- Classification of diuretics
- When are diuretics used?
- How to take diuretics
- Can it be taken by children?
- Treatment with diuretics
Diuretics are medications with a diuretic effect.
When they enter the body, they prevent the reabsorption (reabsorption) of water and salts dissolved in it in the renal tubules. This increases the rate of urine formation and excretion. In simple terms, diuretics are substances that help the body remove water and salts from the body. Experts have proven that with a decrease in reabsorption by just 1%, the volume of urine doubles. Even when taking medications with little effect, patients report frequent and more abundant urination.
Classification of diuretics
Diuretics differ in chemical composition and other parameters. Conventionally, all drugs can be divided into renal and extrarenal. Renal diuretics are powerful drugs that directly affect the kidneys. Extrarenal drugs increase diuresis (the volume of urine produced over a period of time), but affect the body indirectly.
Based on their chemical composition, renal diuretics are divided into several groups:
- Thiazide (moderate, uniform effect);
- Potassium-containing (help remove chlorides and sodium from the body, but not potassium);
- Salt (loop - increase the excretion of salts).
The most popular drug of the thiazide group is dichlorothiazide. Loop diuretics include furosemide, torsemide and bumetanide. Potassium-containing diuretics are triamterene and amiloride.
Extrarenal diuretics include two categories of drugs: osmotic (potassium acetate) and acid-forming (ammonium chloride, calcium chloride).
A quick and pronounced result from the use of diuretics is observed when taking Furosemide and other saline drugs. Due to their powerful effects, such products are called “ceiling”. They begin to act in 15-30 minutes, and the effect lasts up to 18 hours. These drugs accelerate the excretion of water, potassium chloride, sodium and calcium in the urine. Loop diuretics are used in the complex treatment of patients with chronic heart failure, hypertensive crisis, poisoning, and pulmonary edema.
Potassium-sparing drugs and drugs of the thiazide group have a less pronounced diuretic effect compared to loop diuretics. Thiazides are considered moderately potent diuretics. They begin to work 30-60 minutes after administration and maintain the effect for 6-10 hours.
The effect of potassium-containing drugs differs from drugs of other groups. A popular potassium-sparing diuretic is spironolactone. The medications help remove fluid and sodium from the urine, but prevent the loss of potassium. The effect of taking the drug occurs within a few hours. Most often, such drugs are prescribed in combination with drugs of the thiazide group to provide a diuretic effect and avoid potassium deficiency.
In addition to pharmaceuticals, some plants can enhance urine output. A mild diuretic effect is provided by plantain, birch, cranberry fruits, horsetail, bearberry leaf, and prickly pear. Decoctions and infusions are prepared from them and used as part of multi-component pharmaceutical herbal mixtures.
The selection of diuretic drugs and their dosage should be handled by the attending physician. The drugs differ not only in their chemical composition, but also in the duration of their effect on the body and the presence of side effects.
Furosemide
- Has a hypotensive effect
- Promotes increased removal of water from the body
- Promotes the removal of calcium and magnesium ions
More details
THERE ARE CONTRAINDICATIONS. BEFORE USE, READ THE INSTRUCTIONS CAREFULLY OR CONSULT A DOCTOR
Thiazide diuretics in the treatment of arterial hypertension
In June 2007, at the European Congress on Hypertension in Milan (Italy), new European guidelines for the treatment of arterial hypertension (HTN) were announced. Particular attention of cardiologists was directed to the place of certain classes of drugs in treatment regimens for hypertension.
6 rational combinations of antihypertensive drugs have been proposed [1]:
- thiazide diuretic + angiotensin-converting enzyme (ACE) inhibitor;
- thiazide diuretic + angiotensin receptor blocker;
- calcium antagonist + ACE inhibitor;
- calcium antagonist + angiotensin receptor blocker;
- calcium antagonist + thiazide diuretic;
- beta blocker + dihydropyridine calcium antagonist.
Based on the above, we can conclude that calcium antagonists (4 times) and thiazide diuretics (3 times) appear most often in combinations.
Thiazide diuretics have long been used as agents for the treatment of hypertension. In the 2007 European guidelines, the target groups for whom diuretics are preferred include elderly patients with systolic hypertension as well as heart failure [1].
However, the use of medium and high doses of thiazide diuretics is currently considered undesirable: for example, hydrochlorothiazide at a dose of 100 mg/day increases the risk of sudden death, and at doses of 50–100 mg/day does not prevent the development of coronary heart disease (CHD). In this regard, the recommended doses of thiazide diuretics are currently 12.5–25 mg/day, which do not always achieve an adequate diuretic and antihypertensive effect [2]. In addition, limiting the doses of thiazide diuretics is also associated with their negative effect on carbohydrate, fat and purine metabolism [3]. Therefore, in the 2007 European recommendations, gout was included as absolute contraindications to the use of thiazide diuretics, and metabolic syndrome and impaired glucose tolerance were included as relative contraindications. In addition, special emphasis is placed on the fact that high doses of diuretics cannot be prescribed to pregnant women due to the possibility of reducing circulating blood volume (CBV) and deteriorating blood supply to the fetus. However, we should not forget that diuretics can delay the development of chronic heart failure in patients with hypertension (Davis BR, 2006).
Thus, it is obvious that the scope of application of thiazide diuretics in the treatment of hypertension is quite limited. In this regard, the thiazide-like diuretic indapamide is of particular interest.
Indapamide has a dual effect, due to which it has a short-term and long-term antihypertensive effect. The short-term effect is associated with the effect of the drug on the proximal part of the distal tubules of the nephron and represents a natriuretic effect characteristic of representatives of the diuretic class as a whole. As for the long-term antihypertensive effect, it is unique to indapamide and occurs due to a direct vasodilating effect on the smooth muscle cells of the vascular wall [4].
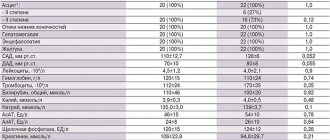
The antihypertensive effect of indapamide retard 1.5 mg was compared with amlodipine (5 mg/day) and hydrochlorothiazide (25 mg/day) in a study of 605 patients with hypertension treated with the above drugs for 3 months. The number of patients responding to monotherapy was slightly higher in the indapamide-retard group (75.3%) compared with the amlodipine (66.9%) and hydrochlorothiazide (67.3%) groups. In the subgroup of patients with isolated systolic hypertension, a similar trend was observed: the number of respondents in the indapamide-retard group was 84.2%, while in the amlodipine group - 80%, hydrochlorothiazide - 71.4% [5].
