Lev Manvelov, Candidate of Medical Sciences
, Albert Kadykov,
Doctor of Medical Sciences
“Science and Life” No. 2, 2007
General diagram of the blood supply to the brain.
Blood enters the brain through four large main arteries: two internal carotid and two vertebral. At the base of the brain stem, the vertebral arteries merge into one, the basilar artery. In the brain, the internal carotid artery divides into two main branches: the anterior cerebral artery, which supplies blood to the anterior parts of the frontal lobes, and the middle cerebral artery, which supplies parts of the frontal, temporal and parietal lobes. The vertebral and basilar arteries supply blood to the brain stem and cerebellum, and the posterior cerebral arteries supply the occipital lobes of the brain (image: Science and Life)
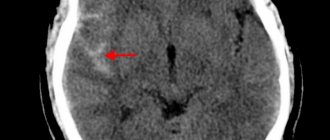
Headache, noise and dizziness, memory impairment, increased fatigue, decreased performance - such symptoms occur not only in the elderly, but also in middle-aged and even young people. Often, patients and some medical professionals do not take such complaints very seriously. Meanwhile, they may indicate chronic cerebral circulatory failure.
Causes of cerebral vasospasm
Angiospasm often occurs due to:
- overwork;
- nervous or physical stress;
- sedentary lifestyle (for example, prolonged sitting at the computer);
- stress and strong emotions, even positive ones;
- lack of sleep;
- lack of oxygen in the room;
- abuse of coffee and strong tea;
- vitamin deficiency;
- smoking;
- excessive alcohol consumption;
- hypothermia;
- atmospheric pressure fluctuations;
- age-related changes in the arteries.
Spasm of cerebral vessels can be a symptom of osteochondrosis of the cervical spine, arterial hypertension, cerebral aneurysm, tumor formation, vegetative-vascular dystonia, and thyroid diseases.
The risk group includes elderly people and people sensitive to weather changes, smokers, abuse alcohol, often drink strong tea/coffee, suffer from insomnia, hypertension, angina pectoris, diabetes mellitus or dyscirculatory encephalopathy, and have a family history of stroke or myocardial infarction .
Treatment of VSD at the Yusupov Hospital
Before starting treatment for vegetative-vascular dystonia, the Yusupov Hospital carries out a comprehensive diagnosis to identify the causes of this disorder. High accuracy of results is achieved through the use of modern European equipment. After receiving the examination results, experienced specialists select the necessary treatment for patients to help relieve spasms during VSD and other manifestations.
At the Yusupov Hospital, medical staff and staff treat each patient with care, so treatment for VSD is not only effective, but also comfortable. An equally important advantage of the Yusupov Hospital is the modern provision of each of the clinics of the multidisciplinary hospital.
By visiting the clinic for the treatment of VSD, patients can receive a variety of services that meet international medical standards. If you need a consultation with a highly qualified neurologist, visit the Yusupov Hospital at a time convenient for you.
Signs of cerebral vasospasm
The main symptom of the pathological process is headache of varying localization and intensity. It usually occurs in the temples and forehead, sometimes felt all over the head.
You may also experience:
- dizziness;
- pain in the eyes, ear, neck;
- noise in ears;
- “flies” before the eyes;
- darkening of the eyes;
- nausea;
- changes in blood pressure;
- feeling tired;
- numbness of lips;
- tingling in temples.
If a spasm is a precursor to a stroke or rupture of an aneurysm, disturbances in speech, sense of orientation in space and coordination of movements, and loss of consciousness are possible.
Muscle spasms during VSD
Back or muscle pain often occurs in patients diagnosed with VSD. The cause of these symptoms is muscle spasms caused by malfunctions of the nervous system. Painful sensations become most intense in the evening, they do not allow a person to fall asleep. Muscle spasms are associated with increased fatigue, so in some cases they may appear during the day.
Tense muscles and blood vessels during VSD require strengthening and relaxation. With strong nervous tension, it is difficult for the patient to control his own movements, so moving the eyelids or turning the head can cause serious difficulties. In addition, excessive muscle tension can cause cramps, as well as tingling or numbness in the limbs.
Neurologists at the Yusupov Hospital use modern methods to normalize the condition of a patient with VSD. Highly effective medications are indispensable in the treatment of VSD, the combination of which with physical therapy exercises contributes to the onset of a therapeutic effect in the shortest possible time.
Treatment
If the problem is caused by external negative factors, they should be avoided if possible. If a spasm occurs against the background of any disease, therapy should be aimed at curing it.
At the same time, drugs are used to relieve spasms of cerebral vessels - No-Shpa, Halidor, Dibazol, Doverin, Papazol, Spazmol. They affect the muscular wall of blood vessels, reduce muscle tone, and expand the lumen of blood vessels.
You can also take painkillers for cerebral vasospasm - Analgin, Aspirin.
Antispasmodic analgesics are drugs of a combined composition that eliminate spasms and relieve pain. This group includes Pentalgin, Andipal, Baralgetas, Novigan, Spazgan, Spazmoblok.
To improve cerebral circulation, it is recommended to take nootropic drugs such as Actitropil, Gopantam, Idebenone, Nootropil, Recognan, Piracetam.
For the treatment of cerebrovascular disorders, medicines and dietary supplements based on ginkgo biloba leaf extract are widely used. This plant improves the rheological properties of blood and oxygen supply to the brain, normalizes microcirculation and metabolism in cells, reduces the permeability of vascular cells, and has antithrombotic and antihypoxic effects.
The patient is recommended physiotherapeutic procedures: oxygen therapy, kinesiotherapy, hydrotherapy, magnetic therapy, darsonvalization. Massages in the neck and back of the head help improve blood circulation.
