Patent ductus arteriosus: causes, treatment, prognosis
The diagnosis of patent ductus arteriosus (PDA) is often made in premature infants. What does this diagnosis mean? Why does patent ductus arteriosus occur? Is surgery always necessary? We talked about this live on “The Right to a Miracle” with Grigory Valerievich Revunenkov
, Ph.D., Head of the Department of Innovative Diagnostic Research Methods, Ultrasound Diagnostics Physician at the Research Institute of Pediatrics and Children's Health, Central Clinical Hospital of the Russian Academy of Sciences.
What is patent ductus arteriosus?
This is a defect that at one stage of the child’s intrauterine development is not a defect. This is one of the types of fetal communication: without an open ductus arteriosus (ductus arteriosus), the child does not develop in utero. Since the lungs do not participate in breathing, they are airless, high-pressure blood must be expelled somewhere. It is through this channel that it is discharged from the pulmonary trunk (which fills the lungs with blood) into the aorta - a vessel that extends from the left ventricle and is the largest vessel in our body.
However, after the baby is born, this fetal intrauterine communication must close. Why? The lungs begin to work, and as soon as the concentration of gases in the blood changes after the first inhalation, the duct contracts (this is a kind of tube of a certain length, with walls with muscle fibers). The duct contracts and blood flow through it stops quite quickly.
However, at first, when the duct is closed, the opposite situation is also possible. For some reason, the muscles may relax and the duct may resume its activity. Why is this happening? For many reasons. Including when using certain medications. These may be very premature babies. It doesn’t make much sense to list all the factors.
What then happens to the patent ductus arteriosus?
There are medications that allow the duct to close. These are non-steroidal anti-inflammatory drugs that we use in everyday life - indomethacin, ibuclin, and so on. These drugs can close the duct in a small child. But only if the muscular apparatus, which is responsible for the spasm of this vessel, works correctly.
In cases where the duct is really large, or there is a non-drug reason why the duct remains open, sometimes it is necessary to decide on the operation directly in the incubator. But for this there must be certain conditions.
How is patent ductus arteriosus diagnosed?
Using a very popular tool now - echocardiography. This is an ultrasound examination of the heart. Abroad, it is not customary for everyone to undergo echocardiography. We also. It is done under a certain situation. When a child has pulmonary insufficiency, low saturation. At an early age, patent ductus arteriosus is very well treated. The time from birth to 1-3 months is the window of opportunity when most congenital heart pathologies can be seen. And the patent ductus arteriosus at this age is clearly visible. Unlike adults.
Where do adults with PDA come from? Echocardiography began to be used so widely relatively recently, about 15 years ago. So, those adults who were underexamined at one time may have a patent ductus arteriosus. And in children, sometimes at an older age, a PDA is discovered during medical examination.
When is patent ductus arteriosus operated on?
If he's big. If it leads to a pronounced disturbance of hemodynamics, this manifests itself in the early period, and the decision is made in the first days. If for some reason this was not required, the open ductus arteriosus is small in caliber, 1-2 mm, then such ducts are not closed immediately, but are left for later, since perhaps they will close on their own, or with medication. Surgery is not always necessary.
How complex is this intervention? How difficult is it to rehabilitate a child after this intervention?
If we consider it from the category of cardiac surgery, it is considered uncomplicated; it is one of the simplest operations. If we consider simply from medical surgical interventions, there is not a single intervention about which we could say that it is not very simple. Observing this defect, if we decide that its effect on the cardiovascular system can be considered stable, that is, it is not hemodynamically significant, we usually observe the duct until preschool age.
How is the operation performed?
The duct has a rather complex structure. The outlet is the trunk of the pulmonary artery - the effect on the state of the cardiovascular system depends on it, it calibrates it. There is an ampulla - this is the wide part on the side of the aorta. And there is its length - extension. All these three parameters force us to select one or another type of device for closing.
There are many options for devices that close the duct. Flipper is an elongated string made of metal with a memory effect, which, when entering the body, curls into a complex spiral and closes the duct. There are occluders that are specially configured - they are used to close more complex ducts.