The multicenter LIVE (Left ventricle hypertrophy: Indapamide Versus Enalapril) study examined the effect of indapamide and enalapril therapy on regression of left ventricular myocardial mass (LVMM). 505 patients (255 - indapamide group; 250 - enalapril group) with mild and moderate hypertension were prescribed indapamide retard 1.5 mg/day or enalapril at a dose of 20 mg once a day for 1 year. Therapy with indapamide led to a significant decrease in LVMM (p < 0.001); similar results were not obtained in the enalapril group. Indapamide also reduced the severity of left ventricular hypertrophy (LVH) to a greater extent than enalapril (p < 0.049) [6, 7].
Thiazide diuretics have been prescribed in combination with ACE inhibitors for a very long time: many pharmaceutical companies have even developed fixed combinations of these components. In a large number of studies, the combination of indapamide with perindopril also showed good results. However, there are not many studies on the effectiveness of combinations of indapamide with other classes of the drug.
In this regard, we found the work of Hashimoto J. et al interesting. [8], who added indapamide at a dose of 1 mg to 76 patients receiving ACE inhibitors, angiotensin receptor blockers, and calcium antagonists as monotherapy, but failed to achieve target blood pressure (BP) values with this treatment. During 4 weeks of combination therapy in these three groups, the dynamics of the level of 24-hour blood pressure monitoring, home blood pressure measurements, and random blood pressure measurements were assessed. In all groups, a significant decrease in systolic blood pressure (SBP) and diastolic blood pressure (DBP) was noted. The decrease in SBP in the evening and pulse blood pressure was significantly more pronounced in the angiotensin receptor blocker + indapamide group compared to the calcium antagonist + indapamide group. Thus, the addition of indapamide to antihypertensive therapy led to an additional hypotensive effect that lasted 24 hours.
Until recently, only three classes of drugs were thought to have nephroprotective effects: ACE inhibitors, angiotensin receptor blockers, and calcium antagonists (mainly phenylalkylamines). The nephroprotective effect of thiazide-like diuretics was demonstrated in the NESTOR study [9]. In 570 patients with hypertension and type 2 diabetes mellitus, a comparative study of the effect of indapamide retard 1.5 mg and enalapril 10 mg on the severity of microalbuminuria (MAU) was carried out during one-year therapy. There was a decrease in MAU by 37% in the enalapril group and by 45% in the indapamide-retard group. Thus, the nephroprotective effect of indapamide retard 1.5 mg turned out to be comparable and even slightly higher than that of enalapril.
Another study examined the effect of indapamide retard at a dose of 1.5 mg prescribed for 3 months, compared with placebo, on 24-hour blood pressure monitoring, carbohydrate and lipid metabolism in patients with type 2 diabetes mellitus [10]. A significant decrease in average daily blood pressure was detected in the indapamide group compared to placebo. In addition, there was no effect of the therapy on electrolytes, creatinine, lipid spectrum, uric acid, liver transaminases, insulin levels, glycosylated hemoglobin and glucose tolerance test results.
Considering that diuretics have long established themselves as the drug of choice for the treatment of elderly patients, especially those with isolated systolic hypertension (ISAH). The multicenter X-CELLENT study included 1,758 patients with systolic-diastolic hypertension or ISAH, who were then randomized into 4 groups, which received monotherapy with indapamide retard 1.5 mg/day, amlodipine 5 mg/day, candesartan cilexetil 8 mg/day and placebo for 3 months. Compared to the placebo group, a significant decrease in blood pressure was noted in all groups. The advantage of indapamide in patients with ISAH was the virtually no effect of the drug on normal DBP values while reducing SBP; the remaining drugs reduced both SBP and DBP. In addition, in this group of patients, indapamide retard reduced average daily SBP to a greater extent than amlodipine. All three types of therapy were well tolerated [11].
As we indicated above, a dose of hydrochlorothiazide of 12.5–25 mg/day is considered metabolically neutral. In the work of A. A. Semenkin et al. A comparative study of the antihypertensive effectiveness and metabolic effects of indapamide retard (1.5 mg/day) and hydrochlorothiazide (25 mg/day) was conducted. Despite the comparable antihypertensive effect, in the group of patients receiving hydrochlorothiazide, after 3 months there was a significant increase in triglyceride levels by 15.3% (p < 0.05) and glucose by 12.2% (p < 0.05), and also a significant deterioration in endothelium-dependent vasodilation by 17% (p < 0.05) [12].
Of interest is the potential expansion of indications for the use of indapamide, in particular, its use in the treatment of chronic heart failure accompanied by edema syndrome. In one recent study in patients with persistent peripheral edema, indapamide 2 mg was added to furosemide (40–120 mg/day), which resulted in a significantly greater diuretic effect without a significant effect on plasma potassium and creatinine levels [13].
Thus, the original indapamide has more than convincingly proven its antihypertensive effectiveness and organoprotective properties during research. In an attempt to combine low cost with high quality of the drug to provide the majority of patients with hypertension with drugs of adequate action, modern generics of indapamide and, in particular, the drug “Ravel SR”, produced in a dose of 1.5 mg, are of particular interest. The drug has successfully proven itself after a trial in Slovenia in 2005–2006. study [4], which examined its antihypertensive efficacy and tolerability. The drug was prescribed to 1419 patients (58.1% women, mean age 61.9 ± 11.6 years), who showed a decrease in SBP by 14.1% and DBP by 11.1%. The development of adverse events while taking Ravel SR was noted in only 2.5% of patients (the most common were dry mouth and dizziness - 0.42% each, and 1 patient required correction of potassium levels due to the development of hypokalemia without discontinuation of the drug) .
The effectiveness and tolerability of Ravel SR was also studied in domestic studies. S. V. Nedogoda et al. [14] compared therapy with Ravel SR 1.5 mg/day and hydrochlorothiazide 25 mg in patients with hypertension and obesity. Patients of the 1st group received Ravel SR for 6 months, patients of the 2nd group were prescribed hydrochlorothiazide at a dose of 25 mg/day for the first 3 months, and then they were transferred to Ravel SR (3 months). The results of the study showed that while taking Ravel SR, achieving target blood pressure values occurred 15% more often than with hydrochlorothiazide. It was noted that only on therapy with Ravel SR there was an improvement in vascular elasticity (as assessed by pulse wave velocity) and a decrease in myocardial hypertrophy, as well as an improvement in carbohydrate and lipid metabolism.
