is 1-2 hours; in the postoperative period, long-term observation and treatment in the intensive care unit is not required. The perioperative protocol at our institution allows patients to be discharged the next day after surgery, which has a beneficial effect on early rehabilitation and prevents the occurrence of infectious complications.
What is carotid artery thrombosis?
Carotid artery thrombosis is a pathology that is extremely dangerous for humans. The fact is that the carotid artery extends from the thoracic artery and directs blood flow directly to all parts of the brain. That is, it is its main blood supply vessel. Therefore, if a clot (embolus) is localized in the carotid artery, then over time it risks breaking off and reaching the brain in the shortest possible time. And this is sudden and inevitable death.
It is the carotid artery that is most prone to the deposition of lipids on its walls. As a result, atherosclerosis develops - the deposition of cholesterol plaques that impede blood flow. Later, platelets adhere to the lipids and plaques, which forms a blood clot. Its growth over time can lead to complete blockage of the vessel. The disease code according to ICD-10 is I70–I79.
Diagnosis of carotid artery stenosis
To determine whether you have stenotic lesions of the carotid arteries or not, your doctor will examine you.
Even if you have no symptoms, your doctor may hear a murmur over your carotid arteries caused by blood flowing through the stenotic area.
If necessary, you will be prescribed Doppler ultrasound of the main arteries of the head (USDG MAG), electroencephalography of the brain (EEG) or computed tomography (CT).
For a more detailed assessment of the condition of the carotid arteries, your doctor may recommend an angiography (x-ray examination of blood vessels).
This study is performed by catheterization, usually of the femoral artery, under local anesthesia in a special operating room equipped with an angiography unit.
After the examination, the doctor will determine the presence of a lesion and choose the optimal treatment method for you.
Forecast
The prognosis for treatment of thrombosis depends on the following factors:
- Where is the carotid artery located and what is its role in the human circulatory system?
- competently prescribed therapy and the patient’s adherence to the doctor’s recommendations, lack of self-medication and ignoring symptoms;
- how quickly medical care was provided after a blood clot formed;
- the presence of concomitant diseases, including those associated with blood vessels (especially cerebral);
- patient's age;
- the degree of severity and nature of changes in brain tissue caused by deterioration of blood supply due to thrombosis (if any).
The timeliness and correctness of medical care is very important.
Examinations before surgery
To select the surgical method (open or endovascular), the patient undergoes examination of the vessels of the head and neck - ultrasound.
In some cases, additional CT, MRI or angiography is required. In addition to examining the blood vessels before surgery, it is necessary to assess the state of health in general; for this, a number of standard examinations are prescribed, as for any other operation: clinical and biochemical blood tests, urine tests, tests for hepatitis, HIV, syphilis, etc., fluorography, ECHO CG (ultrasound of the heart), consultation with a therapist and/or cardiologist. The doctor must have a complete understanding of the patient’s health status, so additional examinations are prescribed if necessary.
One of the features of the examination before vascular surgery is the mandatory EGDS (examination of the stomach). The fact is that during and after the operation the patient is prescribed antithrombotic drugs that “thin” the blood; therefore, if the patient has a stomach ulcer, bleeding from the ulcer can occur. To diagnose an ulcer, an endoscopy is performed.
After a complete examination, the surgical method is selected depending on the characteristics of vascular damage, concomitant diseases and other factors.
Causes of blood clot formation
Most often, the triggering factor for the process is atherosclerosis. This artery is one of the large vessels most susceptible to the accumulation of cholesterol and calcium formations, often leading to severe narrowing of the artery lumen.
At the same time, blood flow is hampered, which leads to a significant deterioration in the blood supply to brain tissue. Plaques deform and injure the walls of blood vessels, creating conditions for blood cells to settle in the thickness of the damaged walls.
A blood clot often occurs when clumps of platelets (a type of blood cell responsible for clotting) adhere to lipid deposits.
Such formations are relatively inert, but they interfere with normal blood flow and can completely block the lumen. The symptoms of the condition greatly depend on where the blood clot has formed.
If a blood clot grows quickly, it can cause a cerebral infarction, or ischemic stroke. If the process develops slowly, you can reduce the risk of developing life-threatening conditions if you consult a doctor in a timely manner.
Factors that increase the likelihood of thrombosis are:
- heart disease, in particular ischemia, atrial fibrillation;
- heart valve defects;
- vasculitis, including Horton's syndrome;
- malignant or benign tumors;
- circulatory disorders, tendency to blood stagnation;
- alcoholism;
- diabetes mellitus (it is well known that patients with this disease have increased blood density, which reduces the speed of blood circulation);
- traumatic brain injuries;
- the patient is overweight;
- stenosis of certain vessels (especially if the lumen between the walls narrows by half or more);
- vascular spasms due to stress;
- a history of blood clots, especially in the vessels of the heart, pulmonary and subclavian arteries;
- individual anatomical features of the artery;
- problems with blood clotting, as well as (in combination with other factors) taking drugs that increase clotting.
In most cases, pathology is detected in elderly men. But in some cases, thrombosis can be detected in young people, which is often associated with head injuries or hematomas of the vessel walls.
- Cholesterol plaques in the carotid artery and vessels of the neck
Depending on which part of the artery is affected by the disease, thrombosis of the internal carotid artery and the external one are distinguished.