The PDA is operated on through a small incision (traditional suturing) or endovascularly, through the femoral artery: a puncture is made, an instrument is inserted that closes this duct.
What happens if you do not close the patent ductus arteriosus?
Quite often there are small open arterial ducts, with a caliber of up to 1 mm or 1 mm or less, they are not hemodynamically significant. But there is one thing. It is customary to close them not because they play such a large role in hemodynamics, but because in the future the development of botalitis is possible.
Botalitis is an inflammation of the botal duct, which can lead to certain complications. And this means thrombosis and the development of vegetation. This is the proliferation of bacterial colonies and occurs during severe bacterial infections: pneumonia of various etiologies, ENT infections, tonsillitis, periodontitis. In this case, treatment becomes quite unpleasant, because thrombosis occurs. This is no longer a simple operation to implant an occluder, but a large operation that forces us to excise the area where these vegetations have arisen, and the treatment takes on a larger scale.
That is, in those cases when we close these small ducts, we do not affect hemodynamics, but we, as it were, lay a straw for ourselves so that this difficult situation with botalitis does not arise. This is prevention.
Question from subscribers. Born at 34 weeks. Open duct 2 mm. We were monitored for up to a year and still sent for surgery. There are no other diseases. We don’t know whether we should still wait until preschool age?
We encounter this situation quite often. Each specific case must be considered separately. Sometimes children are brought in with a 3 mm patent ductus arteriosus. But we understand that there were 3 mm per month, and this is a hemodynamically significant duct. How did he get 3 mm at the age of 3-4-5? And when they deliver it, we measure it again and it turns out that they measure it in the wrong place. That is, not the part that calibrates the duct itself and influences its significance, but let’s say they measured it in the middle part. There really could be 4 or 5 mm. But the anastomosis with the pulmonary artery itself is a millimeter. Thus, this duct is hemodynamically insignificant and there is no need to rush.
The larger the caliber of the vessel through which we pass the device, the more convenient it will be not only for the operator, but also for the patient, because the vascular wall will be less injured. That's why we usually push it to 5-6 years, if possible. If it is impossible, this is a different situation, then it means we need to operate. To the point that if it is not possible to operate endovascularly, then it is necessary to use the open method. When indicated, I repeat.
What are the long-term consequences of patent ductus arteriosus? Does this manifest itself somehow in the future?
Yes, sure. One of the consequences is the development of botalitis. The second situation is when a hemodynamically significant duct is missed for some reason; this also occurs. In this case, in the future we may encounter the development of pulmonary hypertension. The excess volume of blood that will enter the pulmonary circulation will lead to an increase in pressure in it, as a result, the walls of the vessels that go to the lungs will become denser. The vessels become unable to maneuver, namely to expand or narrow. And this is the so-called pulmonary hypertension. The fourth stage of pulmonary hypertension is characterized by the fact that the person is difficult to help and is practically inoperable. Eisenmenger syndrome develops: as soon as we reduce the pressure in the pulmonary circulation, this will lead to a crisis in the pulmonary circulation. The vessels are not able to operate at a pressure lower than before. And with high blood pressure, pulmonary edema develops. Unfortunately, there is only one treatment here - a lung transplant. This is a very difficult situation.
Therefore, PDA must be observed. A month or three months of a child’s life is a window of opportunity when we can see those nuances that, for one reason or another, we will not be able to see at an older age. It’s quite difficult to watch a one-year-old child. Young children at this age are already beginning to be aware of themselves and those around them, and to make certain demands on them. They may not want to lie quietly, they will scream, struggle, and when screaming it is very difficult to explore, because the signal that we receive turns out to be so noisy that sometimes it is impossible to see anything. And at one month the children are quite calm. At least you can feed them.
What are the clinically significant dimensions of the duct?
There is no direct correlation between the diameter of the duct and the clinical situation. Depends on many factors. What period of life - newborn or later period. How mature are the child's lungs? There are a lot of factors. But if the duct is 3 mm, then it is monitored very carefully in the maternity hospital. It’s just that few people do echocardiography in the first days in the maternity hospital. Shortage of specialists, shortage of equipment. But they always call a specialist, even from another institution, if there is a clinical need. It occurs when saturation drops, when cardiopulmonary failure is diagnosed.
