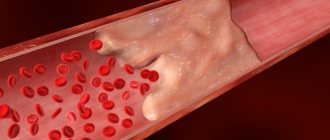
Arterial embolism is the transfer of a blood clot (embolus) from the central parts of the bloodstream through an artery, which gets stuck in some of its branches and can block or limit blood flow. Emboli typically block blood flow to an arm or leg. Embolism is a very dangerous disease, since a sudden cessation of blood flow below the site where it is stuck causes acute circulatory failure and leads to the death of an organ or part of the body.
One clot can cause more than one embolism if it breaks into pieces and is carried further down the artery by the bloodstream. Embolism requires immediate treatment, as irreversible damage to the affected organ or limb can develop in a short time.
Causes of embolism
The cause of embolism can be foreign agents of any origin that have entered the bloodstream in one way or another:
- Elements of adipose or other tissue enter the lumen of blood vessels during fractures of large tubular bones (femur, humerus, tibia), as well as after massive surgical interventions. This also includes embolism by cancer cells with the subsequent development of metastases.
- Amniotic fluid can enter the bloodstream during childbirth due to rupture of uterine vessels (fluid embolism).
- Air sometimes enters the lumen of blood vessels during injuries to large veins and arteries, during open heart surgery and during improperly performed intravenous injections (gas embolism).
- Oily forms of medications (vitamin solutions, etc.) may appear in the blood when a needle is accidentally inserted into a vessel during intramuscular injections.
- Thromboembolism occurs when a blood vessel is blocked by a blood clot formed for various reasons. Most often, thromboembolism occurs in patients with advanced varicose veins.
- Particulate embolism can occur when fragments enter the blood vessels from wounds or penetrating trauma.
- Separately, septicopyemia is considered - blockage of blood vessels by microorganisms, parasites, and protozoa. They, in turn, can enter the blood during ruptures of purulent foci (abscesses, boils, carbuncles) and during purulent melting of the walls of blood vessels located in close proximity to necrotic tissues.
Diagnosis of arterial thrombosis and arterial embolism
In our department of vascular surgery, the diagnosis of arterial thrombosis and arterial embolism is performed in accordance with the highest medical standards. Diagnostic measures include:
· collection of anamnesis and analysis of patient complaints;
· visual inspection;
· a number of laboratory tests;
· performing ultrasound examination of blood vessels;
angiography;
· computed tomography using a contrast agent.
Based on the results of the studies, the degree of the disease is determined: first degree (A, B), second degree (A, B) or third degree (A, B). After making an accurate diagnosis, our specialists decide on further treatment tactics.
Symptoms of embolism
The clinical picture is a set of symptoms characteristic of a circulation disorder in a certain area of the body. The degree of their severity depends on the size of the area that has lost blood supply, the affected organ, the speed and complexity of care. Most often, peripheral vessels, vessels of the lungs, heart, kidneys and brain are affected.
When peripheral vessels are blocked (in the arm or leg), pain in the limb, gradual discoloration of the limb, loss of sensitivity, and a sensation of “pins and needles” under the skin appear.
With pulmonary embolism, the patient complains of chest pain, general weakness, chills, shortness of breath with cough and suffocation. Due to the sudden feeling of fear, the patient has a restless appearance, eyes wide open. Next, a drop in pressure and loss of consciousness occurs. Blueness of the facial skin, rapid heartbeat and increased body temperature appear.
Impaired blood circulation in the kidneys is characterized by acute increasing pain in the lower back with irradiation to the corresponding half of the abdomen, a sharp decrease in the amount of urine, and high blood pressure. The last symptom is more pronounced when the main trunk of the renal artery is blocked; with embolism of its branches, the pressure surge is short-term and weakly manifested.
Cardiac embolism is most often caused by air and other gases entering the bloodstream. Manifested by sharp pain behind the sternum and loss of consciousness. Causes acute dysfunction of the heart and often leads to death. The same applies to cerebral embolism.
Treatment methods
Arterial thrombosis and embolism require hospital treatment , which is selected depending on the severity of the pathology.
Conservative therapy with the use of anticoagulants, angioprotectors, intra-arterial drug block and other drugs is prescribed for the first degree of the disease. Non-surgical treatment may be possible for the second degree A, but more often doctors still advise resorting to surgical removal of blood clots.