Syndromes of thrombosis of the anterior artery of the choroid plexus
The anterior artery of the choroid plexus of the brain begins from the internal carotid artery and supplies blood to the posterior thigh of the internal capsule, as well as the white matter of the brain to the side and behind it, through which part of the optic fibers passes from the lateral geniculate body to the calcarine groove. This area of the brain is also supplied with blood by:
- penetrating vessels coming from the trunk of the middle cerebral artery (arteries of the lenticular nucleus and striatum)
- penetrating branches of the posterior communicating artery
- posterior choroid plexus artery
Therefore, the full clinical syndrome in the form of contralateral hemiplegia (paralysis of the muscles of the body on the opposite side), hemianesthesia (hypoesthesia) and homonymous hemianopsia (loss of half the visual field on the side of the brain lesion) may not develop. Instead, syndromes with minimal severity of neurological focal disorders are observed.
Indeed, in cases of surgical occlusion of the anterior artery of the choroid plexus for the purpose of treating the symptoms of Parkinson's disease, some patients do not show signs of circulatory deficiency in the area of its basin. Patients who initially presented with advanced clinical symptoms often recover fully or partially, apparently due to sufficient levels of collateral arterial blood flow in this part of the brain.
Clinical picture
Common complaints:
- persistent or persistent increasing headaches;
- impaired sensitivity and motor skills of the muscles of the face, arms and legs, right or left half of the body;
- persistent distortion of speech and its understanding;
- blurred vision;
- loss of body balance, dizziness;
- feverish condition;
- excessive sweating;
- blood pressure surges;
- uncontrolled acts of defecation and urination;
- loss of consciousness;
- convulsive contractions, muscle twitching;
- nausea, vomiting.
Thrombosis of the basilar artery
Complaints regarding thrombosis of the basilar artery supplying the brain stem:
- throbbing occipital pain;
- dizziness, patients are “stormy, rocking on the waves”;
- blurry visual perception;
- impaired sensitivity of the skin around the mouth;
- gaze paresis – the inability to move both eyes simultaneously in vertical or horizontal directions;
- impaired sensitivity of half of the face;
- fainting;
- noise in ears.
Thrombosis of the carotid artery (internal, external)
Complaints characteristic of deterioration of blood supply to the brain through the internal carotid arteries :
- serious weakening of visual perception, even blindness;
- inability to speak, speech confusion;
- deterioration of motor function of the upper extremities;
- tremor;
- fainting;
- paresis of one or both halves of the body.
Complaints characteristic of deterioration of blood supply to the cerebral cortex, tissues of the neck and face through the external carotid arteries :
- dry mucous membranes;
- neck pain;
- distortion of facial expressions, paralysis of facial muscles;
- fainting;
- slurred speech;
- constant pain in the head.
Anterior cerebral artery thrombosis syndromes
The anterior cerebral artery of the brain has two segments:
- precommunal (A1) segment of the circle of Willis, or stem, segment that connects the internal carotid artery with the anterior communicating artery
- postcommunal (A2) segment, originating from the connection of the A1 segment with the anterior communicating artery
Segment A2 of the anterior cerebral artery, through its cortical branches, supplies blood to the anterior 2/3 of the medial surface of the orbital part of the frontal lobe, the pole of the frontal lobe, the strip of cortex along the superomedian border and the anterior 2/3 of the corpus callosum. On the other hand, the A1 segment of the anterior cerebral artery gives off many deep penetrating branches, going mainly to the anterior femur of the internal capsule, the anterior perforated substance, the amygdala, the anterior hypothalamus and the lower part of the head of the caudate nucleus of the brain.
Cerebral infarctions (strokes) in the anterior cerebral artery territory are rare. Blockage (occlusion) of the trunk or segment of the A1 anterior cerebral artery is usually well compensated due to the possibility of collateral blood flow from the opposite side. The most severe disorders occur in cases where both anterior cerebral arteries originate from a single trunk (in the case of a congenital anatomical feature of its structure in the patient), blockage (occlusion) of which leads to the occurrence of an extensive infarction in the anterior cerebral arteries of both hemispheres of the brain.
Clinical manifestations of blockage (occlusion) in the basin of both anterior cerebral arteries include bilateral pyramidal disorders with paraplegia (paralysis of the muscles of the left and right half of the body) and pronounced changes in the psyche due to bilateral damage to the frontal lobes of the brain.
Components of a typical syndrome that develops when the anterior cerebral artery is blocked:
Clinical manifestations | Affected brain structures |
| Contralateral foot and leg paralysis | Motor projection of the leg |
| Less severe contralateral arm paresis | Involvement of the area of the cortical projection of the hand and the fibers coming from it in the corona radiata |
| Cortical lesion leading to loss of sensation in the toes, foot, and leg | Sensory projection of the foot and leg |
| Urinary incontinence | Sensorimotor area of the paracentral lobule |
| Contralateral grasping and sucking reflexes, paratonic rigidity | Inner surface of the posterior part of the frontal lobe - supplementary motor area |
| Abulia (akinetic mutism), slowness, retardation, periodic sudden hesitations, spontaneity, whispered speech, motor inactivity, reflex animation when exposed to visual and sound stimuli | Localization is unclear - probably the cingulate gyrus and the medial parts of the parietal and temporal lobes |
| Impaired walking and standing (gait apraxia) | Frontal cortex near the motor projection of the leg |
| Dyspraxia in the left limbs, left-sided tactile aphasia | Corpus callosum |