Symptoms
The complaints of people who have suffered such an attack are similar to one another: “I sleep terribly, I suddenly wake up at night from a strong heartbeat, I can’t breathe normally, I can’t sleep, I break out in a cold sweat.” The essence of the complaints is disturbance of night sleep and a feeling of a racing pulse.
Frequent interruption of night rest, when the heart beats strongly, leads to the fact that a person gets up after sleep without a feeling of freshness, broken, and unable to concentrate during the day. Insomnia often occurs.
The somatic side of the attacks - increased heart rate - is combined with the psychological - panic attacks. They frighten a person, but since they occur at night during sleep, they take the form of disturbing or nightmare dreams. Having awakened, a person does not regard dreams, even terrible ones, as a reason for concern about health.
You can do nothing if sleep is disturbed by attacks of tachycardia only occasionally. When your heart beats at a frantic rhythm from night to night, you cannot remain careless: you cannot do without the help of a competent doctor. Ignoring the problem of a strong heartbeat is fraught with aggravation of attacks.
The following signs indicate a deterioration of the situation and the transition of night palpitations to a more severe form:
- the appearance of chest compression;
- heartache;
- feeling dizzy
- loss of consciousness.
These symptoms join existing night attacks and signal the need to see a doctor as soon as possible.
How can a doctor help with a strong heartbeat?
If you have a complaint about palpitations, you should contact a general practitioner or cardiologist.
When a patient complains of increased heartbeat, it is first necessary to establish its cause - whether it is of physiological or pathological origin. For this purpose, laboratory and instrumental studies may be prescribed, including ECG, echocardiography (ultrasound of the heart), and radiography of the heart. After identifying the cause of the increased heart rate, a course of treatment is prescribed aimed at eliminating pathological factors. Normalization of the heartbeat is achieved through treatment with antiarrhythmic drugs. Such drugs should not be taken on your own; they should be prescribed by a doctor in accordance with the condition of your body, established on the basis of a medical examination. Otherwise, the treatment result may be negative.
Types of arrhythmia
The first examination performed for any heart rhythm disturbance is an electrocardiogram. Analysis of ECG curves made it possible to divide rhythm disturbances present in patients with night-time tachycardia into several types:
- extrasystoles;
- migration of the pacemaker to the AV node;
- blockade of pathways;
- sinus arrhythmia.
Tachycardias at night, accompanied by a lack of breathing (apnea), are observed strictly in a state of sleep
Upon waking up and throughout the day, the heart continues to beat at a normal rhythm, there is no discomfort. With successful treatment of sleep apnea, nocturnal tachycardia stops.
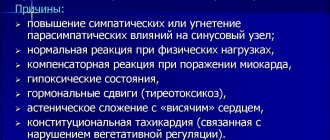
Causes of tachycardia
The transition of the body into a state of sleep is accompanied by the transfer of control from the cerebral cortex inward - to the department of the reticular formation. The active state of the retinal formation inhibits the sympathetic department and increases the tone of the parasympathetic part of the nervous system.
Parasympathetic has a multifaceted influence on all life processes. If there are hidden health deviations under parasympathetic nighttime influence, they become aggravated. This happens with nocturnal tachycardia.
Low vagal tone
The vagus nerve (nervus-vagus), part of the parasympathetic division, reduces the pulse by suppressing the activity of the sinoatrial node. For this reason, at night, a healthy person’s heart beats at a slow pace and blood pressure is reduced.
But insufficient vagal tone allows the sympathetic nerves to remain in a position of dominance. The effect of sympathy on the heart rhythm is exactly the opposite - an increase in the heart rate. The smooth muscles of the intestine are affected by the vagus nerve; in response to increased vagal tone, peristalsis (movement) of the intestinal loops increases.
Neuroses, panic attacks
Frequently observed causes of nocturnal tachycardia are prolonged stress, driven inside the consciousness, and long-standing fears. Each process that occurs in the cerebral cortex and is not completed forms a focus of pathological excitation in it with stable neural connections.
In a state of sleep, the cerebral cortex tries to remove the pathological focus - and the person dreams that he is trying to cope with repressed fear. Sometimes a dream ends with victory over fear. This means that the brain destroyed the pathological focus in the cortex.
In psychiatric practice, such dreams are referred to as “catharsis” - liberation from fears repressed into the subconscious. In a cathartic state, there is a huge release of emotions - a constant sign of getting rid of the pathological focus. Night tachycardia, along with other symptoms, is the physiological side of cleansing catharsis.