Also of interest are the results of the BOLERO program (Basic treatment and antihypertensive effect: the drug “Ravel SR” in patients with arterial hypertension), aimed at studying the antihypertensive effectiveness of the slow-release form of the drug and its effect on quality of life. It was shown that the use of indapamide retard for 2 months led to a decrease in SBP and DBP in men by 18%, and in women by 15%. During treatment, cardiovascular risk decreased to the same extent in men and women, and the improvement in quality of life was more noticeable in the group of women [15].
The emergence of each new high-quality and safe generic drug is a step towards ensuring that Russian patients demonstrate higher adherence to hypertension treatment. Currently, patients with hypertension in the Russian Federation who have a target blood pressure level do not exceed 5–15% of the population, while in Western Europe there are more than 30% of such patients. The drug "Ravel SR" (indapamide retard) 1.5 mg as an antihypertensive drug with a mild diuretic effect has every opportunity to expand the boundaries of the use of diuretics outlined by modern recommendations for the treatment of hypertension.
For questions regarding literature, please contact the editor.
D. A. Napalkov , Candidate of Medical Sciences MMA named after. I. M. Sechenova , Moscow
When are diuretics used?
Due to the diuretic effect of diuretics, they are used in the complex treatment of diseases and disorders in the body that are accompanied by edema. First of all, we are talking about diseases of the heart and blood vessels. Diuretics eliminate fluid retention and excess salts, which helps:
- normalize the balance of mineral compounds;
- lower blood pressure;
- ease the work of the heart;
- reduce swelling of the limbs;
- get rid of congestion in the lungs.
When combined with other medications, diuretics relieve shortness of breath and other symptoms of chronic heart failure.
In addition to cardiac diseases, diuretics are used in the treatment of a number of other diseases. Diuretics are used for chronic renal failure and nephrotic syndrome (edema), liver cirrhosis, glaucoma, diabetes insipidus, gout, neonatal edema syndrome, neurological diseases that lead to increased intracranial pressure.
How to take diuretics
Preparations for diuretic therapy are available in the form of tablets, powders and solutions for intravenous administration. Depending on the clinical case, the doctor selects one drug or a combination of several drugs with different mechanisms of action.
The basic rule for taking diuretics is to use the medicine on an empty stomach and take it with plenty of water.
Blood Pressure Tablets: Part I
High blood pressure is one of the most common health problems in Russia. This disease is especially common in older people who have to “take pills” to feel good and relieve stress on the heart. What is blood pressure, why does it rise too much, how diuretic medications help normalize it and how to take them correctly - read about all this in our article.
What is blood pressure
When the heart muscle contracts, it forcefully pushes out a large volume of blood, putting pressure on the walls of the blood vessels. Depending on the location, this pressure is called arterial (BP), venous and capillary. Pushing a fluid as thick as blood through 100 billion capillaries is no easy task. Due to the natural resistance of this complex network of microscopic vessels, the blood pressure “at the entrance” to the heart is much lower than “at the exit” from it.
The blood pressure “at the exit” of blood from the heart (that is, at the moment of its contraction) is called systolic, and the blood pressure “at the entrance” to the heart at the moment of its relaxation is called diastolic.
The average norm for an adult is considered to be 120/80 mm. rt. Art.; The first number in this case means systolic blood pressure, and the second number means diastolic. Thus, normally, the resistance of the capillary network “eats” 34% of the initial “power” of the blood flow.
In practice, the ratio of the two blood pressure readings varies greatly among different people and even within the same person at different points in time. It depends on a number of factors: heart rate, condition of blood vessels, elasticity of their walls (this parameter is skillfully regulated by the brain), etc.
Why is blood pressure rising?
Arterial hypertension (AH), also known as hypertension, is one of the most common diseases in the world. According to the latest WHO data, about 1.13 billion people worldwide suffer from high blood pressure. Blood pressure readings of 140/90 mm are considered elevated. rt. Art. and higher at rest.
The most common symptoms of a hypertensive crisis (a sharp increase in blood pressure in patients with hypertension) are headache, shortness of breath, chest pain and fatigue. Some patients experience dizziness, hear ringing in the ears, or notice redness on the face and chest.
The main cause of hypertension is excessive activity of the renin-angiotensin system (RAS). It is a cascade of chemical reactions that occur in the body in response to a decrease in blood pressure: the enzyme renin contained in the kidneys is converted into the enzyme angiotensin I, and then into angiotensin II. The latter is a powerful vasoconstrictor. The narrower the vessels, the higher the pressure. Angiotensin II also reduces the excretion of sodium and water by the kidneys. The more water in the tissues of the vessels, the smaller their diameter, which means the higher the pressure.
Arterial hypertension is also associated with an excess of calcium in the cells of blood vessels, as well as with an increased concentration of sodium in the vessels and in the blood. Many people know that calcium is good for bones and teeth, but not everyone realizes how important it is for the body as a whole. In fact, calcium is necessary for the transmission of nerve impulses, muscle contraction, blood clotting, the immune response, and so on. Without this metal we would not be able to think, move, or even live.
But in the body, as in life, everything is good in moderation. Calcium overload in vascular cells leads to hypertrophy of their muscle tissue. And this, in turn, means a thickening of the vessel wall and a decrease in its lumen. The “tube” becomes narrower, and, as a result, the pressure on its walls increases.
Why does calcium overload occur? Calcium metabolism in the body is regulated by hormones, and their level, in turn, depends on the concentration of other important substances. Thus, risk factors for hypertension are: obesity, sedentary lifestyle and hyperlipidemia (fat concentration), diabetes, smoking and alcoholism. In addition, old age is a key risk factor.
In the case of sodium, the risk factor is the abuse of salty foods and hormonal disorders that slow down the removal of this element from tissues. Sodium can accumulate in the blood, increasing its volume by binding water molecules. The more blood passes through the vessels per unit time, the greater the pressure on the walls of the vessels. In addition, the accumulation of sodium in the endothelium (a thin layer of cells lining the inside of blood vessels) leads to its swelling (essentially, edema) and, as a consequence, to a narrowing of the lumen of the vessel.
How do diuretics work?
In this article, we will look at only one class of drugs that are used to treat hypertension - diuretics. These medications are designed to “correct the situation” with sodium, while calcium metabolism and the functioning of the RAS are corrected by other drugs, which we will talk about in the following materials.