In our department, highly qualified specialists perform surgical removal of blood clots (direct and indirect thrombectomy) and perform shunt operations. If a patient experiences muscle contraction due to swelling under the fascia, a fasciotomy is indicated in addition to vascular surgery.
If we are talking about arterial thrombosis of the limb of the third degree, then it will no longer be possible to avoid the formation of a gangrenous focus. In some cases, surgery on the affected vessels can be performed to improve blood flow, which makes it possible to avoid amputation. In case of third degree B, high limb amputation is prescribed.
Embolism prevention
To avoid gas and oil embolism, you should follow the rules for carrying out invasive procedures - operations, injections, intubation procedures, etc. You can prevent septicopyemia by sanitizing foci of infections in a timely manner and refraining from independently getting rid of pustular skin processes (especially in the nasolabial area). It is impossible to reduce the risk of developing fluid, fat, and tissue embolisms by following any instructions. The likelihood of thromboembolism also cannot be calculated or prevented; however, a decrease in the percentage of complications during operations on varicose veins has been observed with a preliminary course of using anticoagulants.
Thrombotic vascular lesions
It is the most common type of embolism and can occur with the following diseases:
- varicose veins;
- heart disease (heart attack, myocarditis, etc.);
- excess body weight;
- thrombophilia.
The risk of pathology increases with a hereditary predisposition to thrombosis, after extensive surgical interventions, when taking hormonal contraceptives, and low physical activity. The most dangerous for the patient are thrombotic lesions of the great vessels of the brain, kidneys and intestines. In this case, there is a direct threat to life due to the development of tissue necrosis of vital organs. If treatment is not carried out in a timely manner, the patient's life can be saved, but he may remain disabled.
If a blood clot occludes a peripheral vessel, gangrene of the limb may develop and amputation may become necessary. Thromboembolism of peripheral arteries is easier to diagnose, which helps prevent severe complications.
Pulmonary thromboembolism is very life-threatening. A blood clot can block the main trunk of the pulmonary artery or its branch. This condition occurs suddenly, and the pathology leads to a very rapid deterioration in the patient’s well-being. He develops cardiopulmonary failure, which ends in cardiac and respiratory arrest.
The main cause of the pathology is the migration of a blood clot from the veins of the lower extremities or pelvis.
Main manifestations of fat embolism
- Arterial hypoxemia (PaO2 <60-70 mm Hg, SpO2 <90-92%);
- Signs of ARDS (usually with severe PVCs);
- Dysfunction of the central nervous system (motor restlessness, convulsions, delirium, coma). It is characteristic that after normalization of oxygenation, there is no noticeable regression of neurological symptoms;
- Petechial rashes develop 24-36 hours after injury in 30-60% of patients with PVCs. They are localized in the upper half of the body, more often in the axillary region. Hemorrhages on the oral mucosa, eye membranes and conjunctiva are also characteristic. The rash usually disappears within 24 hours;
- Sudden decrease in hemoglobin on days 2-3;
- Thrombocytopenia, or rapid decrease in platelet count, decrease in fibrinogen levels;
- Detection of neutral fat in blood, urine, cerebrospinal fluid, sputum (fat is detected in alveolar macrophages);
- Detection of fat during skin biopsy in the area of petechiae;
- Detection of retinal fatty angiopathy.
What is the danger of pulmonary embolism?
21.09.2021
Pulmonary embolism is the narrowing and occlusion of a pulmonary artery or part of its branches by embolic material. These could be, for example, blood clots. vascular obstruction occurs , leading to disruption of the blood supply to the pulmonary parenchyma.
Causes of pulmonary embolism
Pulmonary embolism most often results from deep vein thrombosis . Strong risk factors include:
- significant injuries
- cord injury
- past (major) surgical procedures
- fractures, usually in the pelvis or lower extremities
- hip or knee replacement.
Moderate risk factors are:
- chronic heart failure
- chemotherapy
- knee arthroscopy
- pregnancy and postpartum period
- history of venous thromboembolism
- thrombophilia
- paralytic stroke
- use of oral contraception
- malignant tumors
- hormone replacement therapy
The weakest risk factors for pulmonary embolism include:
- phlebeurysm _
- obesity
- old age
- undergone laparoscopic operations
- immobility for more than 3 days
From this we can conclude that pulmonary embolism can have many causes.
