24-hour blood pressure monitoring (a training manual for doctors)
What are the indications for ABPM? How to evaluate ABPM results?
Over the past ten years, the method of 24-hour blood pressure monitoring (ABPM) has received significant development. Currently, this method has gone beyond scientific research and is increasingly being used in practical healthcare.
The purpose of this training manual is to reflect the main, most important points of practical work with ABPM systems.
- Indications for ABPM
Diagnosis of arterial hypertension (AH)
1. Borderline hypertension. 2. Identification of the “white coat” phenomenon. 3. Suspicion of symptomatic hypertension. 4. Examination of patients with hypertension in combination with coronary artery disease, heart failure, left ventricular myocardial hypertrophy, cerebrovascular diseases, carbohydrate and lipid metabolism disorders, sleep apnea syndrome. 5. Examination of young people with unfavorable heredity for hypertension.
- Diagnosis of arterial hypotension
1. Examination of patients with chronic constitutional and orthostatic hypotension. 2. Examination of patients with disorders of postural and dynamic blood pressure control. 3. Syncope.
- Control of drug intervention
1. Selection of patients for drug treatment. 2. Assessing the effectiveness and safety of pharmacotherapy. 3. Assessment of resistance to drug treatment and selection of the optimal treatment regimen in such patients. 4. Study of the individual daily rhythm of blood pressure during a chronotherapeutic regimen of drug treatment.
Table 1. Comparative characteristics of the two most common non-invasive methods of measuring blood pressure
| Method | Advantages | Flaws |
| Auscultatory | 1. Worldwide recognized as the standard for non-invasive blood pressure measurement both for diagnostic purposes and for verification of automatic blood pressure meters 2. Increased resistance to vibration and hand movements | 1. Sensitivity to external noise, accuracy of the microphone position over the artery 2. Direct contact of the cuff and microphone with the patient’s skin is required 3. Determination of blood pressure is difficult with weak Korotkoff sounds, with a pronounced “auscultatory failure” and “endless tone” |
| Oscillometric | 1. Due to its resistance to noise loads, it can be used at high noise levels 2. Blood pressure indicators are almost independent of the rotation of the cuff on the arm and depend little on its movements along the arm (if the cuff has not reached the elbow) 3. It is possible to determine blood pressure through a thin clothing fabric, which does not affect accuracy | 1. Relatively low resistance to vibration and hand movements |
Currently, there are three known methods of measuring blood pressure: invasive (direct), auscultatory and oscillometric.
Invasive (direct) method of measuring blood pressure. A needle or cannula connected by a tube to a pressure gauge is inserted directly into the artery. The main area of application is cardiac surgery. In clinical and physiological experiments, 24-hour invasive blood pressure monitoring is used. The needle inserted into the artery is flushed with heparinized saline using a microinfuser, and the pressure transducer signal is continuously recorded on magnetic tape.
Among non-invasive methods, auscultatory and oscillometric methods for measuring blood pressure are currently the most widely used.
Auscultatory method by N. S. Korotkov. Registration of blood pressure is carried out by determining Korotkoff sounds using one or more microphones located above the abrachialis.
Oscillometric method. The method is based on the fact that when blood passes during systole through a compressed section of the artery in the cuff, micropulsations of air pressure occur, by analyzing which it is possible to obtain the values of systolic, diastolic and average pressure. Oscillation analysis is carried out using special patented algorithms. Systolic pressure usually corresponds to the pressure in the cuff, at which the sharpest increase in the amplitude of oscillations occurs, average - the maximum level of oscillations, and diastolic - a sharp weakening of oscillations.