Diuretics improve the excretion of urine from the body, and along with it, water. Excess sodium and water leave the blood, its volume decreases and blood pressure decreases.
Diuretics act on the nephron, a structural unit of the kidney that performs filtration, reabsorption (reabsorption) and secretion of various substances. They reduce the return of previously “filtered” sodium and potassium ions into the blood. The lower the sodium reabsorption, the lower the water reabsorption. Instead of entering the blood, the water leaves in the urine.
Three types of diuretics are used to treat arterial hypertension: loop, thiazide and potassium-sparing. Loop diuretics are so called because they act on a special part of the nephron - the loop of Henle. Potassium-sparing ones differ from others in their ability to influence only sodium ions. And all thiazide diuretics are derivatives of the substance benzothiadiazine.
The latter are also capable of acting directly on the walls of blood vessels. They reduce the concentration of sodium ions in the endothelium, which reduces its swelling.
Examples of loop diuretics are torasemide and furosemide. Thiazide diuretics include indapamide. Potassium-sparing diuretics include spironolactone and triamterene.
How to take diuretics?
When taking a number of diuretics, especially loop diuretics as the most “powerful” ones, you should remember the risk of hypokalemia (potassium deficiency). It leads to serious problems with various muscle tissues - myalgia, paralysis, breathing problems and intestinal obstruction.
This is a relatively rare condition because potassium is a very common element in food. However, such risks can be caused by a combination of the action of diuretics, which “expel” potassium into the urine and, say, the consequences of prolonged diarrhea or laxative abuse. Also, medications called beta-agonists (salbutamol, fenoterol, etc.) can affect potassium concentration.
In this regard, we recommend that you begin treatment with diuretics only under the supervision of a doctor who will not prescribe incompatible drugs. Obviously, this problem does not apply to potassium-sparing diuretics.
Diuretics do not have strict guidelines for when to take oral forms, however, as is the case with many other drugs, it is better to take them before meals or a couple of hours after. Any medicine is unlikely to benefit from unnecessary interactions with food.
We wish you health, eternal 120/80 and a rational approach to treatment, including professional help from doctors!
Mark Volkov, editor of the online magazine for pharmacists and medical workers “Katren-Style”
Photo depositphotos.com The author’s opinion may not coincide with the opinion of the editors
Treatment with diuretics
When prescribing diuretics, doctors adhere to the principles of rational therapy:
- At the first stage, a medicine with a moderate effect is prescribed.
- At the beginning of therapy, a minimum dosage of the drug is recommended with a gradual increase until the desired effect of diuretics is achieved. With intensive treatment, it is normal to increase the daily volume of urine by 800-1000 ml, and with maintenance therapy - by no more than 200 ml per day.
- For the majority, the optimal combination of diuretics with different mechanisms of action is optimal.
- To achieve a therapeutic effect, medications must be taken daily for the period recommended by your doctor.
It is important to be aware of the side effects of diuretics. Accidental or intentional abuse of such drugs leads to disruption of water and electrolyte balance. With prolonged use or an incorrectly selected dosage of diuretics, the risk of side effects increases:
- dehydration;
- heart rhythm disturbances;
- excessive decrease in blood pressure.
Headaches and muscle pains, nausea, vomiting, disturbances in the functioning of the gastrointestinal tract, weakness and convulsions, and drowsiness may also be observed. If you are hypersensitive to the drug, an allergic reaction may occur.
With prolonged diuretic therapy, mandatory monitoring of potassium and creatinine is indicated. If these indicators deviate significantly from the norm, a diuretic dosage adjustment or its complete discontinuation is required.
PHARMACOTHERAPY OF HYPERTENSION. PART 2. DIURETICS AS ANTIHYPERTENSIVE DRUGS
Information about various groups of diuretic drugs is presented, their pharmacodynamics, mechanism of action and side effects are described. Recommendations are given for the combined use of diuretics for osteoporosis and diabetes mellitus concomitant with arterial hypertension.
The paper presents information of different groups of diuretics, describes their pharmacodynamics, mechanism of action and side effects. Recommendations are given on combined diuretic therapy for contaminant arterial hypertension, osteoporosis, and diabetes mellitus.
B.A. Sidorenko, D.V. Preobrazhensky - Medical Center of the Administration of the President of the Russian Federation, Moscow
BA Sidorenko, DV Preobrazhensky – Medical Center, Administration of Affairs of the President of the Russian Federation, Moscow
* Part I see No. 8
Part II* Diuretics as antihypertensive drugs
Diuretics began to be used for long-term treatment of hypertension and other forms of arterial hypertension in the late 50s; the first thiazide diuretic, chlorothiazide, was created in 1957. In the 60s, benzothiadiazine derivatives with a stronger diuretic effect than chlorothiazide were synthesized; Among these drugs, hydrochlorothiazide is the most widely used. Thiazide diuretics were initially used as second-line antihypertensive drugs when reserpine, guanethidine, methyldopa and hydralazine, which were then used, were insufficiently effective. But quite soon it became clear that thiazide diuretics themselves are effective antihypertensive drugs and can be used for long-term monotherapy of hypertension. Along with benzothiadiazine derivatives, some heterocyclic compounds have a moderate sodium and diuretic effect - phthalimidines (chlorthalidone, clorexolone), quinazolinones (metolazone, hinetazone), chlorobenzamides (clopamide, indapamide, xipamide) and benzenesulfonamides (mefruzide). These heterocyclic compounds are usually called thiazide-like diuretics. In the early 60s, the so-called “loop” diuretics were created almost simultaneously - fruzemide (furosemide) in Germany and ethacrynic acid in the USA. Furosemide and ethacrynic acid differed from thiazide diuretics in having a significantly more potent sodium and diuretic effect, possible due to the fact that they act throughout the thick part of the ascending limb of the loop of Henle. Furosemide and ethacrynic acid are used mainly in the treatment of heart failure (both acute and chronic), as well as hypertensive crises. The antihypertensive effect of loop diuretics is generally less pronounced than that of thiazide and thiazide-like diuretics. Therefore, until recently they were not considered as first-line antihypertensive drugs for long-term treatment of hypertension. Loop diuretics were recommended for use as antihypertensive drugs only in patients with concomitant renal failure, in which thiazide diuretics are usually ineffective. Potassium-sparing diuretics (amiloride, triamterene, spironolactone) are rarely used as monotherapy for the treatment of hypertension, although there is evidence that spironolactone has fairly high antihypertensive activity. Potassium-sparing diuretics are usually prescribed in combination with thiazide and loop diuretics to reduce potassium loss.