In the morning, a person does not remember why he suffered from night terrors. A similar mental defense mechanism is designated by the psychoanalytic term “repression.” The specialist’s goal is, together with the patient, to find repressed thoughts and fears and help the patient destroy them in a state of consciousness.
Nocturnal hypertension
Why does blood pressure rise at night during sleep?
Attacks of palpitations at night can be caused by a rise in blood pressure in hypertensive patients, if the effect of blood pressure-lowering drugs has ended earlier than expected.
This happens when a patient misses a dose of an antihypertensive drug or takes an insufficient dose. Regular repetition of cases when the heart is pulsating strongly, closer to the onset of morning, means that it is time to see a doctor to adjust drug therapy.
After the examination, the doctor will delve into the complex pathogenesis of the nocturnal rise in blood pressure and prescribe new doses or new antihypertensive drugs. In people suffering from hypertension, a characteristic rise in blood pressure occurs in the morning and signals the need to seek medical help!
Apnea syndrome
Suspending breathing while a person is sleeping is a common cause of an attack of nocturnal tachycardia. The most banal option: the lack of breathing is caused by obstruction of the respiratory tract - the tongue simply relaxes and closes the throat.
Breathing disappears for a few seconds - minutes. Oxygen deficiency causes activation of the respiratory center in the medulla oblongata - breathing movements become more frequent and deeper, the heart beats loudly. At the moment when the inhalation force is higher than the air resistance in the respiratory tract, snoring occurs. The sleeper wakes up from his own snoring or the REM sleep phase begins.
Snoring people not only disturb their loved ones, but also harm themselves. Because of snoring, the sequence of rapid and slow-wave sleep is confused, and as a result, the person is not able to get a good night's sleep. During apnea, the heart muscle suffers from a lack of oxygen. This is fraught with the development of angina, when there is pain in the chest area and the heart is pounding.
The state of lack of breathing at night creates stress for the cerebral cortex, which results in disturbing and nightmare dreams
At the start of apnea, the heart slows down and beats more slowly. When the period of apnea has passed and the person has woken up, breathing and heart rate increase to compensate for oxygen deprivation.
Other causes of nighttime palpitations
Types of pathology that can lead to the appearance of a strong night pulse:
- organic disease of the heart muscle, pathology of the endocrine glands (diabetes, thyrotoxicosis);
- uncontrolled use of cardiac medications, alcohol and nicotine poisoning, acute viral infections;
- reduced hemoglobin content in the blood - anemia.
The reason remains unknown? Such cases are called “idiopathic”.
Causes of physiological tachycardia
In a healthy body, the heart rate increases in many situations.
- Getting physical activity. This includes sports, physical work, muscle tension of various origins.
- A moment of emotional stress. Emotions - any - must be strong.
- Being in a threatening external environment. This is dirty air, lack of oxygen at altitude or in a stuffy room, increased ozone content in the post-storm air.
- A rise in body temperature, for example, during a cold. Surely it is angina that gives you the feeling that you are shaking. After all, there is a “10 to 1” rule: the heart rate increases by 10 beats for every rise in temperature by 1 degree.
- Overeating attacks. Excessive eating often causes an increase in heart rate.
- Allergy attack.
- Menopausal flushing of the face and upper body.
- Taking energy liquids. Heart palpitations can also increase from strong tea or coffee.
Common causes of heart palpitations
Even a healthy person can feel increased heartbeat. This is most common for people with increased nervous sensitivity. The following can lead to heart palpitations:
- significant physical effort;
- rapid rise to altitude;
- physical activity in a hot and stuffy environment (lack of oxygen leads to increased heart function);
- sharp mental stress (fear, excitement, etc.);
- consuming large amounts of foods high in caffeine (coffee, tea, Coca-Cola);
- certain medications (in particular, cold remedies);
- digestive disorders (for example, flatulence, as a result of which the diaphragm appears slightly elevated).
Palpitations may be felt when the temperature is high (patients with a fever often feel palpitations).
Diagnostic methods
The main methods for diagnosing nocturnal tachycardia are:
ECG
The main method for detecting nocturnal tachycardia is to take an ECG. Performed when you first seek medical help.
An ECG helps to study the work of the myocardium during the day and exclude the presence of daytime heart rhythm disturbances
Holter cardiogram
To document the fact of nocturnal tachycardia when a person goes to bed gives a chance to take a Holter electrocardiogram. The mobile device is attached to the patient for a day. A Holter ECG will not only detect nocturnal palpitations, but will also make it possible to determine its type and severity.