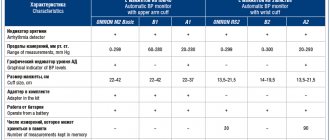
Table 2. Main characteristics of 24-hour blood pressure monitors
| Firm | , Russia | SpaceLabs Medical, USA | Meditech, Hungary | A&D, Japan |
| Model | MDP-NS-01 | 90207/ 90217 | ABPM-02/M | TM-2421 |
| SBP, mmHg Art. | 60–260 | 70–285/ 60–260 | 0-280 | 61–280 |
| DBP, mmHg Art. | 40–200 | 40–200/ 30–200 | 40–159 | |
| Wed. Blood pressure, mmHg Art. | 50–240 | 60–240/ 40–230 | ||
| Heart rate beats/min | 40–180 | 40–180 | 35-200 | |
| Method of measurement | Oscillometric or auscultatory | Oscillometric | Oscillometric | Oscillometric and auscultatory |
| Automatic measurement interval, min | From 3 to 90 | From 6 to 120 | From 1 to 60 | From 1 to 120 |
| Number of measurement periods | 2 | Up to 12 | Up to 4 | |
| Duration of one measurement, s | 30–120 | 35–50 | 30 — 120 | — |
| Number of measurements | 150 | 240 | 300 | 300 |
| Maximum pressure in the cuff, mm Hg. Art. | 300 | 300/ 285 | ||
| Storage System | Permanent action | Permanent action | Permanent action | Permanent action |
| Operational Standards | A.A.M.I., B.H.S. | AAMI, BHS, FRG | A.A.M.I., B.H.S. | A.A.M.I., B.H.S. |
| Power supply | 4 batteries or 4 NiCd AA batteries | 4/3 batteries or 4/3 NiCd AA batteries | 4 batteries or 4 NiCd AA batteries | 4 built-in NiCd batteries |
| Software; language | DOS, Windows; Russian | DOS, Windows;English | DOS, Windows; Russian | S, Windows; English |
| Weight, g | 360 without batteries | 347/255 including batteries | 350 including batteries | 390 including batteries |
| Standard monitoring duration, h | 24–48 | 24–48 | 24–48 | 24–48 |
| Cost for 1 set in US dollars | — | ~ 4500 | ~ 2800 | ~ 3825 |
| Note: the “/” sign separates the parameters of two different models of blood pressure recorders | ||||
- Equipment for non-invasive ABPM
The market for modern non-invasive automatic recorders for outpatient ABPM is quite extensive; it includes both foreign companies and domestic manufacturers. The most widespread developments in our country are those presented in Table. 2. In recent years, devices have appeared that allow bifunctional 24-hour monitoring (BP + ECG), for example, the Cardio Tens system from Meditech, Hungary. The latest achievement in daily monitoring is the multisensory system TM-2425/2025 (A&D Company, Japan), which during the day records not only blood pressure and ECG, but also ambient temperature, patient’s body position, acceleration (acceleration of the patient’s movement), and analyzes the intervalogram .
One of the most important parameters when choosing a device for ABPM is the accuracy of blood pressure measurement.
- Methodological aspects of ABPM
Preparation and installation of a blood pressure monitor. Before starting monitoring, you must make sure that the recorder's power source (batteries or accumulators) has sufficient charge to carry out ABPM. For example, the AVRM-02/M system (Meditex, Hungary) allows you to control the battery voltage on the display of the recorder when you insert power supplies into the device or when you press the orange button for a long time (10 s).
After this, the recorder is connected to a personal computer via a special cable, and the recorder is programmed (initialized) using a computer program. Programming includes information about the patient, setting periods and measurement intervals (for example: 1st period from 10 to 23 hours, interval between measurements 15 minutes; 2nd period from 23 to 7 hours, interval between measurements 30 minutes), presence or absence before each measurement of the sound signal, as well as the need for the values of systolic, diastolic blood pressure and pulse rate to appear on the display. Today, the generally accepted intervals between measurements are: for daytime - 10-15 minutes, for nighttime - 30 minutes.
| Daily blood pressure monitoring significantly expands the doctor’s capabilities both in diagnosing and treating arterial hypertension. Today there is a need for wider use of this method in practical healthcare. Apparently, in the near future, ABPM will become a standard method for examining and selecting effective therapy for patients with hypertension. |
After the recorder is initialized, it is necessary to measure the patient's upper arm circumference in order to select the correct pneumatic cuff size. According to WHO recommendations (1993), a standard cuff for adults should have an internal pneumatic chamber 13-15 cm wide, 30-35 cm long and cover at least 80% of the perimeter of the limb. For patients with an upper arm circumference greater than 32 cm, a larger cuff should be used to prevent overestimation of blood pressure values. For example, blood pressure monitoring systems from SpaceLabs Medical (USA) are equipped with cuffs of four sizes: 13-20 cm (children), 17-26 cm, 24-32 cm, 32-42 cm and 38-50 cm.