Thus, currently, three main groups of diuretic drugs are used in the treatment of hypertension:
|
Clinical pharmacology of diuretics
Diuretics can be classified in different ways; for example, by chemical structure, by the mechanism of diuretic action (saluretics and osmotic diuretics), by the localization of action in the nephron. Diuretics are often divided into three groups depending on the site of their action in the nephron, which determines the severity of the natriuretic effect, expressed as a percentage of excreted sodium from the total amount of sodium filtered in the glomeruli. Potent diuretics
(i.e., causing excretion of more than 15–20% of filtered sodium): • organic mercury compounds (not currently used in clinical practice);
• derivatives of sulfamonlanthranilic acid (furosemide, bumetanide, pyretanide, torasemide, etc.); • derivatives of phenoxyacetic acid (ethacrynic acid, indacrinone, etc.). Diuretics with a moderately pronounced natriuretic effect
(i.e., causing the excretion of 5-10% of filtered sodium): • benzothiadiazine derivatives (thiazides and hydrothiazides) - chlorothiazide, hydrochlorothiazide, bendroflumethiazide, polythiazide, cyclothiazide, etc.;
• heterocyclic compounds similar in the mechanism of tubular action to thiazide diuretics - chlorthalidone, metolazone, clopamide, indapamide, xipamide, etc. Low-acting diuretics
(i.e., causing excretion of less than 5% of filtered sodium): • potassium-sparing diuretics - amiloride, triamterene, spironolactone;
• carbonic anhydrase inhibitors – acetazolamide, etc.; not used in the treatment of arterial hypertension; • osmotic diuretics – mannitol, urea, glycerin, etc.; are not used in the treatment of arterial hypertension. Thiazide, loop and potassium-sparing diuretics used in the treatment of hypertension are distinguished by the site of action at the level of the renal tubules. Thus, thiazide and thiazide-like diuretics suppress the reabsorption of sodium ions at the level of that part of the thick segment of the ascending limb of the loop of Henle, which is located in the renal cortex, as well as in the initial part of the distal tubules. Loop diuretics have been said to affect the reabsorption of sodium ions in that part of the thick segment of the ascending limb of the loop of Henle, which is located in the renal medulla. Finally, potassium-sparing diuretics inhibit the reabsorption of sodium ions at the level of the distal convoluted tubule and collecting duct. Thiazide and thiazide-like diuretics
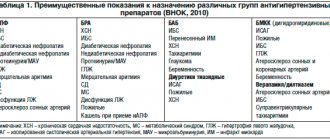
are characterized by a more moderate natriuretic (and diuretic) and longer-lasting effect than loop diuretics, which is explained by the localization of their action in the nephron (Table 1).
The localization of the renal effects of thiazide diuretics determines their other features. The greatest diuretic effect is achieved when prescribing relatively low doses of thiazide diuretics, i.e. they have a relatively low “ceiling”. The above applies not only to the diuretic, but also to the antihypertensive effect of thiazide and thiazide-like diuretics. Thus, relatively low doses of diuretics (12.5–25 mg of hydrochlorothiazide per day or equivalent doses of other thiazide diuretics) cause a significant decrease in blood pressure (BP). With further increases in the dose of thiazide diuretics, the antihypertensive effect increases only to a small extent, but the incidence of hypokalemia and other serious adverse reactions increases significantly [1]. Table 1. Comparative characteristics of diuretics used in the treatment of hypertension
| Drugs | Bioavailability, % action, h | Elimination duration | Main path |
| Thiazide and thiazide-like diuretics | |||
| Hydrochlorothiazide | 60–80 | 6–18 | Kidneys |
| Indapamide | … | 12–24 | Kidneys + liver |
| Xipamide | 90 | 12–24 | Same |
| Metolazone | 50–60 | 12–24 | |
| Chlorthalidone | 65 | 24–72 | Kidneys+liver |
| Chlorothiazide | 10 | 6–12 | Kidneys |
| Loop diuretics | |||
| Bumetanide | 60–90 | 2–5 | Kidneys + liver |
| Torasemide | 80–90 | 6–8 | Same |
| Furosemide | 10–90 | 2–4 | Kidneys |
| Potassium-sparing diuretics | |||
| Amiloride | 50 | 6–24 | Kidneys |
| Triamterene | 50 | 8–12 | Kidneys + liver |
| Spironolactone | 70 | 3–5 days | Liver |
| Note. Literature data regarding the duration of action of various diuretics are extremely contradictory: compare Z. Opte [1], M. Kaplan [2], as well as R. Ureger et al., “Diuretics” (1995) or E. Brauhwald” Heart disease ( 1997). | |||
In addition, the diuretic, and therefore the antihypertensive effect of thiazide diuretics is significantly weakened in patients with renal failure (serum creatinine level above 2.0 mg/dL; glomerular filtration rate less than 30 ml/min). For this reason, thiazide and thiazide-like diuretics are not recommended for the treatment of hypertension in patients with impaired renal function [2]. Thiazide diuretics (unlike loop and potassium-sparing diuretics) reduce the excretion of calcium ions in the urine. The calcium-sparing effect of thiazide and thiazide-like diuretics allows them to be prescribed for the treatment of arterial hypertension in patients with concomitant osteoporosis. Osteoporosis, as is known, often occurs in women after menopause, as well as in elderly patients leading a sedentary lifestyle, and predisposes to bone fractures, in particular the femoral neck. According to some observations, bone fractures in hypertensive patients receiving thiazide diuretics for a long time are observed less frequently than in patients receiving other antihypertensive drugs. Given the calcium-sparing effect of thiazide diuretics, they are currently considered first-line antihypertensive drugs in the treatment of patients with hypertension in combination with osteoporosis [3]. Along with the natriuretic effect, all thiazide diuretics increase the urinary excretion of potassium and magnesium ions and at the same time reduce the excretion of uric acid. Therefore, thiazide, as well as loop diuretics, are contraindicated in patients with hypokalemia (normal serum potassium level 3.5–5.0 mmol/l), gout or hyperuricemia (normal blood uric acid level in men 3.6–8. 5 mg/dl, in women – 2.3–6.6 mg/dl). Table 2. Diuretics used for long-term therapy of hypertension
| Drugs | Average doses (mg/day) | Typical side effects |
| Thiazide and thiazide-like diuretics | ||
| Hydrochlorothiazide | 12,5–50 | Hypokalemia, hypomagnesemia, hyperuricemia, disorder glucose tolerance, hypertriglyceridemia, hyper- cholesterolemia, impotence, hyponatremia, hypochloremia alkalosis (indapamide causes minor changes in blood lipid composition) |