And so, there are different situations: at my appointment there was a girl whose diameter of the patent ductus arteriosus was 9 mm at the age of five. She had Eisenmenger syndrome and, unfortunately, we were unable to help her. There was a boy with a similar situation. But in the modern world this is casuistry and, in theory, this should not happen. With early diagnosis, children could be helped.
What are the risks of occluder placement surgery?
The risks of implanting an occluder are minimal. To do this, there must be a good diagnostician and a specialist who will install this occluder must work with it in tandem.
My son has a clip in his heart. Will anything need to be done with it in the future?
The clip is titanium and remains in the body for life. Questions arise when they are about to undergo magnetic resonance imaging. Yes, the clip is made of non-magnetic titanium material. But non-magnetic materials heat up in a high magnetic field. Therefore there are certain restrictions. In an MRI study, it is believed that if the body has various metal devices (stents, for example), one can remain in the active phase of the study for 15 minutes without harm to health.
The child has a patent ductus arteriosus, but no treatment was prescribed. We are 8 months old, born at 31 weeks weighing 1650 grams. Should I take my child to another doctor?
A second opinion is very good. But since the size of the duct was not indicated, most likely this duct is hemodynamically insignificant, and the doctor decided that it was necessary to observe. And drug treatment at this stage is not necessary. If there is even the slightest doubt, they must be resolved.
You
–
Head of the Diagnostic Research Department.
How fast is technology developing in this area? Just like computers. Development occurs in parallel. Miniaturization, complication, increase in diagnostic confidence. If earlier it was hard to see and only a diagnostician with experience could say that there should be something based on certain signs, now diagnostic confidence is greater, because it is visible better, and the angle can be more conveniently selected. Because the sensors themselves, the devices themselves, are more convenient. Experience is still important though. But in some situations, if you are not entirely sure, you can order another study.
Video
More photos Author(s):
A.N.
LAPSHIN, S.G. ATANASOVA, Yu.V. Strizhak, S.N. VERENIKINA, E.L. KEMELMAN, M.N. LAPSHIN, V.Yu. KHVEDCHUK, I.A. TYURENKOV, P.V. BELOKOPYTOV, S.K. SOBAKINA, T.V. PIMCHENKO, A.V. KLIMOVA Organization(s):
Innovative Veterinary Center of the Moscow Veterinary Academy
Journal:
No. 6-2017 UDC: 619:616.624-089
Key words :
treatment of patent ductus arteriosus, patent ductus arteriosus, endovascular treatment, PDA occlusion, PDA embolization
Key words :
patent ductus arteriosus, embolization of PDA, intervention Radiology
Abstract
Persistent ductus arteriosus is one of the most common congenital defects of the cardiovascular system in animals.
Currently, endovascular technologies are preferred in the treatment of such patients. Summary
Patent Ductus Arteriosus is 1 of the most incidental congenital vascular anomaly of the heart. Now we have excellent treatment option like endovascular occlusion or how we call in embolization of PDA. This paper is focused on different types of embolization by transarterial approach.
Introduction
Persistent ductus arteriosus is one of the most common congenital cardiovascular defects in animals (according to Schrope). Currently, endovascular technologies are preferred in the treatment of such patients. At the same time, with the increase in the number of such interventions in the world, the moment of preoperative determination of the morphology and size of the patent ductus arteriosus (PDA) has also become important. Values such as the type of P-PDA and the minimum diameter of the duct (ostria of the PDA) are often difficult in routine TT-EchoCG and are not determined by cardiologists. In view of this factor, various additional imaging techniques are used for PDA typing at the preoperative stage. The main method used for typing is TE-EchoCG, but at the moment this technique is not used in the Russian Federation. For this reason, in our practice, we use the preoperative CT-A technique with the maximum possible values for the X-ray tube rotation speed and pitch parameter for a 16-slice computed tomograph. After typing the P-PDA, the operation is planned and the access technique is selected.