Table 3. Standards for average blood pressure values according to ABPM dataNormotonia | Hypertension | |
| Daily blood pressure, mm Hg. | <= 130/80 | > 135/85 |
| Daytime blood pressure, mm Hg. | <= 135/85 | > 140/90 |
| Night blood pressure, mm Hg. | <= 120/70 | > 125/75 |
Table 4. Critical values of the standard deviation (STD) for patients with mild and moderate hypertension (Rogoza A. N. et al.)
Day
| Night | ||
| Systolic blood pressure | 15 mmHg Art. | 15 mmHg Art. |
| Diastolic blood pressure | 14 mmHg Art. | 12 mmHg Art. |
Table 5. Methodology for calculating the SNABP
For SAD
| (average SADD – average SADD)x100% / average SADD | |
| For DBP | (average DADd - average DADd)x100% / average DADd |
| Wed SBPd - average daily SBP, avg. SBPn - average night SBP, | |
| Wed DBPd - average daily DBP, avg. DBP - average night DBP | |
Table 6. Classification of patients with hypertension according to the degree of nocturnal decrease in blood pressure (NOBP)
Group name
| English name of the group | SNABP, % | Prevalence, % | |
| Normal SBP | Dippers | 10—22 | 60—80 |
| Insufficient NSBP | Non-dippers | < 10 | Up to 25 |
| Excessive SBP | Over-dippers | > 22 | Up to 20 |
| Steady increase | Night speakers | < 0 (the indicator has a negative value) | 3-5 |
The cuff selected according to the size is applied to the left hand of “right-handers”, and to the right hand of “left-handers”. The artery mark on the cuff should coincide with the point at which the pulsation of the a.brachialis is most pronounced, usually this point is in the distal third of the shoulder. Because the cuff can move during monitoring, resulting in distorted results, we typically use 60mm diameter adhesive, double-sided discs to secure the cuff.
Control (verification) measurements. A pneumatic cuff installed on the patient's shoulder is connected simultaneously with a recorder and a mercury sphygmomanometer using a special T- or Y-shaped device. At least four consecutive measurements are taken with an interval of at least two minutes. The last three measurements are taken to calculate the average “medical” and “instrumental” blood pressure values. If the differences between these average values exceed 5 mmHg. Art. for diastolic blood pressure and/or 10 mm Hg. for systolic blood pressure, it is necessary to check the correct application of the cuff. If differences persist, the cuff is moved to the other arm or a device with a different method of determining blood pressure is used.
Patient instruction. Correct behavior of the patient during monitoring is of great importance to achieve good results with a minimum number of erroneous measurements. The purpose of the study should be explained to the patient in detail and asked to comply with the rules below.
- When measuring blood pressure, the arm with the pneumatic cuff should be extended along the body and relaxed.
- Intense physical activity and exercise are excluded on the day of blood pressure monitoring.
- If blood pressure measurement begins while walking, you need to stop, lower your arm along your body and wait until the measurement is completed.
- The patient is not allowed to look at the readings of the device, as this provokes an alarming reaction in him, which can lead to distortion of the results and neutralize the main advantage of ABPM.
- At night, the patient should sleep and not think about the work of the recorder, otherwise the values of night blood pressure will be unreliable.
- During monitoring, the patient should keep a detailed diary, which reflects his actions and well-being.
- Processing and basic principles for assessing ABPM results
All existing systems for monitoring blood pressure are usually supplied complete with a special computer program. This program allows you not only to initialize the blood pressure recorder, but also to read and automatically process monitoring results and, in addition, issue them in printed form. Below we will look at the main indicators of the daily blood pressure profile (BPAP), which today are practically universally accepted.
