Resuscitation is the restoration of body functions when they are significantly reduced with a high threat of death, as well as a return to life in case of sudden death. The goal of resuscitation is to prevent sudden death, stabilize vital functions, and, if possible, restore some of what is lost due to illness or injury.
Further treatment and recovery will take place in another, non-intensive care unit. The task of specialists in the intensive care unit (or ICU) is to prevent death from a person.
When is resuscitation required in oncology?
Resuscitation in oncology involves, if not returning a cancer patient to an absolutely normal life, then maintaining vital functions in a stable state.
In what cases is a patient taken to the intensive care unit? There are differences in the work of the oncology intensive care unit from the usual ones. In addition to typical cases of cardiopulmonary resuscitation after cardiac arrest or fatal rhythm disturbances, which also happens during a malignant process, a cancer patient is admitted to the intensive care unit:
- After extensive combined operations for common malignant processes, when the cancerous tumor and adjacent organs and tissues are removed as a single block.
- After thoracic interventions, when a change in the anatomical relationship in the chest cavity after removal of part or all of the lung with lymph nodes or a tumor conglomerate of the mediastinum directly affects the functioning of the heart.
- After removing part or all of the stomach for cancer, because the malignant process causes a catastrophic metabolic disorder that at the end of the last century led to the death of one in four of those operated on, intervention in the abdominal cavity can lead to irritation of the vagus nerve, which partly determines the heart rhythm.
- With all interventions on the brain, due to the danger of swelling and compression of the medulla oblongata, where the regulatory centers of the cardiovascular and respiratory systems are located.
- In case of severe complications of stage 4 chemotherapy, for example, in case of critical thrombopenia with the risk of spontaneous bleeding, necrotic enteritis, and so on.
- For post-chemotherapy complications of grade 3 in patients with severe concomitant diseases, when their decompensation is possible.
- When using certain immunological anticancer drugs that cause severe allergic reactions, and during high-dose chemotherapy.
- To monitor the patient’s condition after some “non-standard” methods of administering chemotherapy.
- In case of decompensation of concomitant diseases, for example, hypoglycemic or hyperglycemic coma due to diabetes mellitus, ventricular fibrillation, and so on.
- In case of breathing problems as a result of extensive metastasis to the lungs, forced mechanical ventilation is required.
- After bleeding in any organ due to the disintegration of a malignant tumor.
It is impossible to list all the clinical situations when the functioning of organs and systems becomes so insufficient to support life that emergency and active intervention by professionals is required.
Resuscitation. Can she help?
This is an excerpt from the book “Next to the Seriously Ill. Palliative care at home”, published by the Vera Hospice Charitable Foundation. It is about the difficult decision to refuse resuscitation for a dying person or, on the contrary, to support life until the very end, regardless of its quality.
A seriously ill person and his loved ones will face the question of resuscitation again and again. It’s hard to breathe, everything hurts, the pressure drops - maybe it will be easier in intensive care?
We believe that the decision to resuscitate is best made in advance, before the onset of a critical condition. In times of crisis, fear of the situation prevents you from acting in a balanced and thoughtful manner.
Resuscitation is necessary when a patient with a relatively favorable prognosis for life experiences a sudden deterioration in his condition that is not related to his underlying disease. But when a person is sick for a long time (with cancer or another serious illness), all his organs are exhausted - the condition worsens systemically and inevitably. These changes cannot be reversed through resuscitation efforts. We often hear that a dying person was refused to be hospitalized in the intensive care unit because the doctors were cruel and did not want to get involved because it was unprofitable...
In fact, refusals in intensive care for palliative patients are due to the fact that there are no medical measures that could restore a person’s health and bring him to his senses.
In the terminal phase (last days and hours of life), resuscitation measures become impossible or unnecessary. In intensive care, the patient may be given a large dose of sedatives (hypnotics). Sedation is not anesthesia; it cannot relieve pain or alleviate the condition; it can only dull reactions, that is, deprive a person of the ability to signal his pain. The pain itself does not go away. What to do about the pain? Doctors can prescribe the correct pain relief regimen, but without the help of caregivers, their efforts will be ineffective.