How do tension headaches manifest?
With tension-type headache, the head hurts on both sides in the temples, back of the head, and crown area. The pain itself is pressing or squeezing in nature, but not pulsating. They rarely become strong and painful. Most often, the pain is mild or moderate in intensity. Patients often describe their sensations as “squeezing the head with a hoop,” “girdle pain around the temples,” “pressing pain, like a helmet or helmet.” They may occur:
- in the morning immediately or shortly after waking up, persist throughout the day, often alternately weakening and gaining intensity;
- in the afternoon, especially after suffering stress, anxiety or performing particularly strenuous work, a long stay in a forced uncomfortable position that provokes overstrain of the muscles of the neck and head (most often when working at a computer, machine tool, driving a car, etc.).
The attack begins gradually, although with serious emotional shock it can develop abruptly. It may be accompanied by:
- decreased appetite;
- deterioration of health when staying in a noisy and crowded room;
- a feeling of pressure in the eyes;
- a feeling of stiffness of the head and movements with it;
- unpleasant sensations when combing hair or wearing a hat;
- sleep disturbance, insomnia due to pain in the head that persists even at night.
But HDN does not completely deprive a person of working capacity, although it has a negative effect on it. Also a characteristic feature of tension headaches is an improvement in the condition when experiencing positive emotions, during pleasant activities, rest, and relaxation. In some cases, even switching attention from one task to another, more pleasant one, leads to a decrease in the severity of pain in the head.
When a headache occurs, some patients notice transient or permanent discomfort, a feeling of tension in the back of the head, the back of the neck and the shoulders. Sometimes the muscles in these areas are so tense that outright pain occurs. This is called “coat hanger” syndrome and is mainly caused by prolonged stay in a static position with a bowed head. The severity of muscle tension increases as the intensity and frequency of headache attacks increases.
Tension headaches differ from migraines in the absence of a sensation of pulsation, the bilaterality of the process, as well as the absence of nausea, vomiting, severe photophobia and intolerance to loud sounds. Although sometimes it is still possible to experience slight increased sensitivity to light and sounds.
Chronic tension headaches are somewhat more severe. Although the attacks occur with the same symptoms, their high frequency exhausts the person. This affects not only his ability to perform daily duties, but also affects his psychological state, causing irritation, increased anxiety, sleep disturbances, melancholy, and depressive disorders. All this together significantly reduces the patient’s quality of life.
TTH needs to be differentiated from headaches due to vegetative-vascular dystonia (VSD). In the latter case, in addition to a headache, patients note dizziness, a feeling of palpitations, increased sweating of the palms, trembling hands, tingling in the chest, difficulty breathing, or only some of these symptoms. With VSD, presyncope or even loss of consciousness is often observed.
Prevention
Preventive measures are aimed at maintaining the normal functioning of the circulatory system and strengthening blood vessels. These include:
- normalization of work and rest schedules;
- good sleep;
- moderate exercise;
- hardening;
- to give up smoking;
- reasonable alcohol consumption;
- adequate drinking regime;
- avoiding hypothermia;
- proper nutrition.
Doctors recommend eating more vegetables, fruits and herbs, and giving preference to fish and lean meats. Limit the consumption of butter, coffee, black tea, cocoa, sugar, chocolate, smoked meats, lamb and pork, mayonnaise and sauces, fried foods.
Causes of Prinzmetal's angina
Coronary artery spasm can occur in the following cases:
- hypothermia of the body;
- smoking;
- symptoms of arterial hypertension;
- stress;
- increased cholesterol levels;
- taking medications that slow blood flow;
- consumption of alcohol and drugs.
The disease is more common in patients aged 50 to 60 years. 5 times more common in men than in women. Smoking and alcohol consumption are recognized as the main risk factors. Less commonly, the pathology develops against the background of vasomotor vascular disorders.
Popular questions about cerebral vasospasm
How to understand the cause of a headache?
First of all, it’s worth analyzing the situation - what could be causing the problem? Perhaps a headache occurs when the weather changes, after excessive physical exertion, hypothermia, stress, or frequent lack of sleep. If there is no explainable reason, you should definitely seek help from a doctor.
What drugs can be taken without a doctor's prescription?
Most non-narcotic analgesics and antispasmodics are sold without a prescription.
The most effective drugs?
The best tablets for cerebral vasospasm are combined drugs that have analgesic and antispasmodic effects, for example, Bralangin, Pentalgin and Spazmalgon. Antispasmodics that reduce vascular tone, for example, Papaverine and Drotaverine, are also effective.
How to strengthen blood vessels during VSD
For autonomic dysfunction, drugs with different mechanisms of action are used. No-spa for VSD effectively relieves spasms and eliminates pain. However, this drug should be used only after it has been prescribed by your doctor.
To strengthen blood vessels and muscles during VSD, massages and regular physical therapy exercises are used. Exercise therapy instructors at the Yusupov Hospital Rehabilitation Center select exercises for patients in which physical activity is moderate, and also clearly tell patients how to strengthen blood vessels during VSD. Daily gymnastics under the guidance of experienced trainers improves muscle flexibility and strengthens blood vessels.
Methods for diagnosing the disease
Suspicion of Prinzmetal's angina arises in any case if the patient complains of sharp chest pain at rest or at night. The diagnosis implies that the duration of attacks can range from 30 seconds to 5 minutes, and their number varies up to several dozen within half an hour. In addition, an indirect sign is the subsidence of pain when taking sublingual drugs with a nitrate chemical composition.
The initial assumptions can be confirmed by:
- electrocardiogram in the format of a one-time study or daily monitoring;
- provocative pharmacological tests.