Average values. Calculation of average values (systolic, diastolic, mean blood pressure and pulse rate) is the most common way to evaluate the results of blood pressure monitoring. Typically, average values are calculated for the day (24 hours), day (waking period, for example, from 7 to 23 hours) and night (sleep period, for example, from 23 to 7 hours). The obtained average values give the main idea of the level of blood pressure in a particular patient and have high prognostic significance, which has been proven by numerous studies. When assessing average values obtained from blood pressure monitoring, different criteria are used than when assessing traditional blood pressure measurements. In table 3 we present standards for the average values obtained by J. Staessen et al. (1998) based on an analysis of national projects and individual studies on ABPM.
The change in average values during treatment is the most important characteristic of the effectiveness of the antihypertensive drugs used.
Frequency of increase in blood pressure (FAP) (pressure load, hypertensive load, time index) - the percentage of blood pressure measurements exceeding the level taken as the upper limit of normal (for the day - 140/90, for the night - 120/80 mm Hg. Art.) total number of registrations. This indicator has several names, reflected in the title of this section, but the most successful, in our opinion, is the name “frequency of increased blood pressure during monitoring” (V. M. Gorbunov, 1997).
The NPP indicator is closely related to the average blood pressure values. However, at high blood pressure levels, this indicator, approaching 100%, loses its information content. In such cases, PPBP is calculated as the area under the curve of blood pressure versus time, limited to 140 mmHg. Art. for systolic blood pressure and 90 mm Hg. Art. for diastolic blood pressure. The NPP indicator complements the analysis of average blood pressure values and has the same high prognostic significance. It can also be successfully used in assessing the effectiveness of antihypertensive drugs.
Blood pressure variability. Determining variability involves assessing deviations of blood pressure from the circadian rhythm curve. In the algorithms of modern systems for blood pressure monitoring, a simplified indicator is most often calculated - the standard deviation from the average blood pressure (STD) for the day, day and night periods. The critical values of this indicator for patients with mild and moderate arterial hypertension (AH) are given in Table. 4.
If a patient has an excess of at least one of the four values, then he is included in the group of people with increased variability. Increased blood pressure variability is usually associated with damage to target organs (left ventricular myocardial hypertrophy, atherosclerosis of the carotid arteries, changes in the fundus vessels, etc.).
Circadian rhythm of blood pressure (circadian index). To analyze the severity of the circadian rhythm, the degree of nocturnal blood pressure decrease (NBP) is usually calculated. In table 5 shows the methodology for calculating this indicator.
Disturbances in the circadian rhythm of blood pressure are more common in patients with impaired carbohydrate tolerance, type I and II diabetes mellitus without hypertension and with hypertension, in normotensive patients with unfavorable heredity for hypertension, in persons with symptomatic hypertension (pheochromocytoma, renal hypertension, etc.) .
According to the literature, circadian rhythm disorders with insufficient reduction in blood pressure at night are associated with a higher incidence of strokes, more frequent development of left ventricular myocardial hypertrophy, and more frequent and severe microalbuminuria. Women with insufficient blood pressure reduction at night are more likely to develop coronary artery disease and have a higher mortality rate from myocardial infarction.
All of the above ABPM parameters are used both in the diagnosis of hypertension and in the assessment of antihypertensive therapy. For example, if the average daily DBP consistently exceeds 90 mm Hg, and the RR is more than 50%, then stable hypertension can be diagnosed with confidence. With the values of these indicators being 85 mm Hg. Art. and 15-20%, respectively, we can talk about normal blood pressure. When assessing antihypertensive therapy, it is necessary to take into account the specific nature of the average values of SBP and DBP, since they reflect the results of a large number of measurements and are usually not associated with the patient’s anxiety reaction. Therefore, a decrease in average DBP values by at least 3-5 mmHg. Art. during treatment may indicate a significant antihypertensive effect.
When selecting antihypertensive therapy, it is necessary to strive to normalize blood pressure both during the day and at night. In this case, it is necessary to take into account the possibility of excessive hypotension at night in some patients. However, today there are no unambiguous criteria for assessing this condition based on ABPM data.
The prescription of antihypertensive drugs should not cause significant shifts in the ratio of daytime and nighttime blood pressure values in patients with normal SBP.