| Indapamide | 1,25–5 | |
| Klopamide | 10–20 | |
| Xipamide | 10–40 | |
| Metolazone | 2,5–5 | |
| Chlorthalidone | 12,5–50 | |
| Loop diuretics | ||
| Bumetanide | 0,5–4 | Hypotension, hypokalemia, hypomagnesemia, hyperuricemia, hyponatremia, impaired glucose tolerance, hypo- chloremic alkalosis, hypercalciuria, hearing loss (ethacrynic acid does not contain a sulfhydryl group and is the most ototoxic) |
| Torasemide | 2,5–10 | |
| Furosemide | 40–240 | |
| Ethacrynic acid | 25–100 | |
| Potassium-sparing diuretics | ||
| Amiloride | 5–10 | Hyperkalemia, hyponatremia, hyperchloremic acidosis The same plus kidney damage (rare) The same plus gynecomastia and sexual dysfunction in men and hirsutism and menstrual irregularities (dysmenorrhea) in women |
| Triamterene | 25–100 | |
| Spironolactone | 25–100 | |
The most common metabolic (biochemical) side effects observed when using thiazide diuretics are hypokalemia, hypomagnesemia and hyperuricemia. Excessive loss of potassium and magnesium ions during treatment with high doses of thiazide diuretics explains other known side effects - the occurrence of ventricular arrhythmias and disorders of carbohydrate metabolism. The appearance or increase in ventricular extrasystole during treatment with high doses of thiazide diuretics (without simultaneous administration of potassium-sparing diuretics or potassium salts) was observed in a number of controlled studies. It is assumed that the increased incidence of sudden death in patients with essential hypertension with left ventricular hypertrophy (according to ECG criteria) is associated with ventricular arrhythmias caused by hypokalemia caused by thiazide or thiazide-like diuretics. To prevent the development of hypokalemia, in recent years, for the treatment of hypertension, it has been recommended to use small doses of thiazide diuretics (12.5–50 mg hydrochlorothiazide per day or equivalent doses of other drugs) in combination with a potassium-sparing diuretic (amiloride, triamterene or spironolactone) or potassium salts ( approximately 40–60 mEq of potassium per day). Combining angiotensin-converting enzyme (ACE) inhibitors with thiazide diuretics also prevents the development of hypokalemia. Thiazide diuretics may interfere with carbohydrate metabolism, resulting in increased serum glucose and insulin concentrations. Hyperglycemia during treatment with thiazide diuretics rarely reaches clinically significant levels. Hyperinsulinemia is believed to occur in response to decreased sensitivity of peripheral tissues to the action of insulin and may predispose to the development of atherosclerosis. In patients with diabetes mellitus, the use of thiazide diuretics can cause decompensation of the disease and, in very rare cases, especially in the elderly, provoke the development of hyperosmolar non-ketonemic diabetic coma. Table 3. Effect of diuretics on key outcomes of hypertension: meta-analysis of randomized placebo-controlled trials [8]
| Exodus | Relative risk of an event depending on the dose of diuretics | |
| high | low | |
| Brain stroke | 0,49 (0,39–0,62) | 0,66 (0,55–0,78) |
| Cardiac ischemia | 0,99 (0,83–1,18) | 0,72 (0,61–0,85) |
| Congestive heart failure | 0,17 (0,07–0,41) | 0,58 (0,44–0,76) |
| Cardiovascular mortality | 0,78 (0,62–0,97) | 0,76 (0,65–0,89) |
| Overall mortality | 0,88 (0,75–1,03) | 0,90 (0,81–0,99) |
| Note. Doses of hydrochlorothiazide were considered high: at least 50 mg/day, bendroflumethiazide—at least 500 mg/day, methyclothiazide—at least 5 mg/day, and trichloromethiazide—at least 5 mg/day. In brackets are extreme values. | ||
When treated with thiazide and thiazide-like diuretics, the content of triglycerides (by 10–20%) and total cholesterol (by 5–10%) in the blood increases. Disturbances in blood lipid composition are more pronounced when using medium or high doses of thiazide diuretics (more than 25 mg of hydrochlorothiazide per day) [4]. Thiazide diuretics may cause impotence. The incidence of impotence increases significantly with long-term use of medium or high doses of drugs (more than 25 mg of hydrochlorothiazide or chlorthalidone per day). Cases of the development of pancreatitis, intrahepatic cholestasis, vasculitis, pneumonitis, interstitial nephritis, leukopenia and thrombocytopenia during treatment with thiazide diuretics have been described. Among thiazide and thiazide-like diuretics, hydrochlorothiazide is considered the prototype drug. The diuretic effect of chlorothiazide is more short-term than hydrochlorothiazide, and polythiazide, on the contrary, is longer lasting (see Table 1). Thiazide-like diuretics such as clopamide, chlorthalidone, metolazon and indapamide have a longer diuretic effect than hydrochlorothiazide. Among the thiazide-like diuretics, three drugs stand out: indapamide, xipamide and metolazone. Indapamide and xipamide
According to their chemical structure, they, like clopamide, belong to chlorobenzamide derivatives.
Indapamide differs from other thiazide and thiazide-like diuretics in that, along with the diuretic effect, it has a direct vasodilator effect on the systemic and renal arteries. The vasodilating effect of indapamide is explained by the fact that it is a weak calcium antagonist. With the same antihypertensive effectiveness as other thiazide and thiazide-like diuretics, indapamide does not have a significant effect on blood lipid composition and carbohydrate metabolism. Unlike other diuretics, indapamide does not appear to impair the sensitivity of peripheral tissues to the action of insulin [5]. With long-term use in patients with moderate hypertension and impaired renal function, indapamide increased the glomerular filtration rate, while hydrochlorothiazide decreased it [6]. The incidence of hypokalemia with indapamide does not appear to be lower than with other thiazide diuretics. Therefore, among thiazide and thiazide-like diuretics, indapamide is the drug of choice for the treatment of arterial hypertension in patients with atherogenic dyslipidemia, diabetes mellitus and moderate renal failure (glomerular filtration rate more than 50 ml/min). Xipamide, in its pharmacodynamic characteristics, is more similar to a loop diuretic than a thiazide diuretic. Firstly, xipamide has a significant sodium and diuretic effect even in patients with severe renal failure (glomerular filtration rate less than 30 ml/min). Secondly, unlike thiazide and thiazide-like diuretics, xipamide increases the excretion of calcium ions in the urine. Metolazone
is also effective for renal impairment.