Echocardiogram
Another name is ultrasound of the heart. Allows you to “see” on the screen all the structures of the heart: chambers, valve apparatus, vessels. The functioning of the endocrine glands is checked using blood biochemistry, ultrasound of the thyroid gland, and pancreas.
Treatment
It is a common situation when cardiac pathology is the basis of the nightly “pranks” of the pulse. In this case, treatment aimed at getting rid of cardiac pathology will help. The main goal of therapy is to reduce the number of attacks and their severity. Indeed, in the presence of myocardial pathology, a violation of the rhythm of contractions gradually turns into a factor aggravating heart disease.
When the cause of night attacks is high blood pressure, the doctor prescribes antihypertensive drugs and determines the dose individual for the patient. As a rule, the evening dosage of the medication is increased. If the issue is sleep apnea, then everything is more complicated. Therapeutic measures in relation to it have a weak effect.
In all cases, doctors advise sleeping on your side. But sleeping people usually do not control the position of their own body in their sleep. For this reason, the only effective method is the use of special devices for ventilation. Such gadgets pressurize oxygen through a mask into the lungs of those sleeping.
To prevent your tongue from closing your windpipe at night, you can lose excess weight and cure ENT pathology. One hundred percent option: the doctor selects a gadget that fixes the position of the lower jaw while you sleep. Straining, changing body position, and taking a hot-cold shower will help quickly (but not for long) make tachycardia disappear.
Psychotherapy
The trigger for an increase in heart rate at night can be a mental injury, after which the patient wakes up for a long time, attacked by panic attacks. A qualified psychotherapist will help eliminate this problem. Beta-blockers and sedatives are indicated as medications.
General recommendations for nocturnal tachycardia - normalize sleep, increase the overall tone of the body
Increased heart rate and high blood pressure
Increased heart rate is often accompanied by increased blood pressure. In this case, the more often the heart contracts, the higher the pressure in the arteries. The dependence here is exactly that... Therefore, it is wrong to consider high blood pressure as the cause of increased heart rate. Another thing is that increased blood pressure, accompanied by a general deterioration in well-being, can make you notice how hard your heart is beating.
Rapid heartbeat and increased blood pressure can be caused by the same reasons. In this case, therapeutic measures aimed at normalizing blood pressure will also help normalize the heartbeat.
Signs and warning signs
Conditions when you need to pay attention to your health and immediately consult a doctor:
- the appearance of shortness of breath (I can’t breathe);
- noise in the ears, cranium;
- dizzy;
- it becomes dark in the eyes;
- there is weakness up to loss of consciousness;
- heartache.
You must immediately call an ambulance, and while waiting for it you must:
- free the patient’s neck and chest from tight clothing;
- provide air access to the patient (open the window);
- apply cold to your forehead, rinse your face with very cold water.
Prevention
To prevent attacks of nocturnal tachycardia from occurring, the best way out is to reduce the load from both physical labor and emotions, adhere to an active lifestyle that can enhance the reserve capabilities of the human body and bring the pulse back to normal.
You need to take control of the number of hours spent motionless (at the computer), remove all “nicotine poisoning sessions” from the regime, and avoid drinking 8 cups of coffee a day, especially before going to bed.
It is better to avoid heavy meals before bedtime and reduce the amount of quickly digestible carbohydrates. The body should receive almost the entire daily dose of calories in the first half of the day. Before going to bed, you should not engage in physical activity; it is better to take a walk or take a relaxing shower.
Two techniques
Aortic rupture can be prevented with surgery. Until 1995, in Russia they were made only in one way: they opened the peritoneum, cut out the deformed section of the aorta, and replaced it with a prosthesis made of durable synthetic material the size of a healthy aorta. The full course of recovery after such an operation takes 2-3 months. The success rate of treatment is 90%. Since 1991, it has become possible to perform operations using the endovascular method, that is, intravascularly. What does it look like? Incisions are made in the femoral arteries, through which surgeons insert the components of the prosthesis, packaged in a delivery device with a diameter of 7-8 mm (and the normal width of the aorta is 2 cm), and pull these parts along a path 30-40 cm long to the desired section of the abdominal aorta. And already there, inside the aorta, the prosthesis is assembled. The endoprosthesis consists of a mesh frame that supports the diameter of the vessel and a thin synthetic material that does not allow blood to pass through. All these manipulations are carried out under fluoroscopy control. Fantastic? Surgeons say: “The technique is simple.” True, endoprostheses are not produced in Russia, and they are not cheap; they are made to individual standards in the West. But there are no quotas for such gentle, non-traumatic, modern operations; the state does not pay for them. Therefore, up to 90% of operations for aortic anervism are still performed in our country using an open surgical method.