Effective antihypertensive therapy usually leads to a decrease in blood pressure variability. If, during treatment, there is a significant increase in blood pressure variability, the treatment result should be considered unsatisfactory.
When assessing the uniformity of the effect of long-acting antihypertensive drugs, which are prescribed once a day, you can use the trough/peak coefficient - the ratio of the final and peak effects (CE/PE). To calculate this coefficient, the amount of reduction in SBP or DBP relative to the initial schedule obtained before treatment is divided by the similarly calculated amount of reduction in blood pressure at the peak of the drug's effect. According to FDA recommendations (Food and Drug Administration, USA), this ratio should be at least 50%. A lower EC/PE ratio indicates an insufficient hypotensive effect of the drug at the end of the interdose interval or excessive hypotension at the peak of the drug's effect. This requires adjustment of the dose or timing of the drug.
Arterial hypertension: how to correctly measure blood pressure levels?
September 25, 2020
You have already become familiar with the causes of arterial hypertension and know what the main symptoms of this disease are.
It should be borne in mind that each patient may experience arterial hypertension differently. Thus, in some cases, so-called “white coat” hypertension is observed, i.e., elevated blood pressure numbers are detected only when blood pressure (BP) is measured by medical workers, and at home the blood pressure level does not exceed normal values. Such fluctuations in blood pressure cannot be ignored, since in the future they can contribute to the development of complications.
In most patients, blood pressure remains stably elevated - “stable” (persistent) hypertension develops.
Some patients may experience hypertensive crises - a sharp increase in blood pressure, which may be accompanied by increased headache, nausea, sometimes dizziness, and palpitations. In such cases, emergency care and medical supervision are necessary.
It is very important for all patients suffering from arterial hypertension to monitor their blood pressure levels, contact medical professionals in a timely manner, or learn to measure it themselves. Monitoring blood pressure levels is necessary for the timely detection of arterial hypertension, blood pressure fluctuations, hypertensive crises, as well as for monitoring the correctness of treatment.
Reliable results when measuring blood pressure can be obtained by observing basic rules in relation not only to the device for measuring blood pressure, but also to the patient himself and his environment. Basic measurement rules:
- Before measuring blood pressure, the patient must sit for at least 5 minutes. in a relaxed state in a comfortable chair with support on its back, legs should be relaxed and not crossed.
- The patient should not wear tight, constricting clothing.
- It is not recommended to talk while measuring blood pressure.
- Blood pressure should be measured sequentially 2-3 times at intervals of 1-2 minutes after the air is completely deflated from the cuff.
- The average of two or three measurements taken on one arm is more accurate in reflecting blood pressure than a single measurement.
- The arm with the cuff placed on the shoulder should be bare and motionless; it should be placed on a table located next to the chair.
- The middle of the cuff placed on the shoulder should be at the level of the patient's heart. Deviation from this position may lead to false blood pressure measurements (overestimation of blood pressure when the cuff is positioned below the heart level and underestimation of blood pressure when the cuff is positioned above the heart level).
- It is advisable to measure blood pressure 2 times a day at the same time (morning and evening) no less than 30 minutes later. after physical exertion, smoking, eating, drinking tea or coffee.
- It is advisable to record the results of blood pressure measurements in a personal diary (you can use a regular notebook for this) in order to then coordinate treatment with your doctor.
- The patient's environment when measuring blood pressure should be quiet and calm. The room should be warm (about 21 C), since low air temperature can cause an increase in blood pressure.
For patients suffering from arterial hypertension, it is advisable to purchase a device for measuring blood pressure (tonometer) and be able to independently monitor its level. When measuring blood pressure at home, you can estimate its value on different days in everyday life. Blood pressure can be monitored using devices with a “manual” measurement method. It is based on the method of listening to tones on the ulnar vessels (this method was proposed by N.S. Korotkov and is the most accurate). At home, semi-automatic or automatic blood pressure monitors are convenient. An important factor influencing the quality of blood pressure self-monitoring is the use of devices that meet accuracy standards. You should not purchase tonometers without documents confirming their compliance with accepted standards.