In addition, clinical studies show that it may enhance diuresis caused by furosemide. The combination of metolazone and furosemide is used in the treatment of patients with refractory edema. Loop diuretics are characterized by the following features.
Firstly, they provide a pronounced but short-term diuretic effect (see Table 1).
During the period of action of loop diuretics, the excretion of sodium ions in the urine increases significantly, but after the cessation of the diuretic effect of the drugs, the rate of excretion of sodium ions decreases to a level below the initial level. This phenomenon is called the “ricochet phenomenon” (or recoil). It is believed that the basis of the “rebound phenomenon” is a sharp activation of the renin-angiotensin and, possibly, other antinatriuretic neurohumoral systems in response to massive diuresis caused by loop diuretics. The existence of the “rebound phenomenon” explains why, when taken once daily, loop diuretics may not have a significant effect on the daily excretion of sodium ions. The pronounced excretion of sodium ions during the diuretic effect of short-acting loop diuretics (for example, furosemide and bumetanide) is compensated by excessive retention of sodium ions after the end of the diuretic effect. To achieve the removal of sodium ions from the body, short-acting loop diuretics must be prescribed 2 times a day. When prescribed once daily, loop diuretics may not be effective enough as antihypertensive drugs. Long-acting loop diuretics do not appear to have a rebound effect and are therefore more effective in the treatment of hypertension than furosemide and bumetanide. Recent studies have shown that the long-acting loop diuretic torasemide, administered at a dose of 2.5 mg once daily, without causing significant diuresis, leads to the same significant reduction in blood pressure as hydrochlorothiazide, chlorthalidone and indapamide [7]. The second feature of loop diuretics is that their diuretic effect increases significantly as the dose increases, i.e. Unlike thiazide diuretics, loop drugs have a high “ceiling” of effective doses. Thirdly, loop diuretics remain effective at low glomerular filtration rates, which allows their use for the treatment of arterial hypertension in patients with renal failure. Finally, loop diuretics (primarily furosemide) can be administered intravenously. Therefore, they are widely used in the treatment of hypertensive crises. Adverse reactions when using loop diuretics are generally the same as during treatment with thiazide and thiazide-like drugs. Loop diuretics, like thiazide drugs, are contraindicated in patients with hypokalemia, gout and hyperuricemia. Potassium-sparing diuretics
prevent urinary potassium loss by acting at the level of the distal convoluted tubule and collecting duct as either a competitive aldosterone antagonist (spironolactone) or a direct inhibitor of potassium ion secretion (amiloride, triamterene).
As monotherapy, spironolactone is used in the treatment of so-called “idiopathic hyperaldosteronism,” when hypersecretion of aldosterone is caused by bilateral hyperplasia of the adrenal cortex. In all other cases of hypertension, both spironolactone and amiloride and triamterene are prescribed, usually in combination with thiazide or loop diuretics as potassium-sparing drugs. Of the potassium-sparing diuretics, spironolactone is best used for combination therapy, since it counteracts the kaliuretic effect of aldosterone, which is secreted in increased quantities in hypertensive patients receiving thiazide or loop diuretics. Hypersecretion of aldosterone during diuretic treatment is associated with excessive activation of the renin-angiotensin system. Of the side effects of spironolactone, in addition to hyperkalemia, the most serious are gynecomastia and impotence in men and menstrual irregularities (dysmenorrhea) and hirsutism in women. All these side effects are more common with long-term administration of high doses of spironolactone (more than 100 mg/day) and in patients suffering from liver disease or alcoholism. Amiloride and triamterene are used in combination with thiazide or loop diuretics. They enhance the natriuretic effect of stronger diuretics, but weaken their kaliuretic effect. Hyperkalemia is the most serious adverse reaction observed with amiloride and triamterene, but is rare when potassium-sparing diuretics are given in combination with thiazide or loop diuretics. For long-term therapy, it is better to use amiloride rather than triamterene, which is excreted by the kidneys and in some cases can cause kidney damage. Cases of the development of acute renal failure have been described with the simultaneous use of triamterene and indomethacin [1, 2]. All potassium-sparing diuretics are contraindicated in the presence of hyperkalemia (serum potassium level 5.5 mmol/L or higher). These diuretics should be prescribed with great caution to patients at increased risk of developing hyperkalemia, such as patients with concomitant kidney disease, diabetes mellitus, elderly patients, or those receiving ACE inhibitors. During pregnancy, the use of spironolactone, which has antitestosterone activity, is contraindicated. In the treatment of hypertension, potassium-sparing diuretics are usually taken 1 or 2 times a day (morning and afternoon) together with thiazide or loop diuretics. International names of diuretics used to treat arterial hypertension, as well as their average therapeutic doses and characteristic side effects are given in Table. 2. Mechanisms of antihypertensive action of diuretics.
The hemodynamic effect of hydrochlorothiazide and chlorthalidone in patients with hypertension has been most well studied.
At the beginning of therapy with these diuretics, a decrease in blood pressure is accompanied by a decrease in the volume of circulating plasma and the volume of extracellular fluid; cardiac output decreases, while total peripheral vascular resistance may increase. After 6–8 weeks of therapy, the volume of circulating plasma normalizes, but the total peripheral vascular resistance significantly decreases; At the same time, cardiac output is normalized. Place of diuretics among other antihypertensive drugs.