Pulmonary embolism - prognosis
To predict the early (in-hospital or 30-day) prognosis of patients with acute pulmonary embolism, both disease risks and the patient's clinical condition, as well as comorbidities, should be considered. If the disease is suspected, hemodynamically unstable patients with shock or hypotension should be immediately considered high-risk. They require the use of a diagnostic algorithm in emergency cases, and if embolism is confirmed, the introduction of primary pharmacological reperfusion (alternatively, surgical or interventional). Patients without shock or hypotension are not at high risk for early (poor) prognosis. About one third of patients are at low risk of early adverse events.
Correct diagnosis and treatment of pulmonary embolism reduces mortality during an acute episode by up to 3%. For massive embolism, thrombolytic treatment can reduce the risk of death or recurrence by up to 50%. Long-term prognosis depends on the cause of the disease and the effectiveness of secondary prevention. Relapse within 3 months is observed in 8% of patients. It accounted for 30% of deaths at 2-week follow-up and 50% of deaths at 3-month follow-up.
Complications of pulmonary embolism
Pulmonary embolism in its course can lead to heart failure, as well as
- bleeding
- opening of the oval window
- chronic pulmonary hypertension
Major bleeding occurs in approximately 22% of patients with pulmonary embolism receiving thrombolytic treatment, including 3% of intracranial bleeding. The incidence of these complications is lower among patients receiving heparins only. Another complication is cross embolism. Increased right atrial pressure can lead to opening of the foramen ovale, which is anatomically open in 30% of the healthy population. Then blood clots coming from the venous system, flowing through the foramen ovale, can cause embolism of the arteries of the central nervous system . Finally, it is worth mentioning chronic pulmonary hypertension of embolic etiology. In 4% of cases of pulmonary embolism, despite proper treatment, the blood clots do not dissolve, which is the cause of the development of chronic pulmonary hypertension.
Is pulmonary embolism dangerous?
Pulmonary embolism should be considered a dangerous disease. It ranks third (just behind heart attack and stroke) among modern causes of death from cardiovascular disease. It is also the most common cause of death in pregnant women. If the disease is severe, it almost always ends in death.
Published in Pulmonology Premium Clinic
Treatment and prevention of pathology
Treatment of the disease depends on its type. A treatment protocol has been developed for each type of pathology. It is aimed at normalizing vital functions and eliminating the cause that led to blockage of the vessel.
Conservative therapy includes taking medications:
- anticoagulants;
- glycosides;
- fibronolytics;
- glucocorticosteroids.
If the pathology occurs due to injury or infection, antibiotics are prescribed.
A patient with thromboembolism is prescribed ozone therapy, which eliminates the lack of oxygen in tissues and has a bactericidal effect.
If drug therapy is not effective enough, surgery is performed to remove the blood clot. To prevent thromboembolism, it is necessary to regularly monitor blood clotting parameters. There is a special analysis for this - a coagulogram. If necessary, a patient at high risk of thrombosis should take anticoagulants.
Varicose veins and heart disease are factors that provoke thrombotic damage to the arteries. If you have such diseases, it is important to monitor your condition and undergo timely treatment.
Prevention and treatment of fat embolism
In case of fat embolism, the patient needs to be hospitalized in the intensive care unit and connected to a ventilator. Drug therapy involves taking drugs that dissolve fatty particles. The patient is also prescribed anticoagulants, cardiac glycosides, and oxygen therapy.
To prevent fat embolism, it is necessary to eliminate factors that could cause lipid particles to enter the blood. In case of fractures, it is important to stop the bleeding as soon as possible, correctly fix the injured limb, monitor the patient’s condition, and control blood pressure.
Prevention and treatment of air embolism
If there are signs of pathology, the patient needs emergency care. He is fitted with a venous catheter for air aspiration and connected to an artificial respiration apparatus. To eliminate tissue hypoxia, oxygen instillations and hyperbaric oxygenation are performed.
To prevent air embolism, scuba divers must strictly follow safety rules when ascending from depth to the surface in order to prevent decompression sickness. The pathology can be caused by air entering an injured blood vessel, so it is important to promptly provide medical care to patients with such injuries and monitor their health.
When injecting drugs into a vein, it is important to follow safety requirements to avoid air bubbles entering the vessel.