Currently, automatic devices for daily recording of blood pressure during periods of wakefulness and sleep are widely used in cardiology clinics and dispensaries. Data from 24-hour blood pressure monitoring more accurately reflect the relationship between blood pressure and changes in vital organs compared to one-time blood pressure measurements.
The use of this method makes it possible to identify the previously mentioned “white coat” hypertension at home, as well as record changes and fluctuations in blood pressure not only during the day, but also at night. Daily blood pressure monitoring helps doctors especially accurately assess the effectiveness of treatment for arterial hypertension.
A patient suffering from arterial hypertension must be aware of how this disease progresses in him, must be able to properly control blood pressure levels and, if necessary, consult a doctor in a timely manner.
Tags:
- Hypertension
- cardiovascular diseases
- Heart
- Hypertensive crisis
1 comment • To leave a comment you must be an authorized user
- katrinnns Thanks for the article! I didn’t even know that I also had to measure my blood pressure correctly! I don’t do this so often anymore, I’m on my way to recovery! Congratulate me, friends in misfortune! By the way, I recommend my product - hyperopril. And a moderately active lifestyle is an ideal remedy against all diseases!
Algorithm for studying blood pressure in peripheral arteries
1. Preparation for the procedure:
1) Introduce yourself to the patient, explain the purpose and course of the procedure.
2) Treat hands hygienically and dry.
3) Give the patient a comfortable position, sit or lay him down.
2. Performing the procedure:
1) Expose the patient's hand, placing it palm up, at the level of the heart.
2) Place the blood pressure cuff on the patient’s shoulder. Two fingers should be placed between the cuff and the surface of the shoulder (for children and adults with small arms - one finger), and its lower edge should be located 2.5 cm above the ulnar fossa.
3) Gradually inject air with the tonometer bulb until the pulse disappears (the disappearance of the pulse is recorded by the researcher by palpation). This pressure level, recorded on the tonometer scale, corresponds to systolic pressure.
4) Deflate the air from the tonometer cuff and prepare the device for re-inflation.
5) Place the stethophonendoscope membrane at the lower edge of the cuff above the projection of the brachial artery in the area of the ulnar cavity, lightly pressing it against the skin, but without making any effort.
6) After fixing the membrane, quickly inflate the cuff to a level exceeding the obtained result by 30 mmHg.
7) Maintaining the position of the stethoscope, begin to deflate the air from the cuff at a speed of 2-3 mm Hg. in a second. When the pressure is more than 200 mmHg. it is allowed to increase this indicator to 4-5 mm Hg. in a second.
 Remember the appearance of the first tone on the scale on the tonometer - this is the systolic pressure, the value of which should coincide with the estimated pressure obtained by palpation.
Remember the appearance of the first tone on the scale on the tonometer - this is the systolic pressure, the value of which should coincide with the estimated pressure obtained by palpation.
9) Mark on the scale on the tonometer the cessation of the loud last tone - this is diastolic pressure. To control the complete disappearance of sounds, continue auscultation until the pressure in the cuff decreases by 15-20 mm Hg. relative to the last tone.
3. End of the procedure
1) Inform the patient the result of blood pressure measurement.
2) Treat the phonendoscope membrane with an antiseptic or disinfectant.
3) Treat hands hygienically and dry.
4) Record the results in the appropriate medical records. If there is a change in the patient's blood pressure, inform the doctor.
Pulse research algorithm.
I. Preparation for the procedure.
1. Introduce yourself to the patient, explain the process and purpose of the pulse examination procedure. Obtain patient consent for the procedure.
2. Treat hands hygienically and dry.
3. Offer the patient or give him a comfortable position.
II. Execution of the procedure.
1. Place the first finger of the hand on the back side above the patient’s hand, and the second, third and fourth fingers along the radial artery, starting from the base of the patient’s first finger.