Most veterinarians performing endovascular interventions for PDA prefer the transarterial approach through the femoral artery, since it is the simplest from the point of view of positioning the embolic device in the cavity of the PDA.
Patient preparation
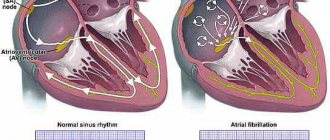
The diagnosis of PDA is established on the basis of physical examination (auscultation) and TT-EchoCG. Ultrasonography of the heart determines the direction of blood flow in the PDA (left-to-right or right-to-left shunt), determines the size of the heart chambers and valve dysfunction (mitral regurgitation). This makes it possible to determine whether it is promising to recommend a surgical treatment method to the patient or whether it is no longer possible to help him (impaired contractility of the heart chambers and/or the presence of a right-to-left shunt).
Due to the fact that the choice of treatment for the patient is entirely the responsibility of the animal owner, the doctor explains all the pros and cons of various surgical techniques. Previously, we recommended performing CTA only in cases where owners agreed to undergo endovascular treatment for their pet, but with the advent of the material by Dundie et al. about the use of 3D printing technologies in surgical planning of open operations, the possibilities of using CTA can be significantly expanded.
The main task of CT specialists when performing a study is to force the tomograph to overtake the speed of the cardiac impulse to obtain the best characterization of the morphology of the PDA. However, it is not possible to fully realize this goal on a 16-slice tomograph. At the same time, our specialists are able to perform good visualization of the PDA at the maximum scanning parameters available to the device (tube rotation 0.6 s and pitch = 1.5), for subsequent calculations of the size of the required embolic device (Fig. 1, 2).
Operation technique
Transarterial catheterization through the femoral vein is the simplest method of access due to the absence of the need for “reverse” bends of the catheter, as with transvenous access. It should be noted that transarterial access can be used in patients weighing more than 3 kg. Dissection of the right or left femoral artery is performed. A ligature is applied to the distal part of the selected section of the femoral artery, and a tourniquet is applied to the proximal part (Fig. 3). The femoral artery is punctured with a 16G catheter or dissected in the transverse direction. Next, an angiographic guide is inserted into the femoral artery to the level of the aortic arch, which is controlled fluoroscopically. An introducer or delivery device (guide catheter) is installed along the guidewire. When using a catheter, it is inserted through a guidewire to the level of the aortic arch. A first angiography is performed and the size of the PDA ampulla and striae is assessed. In our experience, the blood flow rate is so high that adequate visualization of the PDA can be difficult even in small patients and with a C-arm operating parameter of 30 frames per second. Therefore, the catheter is then pulled back, and in this movement it easily enters the cavity of the PDA. Angiography directly from the PDA cavity provides a better picture of the minimum diameter of the duct and ampulla. Next, the conductor is inserted through the ostium into the cavity of the pulmonary trunk and a catheter is passed along it (Fig. 4, 5).
Coil embolization
Traditionally, controlled coils of the Flipper family from CookMedical are used for coil embolization of PDA. The coil technique may be suitable for patients with a small PDA ampulla and a striatum no larger than 4 mm.
Two turns of the spiral are inserted through the catheter into the cavity of the pulmonary artery trunk, then the spiral is pulled to the ostium and three turns of the spiral are opened in the ampulla of the PDA (Fig. 6–8). Then a coil traction test is performed (the coil is pulled towards the aorta and then pushed into the trunk of the pulmonary artery), this allows you to determine the stability of the coil and prevents the incidence of migration of the embolic agent after implantation. At the moment of precise positioning of the spiral, we ask the anesthesiologist to place the stethoscope under sterile surgical linen at the level of the aortic arch and perform auscultation. When using an embolic coil, the auscultatory noise from the PDA fades almost immediately or becomes an order of magnitude quieter. At this moment, the cable of the delivery device is unscrewed from the helix, and the helix is released. Before removing the catheter, a control angiography is performed, which indicates either the absence of blood discharge into the pulmonary trunk, or minimal discharge (Fig. 9).