Along with beta-blockers, thiazide diuretics are considered first-line antihypertensive drugs for long-term therapy in patients with hypertension. This opinion is based on the results of numerous controlled studies, which found that thiazide diuretics not only lower blood pressure, but also significantly reduce the risk of developing cardiovascular complications in patients with hypertension. Recently, V. Psaty et al. [8] published the results of a meta-analysis of 16 randomized placebo-controlled trials that assessed the antihypertensive effectiveness of thiazide and thiazide-like diuretics. A meta-analysis showed that thiazide diuretics significantly reduce the likelihood of cerebral stroke and coronary heart disease (CHD), and also reduce mortality from cardiovascular diseases in patients with hypertension (Table 3). The likelihood of developing cerebral stroke and congestive heart failure is most significantly reduced with long-term use of comparable doses of thiazide and thiazide-like diuretics (at least 50 mg of hydrochlorothiazide or chlorthalidone per day). The risk of developing coronary artery disease is significantly reduced in patients with hypertension only when using low doses of thiazide diuretics. Until recently, thiazide diuretics were not recommended for long-term monotherapy of arterial hypertension in patients with diabetes mellitus. This was based not only on the presence of diabetogenic adverse reactions with the use of thiazide and thiazide-like diuretics, but also on reports of higher mortality in diabetic patients receiving diuretics for hypertension. Thus, J. Warram et al. [9] found that overall mortality in diabetic patients was 5.1 times higher among those receiving diuretics for hypertension. Interestingly, the mortality rate of diabetic patients who did not receive antihypertensive therapy was only 1.6 times higher than that of patients with normal blood pressure. Taking into account the results of the study by J. Warram et al. [9], which included 759 patients, 80% of whom were on insulin therapy, and some other observations, the use of diuretics as monotherapy for arterial hypertension in patients with insulin-dependent diabetes mellitus (IDDM) is considered inappropriate. For the treatment of arterial hypertension in patients with IDDM, ACE inhibitors should be used primarily, if necessary in combination with calcium antagonists or diuretics [1, 3]. As for the use of thiazide diuretics for the treatment of arterial hypertension in patients with non-insulin-dependent diabetes mellitus (NIDDM), it is quite justified provided that small doses of the drugs are prescribed (no more than 25 mg of hydrochlorothiazide or chlorthalidone per day). These recommendations are based on the results of a randomized trial on the treatment of systolic hypertension in elderly patients. This study showed that the thiazide-like diuretic chlorthalidone (12.5–25 mg/day) equally reduced the likelihood of developing cardiovascular events in elderly patients with isolated systolic hypertension, regardless of the presence or absence of NIDDM. In patients with concomitant diabetes mellitus, the diuretic significantly reduced the likelihood of developing clinically significant manifestations of coronary artery disease (myocardial infarction, sudden cardiac death, etc.) than in patients without diabetes mellitus (by 56% versus 19%) [10]. Diuretics, like other effective antihypertensive drugs, can reverse the development of left ventricular hypertrophy [11]. Therefore, there is no reason to refuse the use of thiazide and thiazide-like diuretics in patients with hypertensive heart, as was recommended until recently. The glomerular filtration rate does not change or decreases during treatment with thiazide and thiazide-like diuretics, and therefore these diuretics (with the exception of indapamide) are not recommended for use as monotherapy in patients with arterial hypertension and moderately impaired renal function (glomerular filtration rate from 50 to 80 ml /min). The calcium-sparing effect of thiazide and thiazide-like diuretics makes them first-line antihypertensive drugs in patients with severe osteoporosis and nephrolithiasis (urolithiasis). As monotherapy, thiazide and thiazide-like diuretics in low doses, recommended in recent years for the treatment of hypertension, are effective in approximately 25–65% of patients with mild and moderate forms of arterial hypertension [12, 13]. As the dose of a diuretic increases, its antihypertensive effectiveness increases, but the frequency of side effects increases significantly. Therefore, if relatively low doses of thiazide diuretics (25–50 mg hydrochlorothiazide or equivalent doses of other drugs per day) are insufficiently effective, combination therapy is resorted to. It is known that diuretics potentiate the antihypertensive effect of beta-blockers, ACE inhibitors, AT1 receptor blockers, etc. (with the possible exception of calcium antagonists). Combination antihypertensive drugs are produced, which include a diuretic and a beta-blocker (atenolol + chlorthalidone), a diuretic and an ACE inhibitor (captopril + hydrochlorothiazide), a diuretic + AT1 receptor blocker (losartan + hydrochlorothiazide), etc. Combination with other antihypertensive drugs increases the antihypertensive effectiveness of thiazide and thiazide-like diuretics and reduces the risk of side effects, which are observed mainly when using high doses of diuretics. Thus, at present, thiazide (and thiazide-like) diuretics are considered first-line antihypertensive drugs, since they not only cause a significant reduction in blood pressure, but also prevent the development of cardiovascular complications in patients with hypertension.
Literature:
1. Opie ZH Drugs for the heart 4th ed. – Philadelphia, 1995. 2. Kaplan NM Clinical hypertension. 5th ed – Baltimore, 1990. 3. The sixth report of the joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Bethesda, 1997. 4. Johnston CJ. The place of diuretics in the treatment of hypertension in 1993: Can we do better? Clin and Exp Hypertension 1993; 15 (6):1239–55. 5. Kaplan NM. Diuretics: Cornerstone of antihypertensive therapy. Amer J Cardiol 1996;77(6):3B–5B. 6. Madkour H., Yadallah MM, Riveline B. et al. Ludapamide is superior to thiazide in the preservation of renal function in patients with renal insufficiency and systemic hypertension. Amer J Cardiol 1996, 77(6):23–25. 7. Achhammer J., Metz P. Low dose loop diuretics in essential hypertension. Experience with torasemide. Drugs 1991;41(suppl 3):80–91. 8. Psaty BM., Smith NZ., Siskovick DS. et al., Health outcomes associated with antihypertensive agents. A systematic review and metaanalysis. JAMA 1997;277(9):739–45. 9. Warram JH, Zaffel ZMB, Valsania P. et al. Excess mortality associated with diuretic therapy in diabetes mellitus. Arch Intern Med 1991;151(7):1350–6. 10. Curb JD, Pressel Sz, Cutler JA. et al. Effect of diuretic–based antihypertensive treatment on cardiovascular disease risk in older diabetic patients with isolated systolic hypertension. JAMA 1996;276(23):1886–92. 11. Yottdiener JS, Reda DJ, Massic BM. et al. Effect of single-drug therapy on reduction of left ventricular mass in mild to moderate hypertension. Circulation 1997;95(8):2007–14. 12. Neaton JD, Yrimm RH, Jr, Prineas RJ et al. Treatment of mild hypertension study. JAMA 1993;270(6):713–24. 13. Materson BJ, Reda DJ, Cushman WC. et al. Department of Veterans Affairs single-clung therapy of hypertension study. Amer J Hypertens 1995;8(2):189–92.