2. Lightly press the artery to the radial hand and feel its pulsation.
3. Take a watch with a stopwatch.
4. Count pulse waves in the artery for 1 minute.
5. Determine the intervals between pulse waves (pulse rhythm)
6. Determine pulse filling (volume of arterial blood forming a pulse wave).
7. Compress the radial artery and evaluate the pulse tension.
III. End of the procedure.
1. Register the pulse rate in the temperature sheet graphically, and in the observation sheet digitally.
2. Inform the patient about the results of the study.
3. Wash and dry your hands.
4. Treat your hands with an antiseptic.
Target blood pressure level
All patients with hypertension receiving therapy, regardless of age and risk level, are recommended to reduce blood pressure to less than 140/90 mm as the first target level. rt. Art., and with good tolerance - up to the level of 130/80 mm. rt. Art. or even lower. It is with these figures that a reduction in the risk of cardiovascular complications mentioned above has been proven. However, it must be remembered that an excessive decrease in blood pressure can be dangerous.
Your attending physician will definitely tell you about your target blood pressure level, since these numbers are individual for each patient with hypertension. During treatment, achieving the target blood pressure level allows reducing the risk of death and complications of hypertension.
Step-by-step instruction
How to measure blood pressure correctly with a mechanical tonometer:
- Take a sitting position (a sofa or armchair is suitable for this).
- Lean your back on the back of the chair, and place your feet on the floor (it is not recommended to cross them, tuck them in, throw them on top of each other, etc.).
- The left hand is freed from clothing and placed on a table or any other flat surface. The main thing is that it is not in a canopy.
- Open the cuff, insert your hand into it and secure it slightly above (2-3 cm) the elbow bend.
- Place part of the stethoscope in the form of a small metal disk on the inside of your elbow. It is important that the pulsating artery is clearly felt in this place.
- If you are performing this procedure for the first time and do not yet fully understand how to correctly measure pressure with a mechanical tonometer, then first feel the pulse with your fingers. For the future, you will know exactly where to place the metal part of the stethoscope.
- Then insert the hearing aid stethoscope into your ears.
- Make sure the air release wheel on the bulb is tightly closed.
- Place the rubber bulb of the tonometer in your hand and begin manually supplying air. The arrow on the dial will begin to move. After it reaches the 200-220 mm mark. rt. Art., stop squeezing the bulb and slowly begin to spin the wheel. The air should come out slowly, about 4 mmHg. Art. per second.
- As the air descends, you should hear a pulse. The number where the needle will be on the first beat is your systolic pressure (i.e., top). The pulse will be heard for some time. The value at which the needle will be at the last beat is your diastolic blood pressure (i.e., lower).
- Measure blood pressure on the other arm. Consider higher values as reliable. In the future, measure the pressure on the arm where it is higher.
- Both results obtained must be written down or remembered.
In general, this process will take you a few minutes. This procedure must be carried out daily, recording the data obtained. Thus, you can determine the average values of your upper and lower pressure.
How exactly is the research carried out?
Daily blood pressure monitoring is carried out using a special device. The device consists of a blood pressure cuff that is placed on the patient's arm, wires, and a small recording device that the patient wears on his belt.
The patient wears the ABPM device for 24 or 48 hours (according to the doctor's indications). Measurements are taken every 15-30 minutes during the day and every 30-60 minutes at night. The device also allows you to measure pressure at the request of the patient, for example, in case of illness. After the registration period, the device is removed and connected to a computer, the results obtained are analyzed using appropriate software and then assessed by a doctor.
With 24-hour recording, ABPM provides the treating physician with a complete record of a patient's blood pressure over a period of one or two days. The information that 24-hour blood pressure monitoring provides is fundamentally different from the information that a doctor receives when measuring a patient's blood pressure in the office. ABPM gives the most complete picture, since the results are obtained in a wide range of situations and activities: from running to sleep. Among the main advantages of the technique:
- measurements made using this method better reflect actual pressure values during normal operation, which are difficult to record during single tests;
- measurements are made outside the medical environment (hospital, clinic), which makes it possible to eliminate the associated stress, as well as to identify patients with “white coat hypertension” who do not need treatment;
- ABPM allows you to detect hidden arterial hypertension;
- The study allows a more accurate assessment of the effectiveness of the pharmacological treatment used.
ABPM does not show only one blood pressure value, which is usually regarded as the patient’s “official” blood pressure. The method reflects the entire range of frequently changing values over the course of a day or longer, and this is its key advantage.