Embolization with occluder
Most often, we use a vascular plug of the second type (Amplazer Vascular Plug 2) as an occluder. The device was previously used in animals before the advent of a special veterinary occluder (Amplazer Canine Ductual occluder). An important factor in the use of VP2 is the matching of the diameters of the delivery device and the occluder.
After preparatory measures with the femoral artery (see above), the delivery device is positioned in the aortic arch and then moved caudally and thus catheterization is performed. Angiography is performed in the PDA cavity, and the minimum diameter of the duct (ostria) is also calculated (Fig. 10). Next, the catheter is passed into the lumen of the ostrium. VP2 is shaped like three connected discs, and when positioned, the first disc opens in the cavity of the pulmonary artery trunk, then traction is created on itself, and the remaining two discs open in the lumen of the PDA ampulla (Fig. 11,12). Typically, when using a technique with an occluder, the auscultatory noise from the PDA fades within the first 10 minutes, so we try not to disconnect the cable from the occluder during this time. At the same time, the anesthesiologist conducts auscultation for the attenuation of the noise; when the noise becomes unauscultable or barely audible, control angiography is performed (Fig. 13). Control angiography often does not detect a significant discharge of contrast into the pulmonary trunk. Next, a test is carried out with traction of the occluder (pulling, alternating with pushing the occluder); if the occluder is stable, the cable is disconnected (Fig. 14). Next, all catheters are removed and the femoral artery is ligated.
In the postoperative period, the patient is prescribed antibiotic therapy for 3–4 weeks and is recommended not to perform any planned operations for 3 months. This tactic was previously used to prevent the development of bacterial endocarditis, however, in the latest study by Szatmári, the hypothesis that there is no need for prophylactic antibiotic therapy in relation to the implant-dependent development of bacterial endocarditis was tested, which confirmed the absence of the need for this prevention.
conclusions
Transarterial access to PDA embolization can be considered the simplest technique, which requires minimal skills in endovascular surgery, but significant preparation before the procedure and much more attention to preoperative planning. CTA, performed in all cases of endovascular treatment of PDA, helps us reduce the possibility of complications associated with migration of the embolizing device with a slight discrepancy in the calculated sizes according to TT-EchoCG, and also eliminate the possibility of the lack of the required size in the line of consumables that is available. It is worth considering that in dogs weighing more than 3 kg, but less than 10 kg, access through the femoral artery may be difficult due to its size (the minimum size of the femoral artery that allows it to be worked with is 2.3 mm).
Note: video material dedicated to this technique can be found on youtube.com channel Dr.AntonLapshin.
The authors would like to express their gratitude to cardiologists from veterinary clinics of the Russian Federation for trusting the lives of their patients in our hands.
Literature
1. Dundie A. et al. Use of 3D printer technology to facilitate surgical correction of a complex vascular anomaly with esophageal entrapment in a dog. Journal of Veterinary Cardiology. 2021. https://dx.doi.org/10.1016/j.jvc.2016.10.003
2. Nguyenba T. Amplazer canine duct occluder: A novel device for patent ductus arteriosus occlusion.
3. Schrope DP Prevalence of congenital heart disease in 76,301 mixed-breed dog sand 57,025 mixed-breed cats. JVetCardiol. 2015;17:192–202.
4. Szatmári V. Incidence of postoperative implant-related bacterial endocarditis in dogs that underwent trans-catheter embolization of a patent ductus arteriosus without intra- and post-procedural prophylactic antibiotics. Veterinary Microbiology. 2017;207:25–28.
5. Saunders AB, Gordon SG, Boggess MM, et al. Long-term outcome in dogs with patent ductus arteriosus: 520 cases (1994–2009). J Vet Intern Med. 2014;28:401 –410.
6. Sanders RA, Olivier NB Alternative methods for the measurement of the minimal ductal diameter of a patent ductus arteriosus in a dog. Journal of Veterinary Cardiology. 2021. https://dx.doi.org/10.1016/j.jvc.2016.08.002