Therefore, we want to tell you about the types of pain and methods of dealing with it. Vera Foundation Pain relief
In the intensive care unit, the patient may be connected to a ventilator. But in the last days and hours of life this will not be a relief, because the patient is endlessly exhausted, his body is powerless, and other organs work with great difficulty. Artificial respiration becomes torture for the whole body. A ventilator means being confined to a bed and a machine, a tube in the throat and tied hands, and the inability to eat and drink normally. On mechanical ventilation, a person no longer suffers from shortness of breath, but from many other factors.
The same problems arise when trying to improve cardiac function. When the heart and body are exhausted, it is possible to “restart” cardiac activity mechanically only for a few hours or days. And the patient will spend this time in a very serious general condition.
At some point, the disease takes such hold of the human body that doctors are unable to cope with it, even in the intensive care unit.
Medicine at this stage is not able to change the number of days remaining for a person. What becomes much more important for the patient is not treatment, but peace and support from loved ones. In intensive care patients often do not have this opportunity.
According to the law (Articles 14 and 79 of the Federal Law “On the Fundamentals of Protecting the Health of Citizens in the Russian Federation”), relatives must be allowed into the intensive care unit, but the procedure for such visits (including the schedule) is established by the regional executive authority. In Moscow, Order No. 451 of the Moscow Department of Health dated June 29, 2018 “On organizing visits to patients in the intensive care unit” was adopted, establishing round-the-clock admission of relatives of patients to the intensive care unit, but such orders are not available in all constituent entities of the Russian Federation and cases are not uncommon when loved ones are denied visitation.
In a hospice, in the last hours of life, loved ones have the opportunity to simply be nearby, to hold the hand of the departing person. These last hours of life spent together are more important to the patient and his family than a few lonely days in intensive care.
Caring for a person at the end of life How to better understand your loved one and their needs in the last days and hours of life Vera Foundation
End of life
NOTE!
According to the legislation of the Russian Federation, a doctor has the right not to carry out resuscitation “in a state of clinical death of a person (stopping the vital functions of the body [circulation and respiration] of a potentially reversible nature in the absence of signs of brain death) against the background of progression of reliably established incurable diseases or incurable consequences of acute injury , incompatible with life." “Reliably established” means confirmed by the conclusion of a council of doctors.
If you want to consult about receiving palliative care, do not know what decision to make and where to turn in connection with the condition of a loved one, call the Helpline for Terminally Ill People: 8 (24 hours a day, free).
You may also be interested in our instructions on access to intensive care for a patient over 18 years of age, as well as for a child.
For a detailed article about the rights of the patient and his legal representative - including the right to refuse resuscitation, the right to know your diagnosis, and have access to medical records - read the link.
The material was prepared using a grant from the President of the Russian Federation provided by the Presidential Grants Foundation.
Stock image used from Depositphotos.
What do they do with a patient in intensive care?
They do everything that can stop the fatal decline in body functions, mainly these are multi-liter and many-hour droppers with various medications. In some situations, a subclavian catheter is installed, which allows not only to administer large volumes of fluid, but also to determine central venous pressure and take blood for analysis at any time. In some cases, for all manipulations, it is sufficient to place a catheter in the peripheral - ulnar vein.
In some cases, it is necessary to maintain adequate breathing with a ventilator, then a special tube is inserted into the trachea, and the patient is put into medicated sleep.
After operations on the gastrointestinal tract, a probe is installed through the nose, through which wound exudate and digestive juices produced in excess are removed.
After surgical interventions on the organs of the urinary system, a catheter can be installed in the urethra for better tissue restoration.
Each intensive care patient is connected to a monitor that informs about the respiratory and heart rate, blood pressure and oxygen concentration in the blood at the current time. At certain intervals, blood is drawn for tests.
In addition to medical procedures and infusions, the patient is given hygienic measures - treatment of the skin and mucous membranes, the “toilet” of the wound is performed - dressing, and of course, timely emptying of the bladder and intestines is monitored.
The order of the Ministry of Health requires turning the patient over in bed every 2 hours to prevent ischemia of soft tissues as a result of their compression by body weight, which threatens the development of bedsores. Bedsores are dead tissue and not only a source of toxic decay products, but also a gateway to infection. Intensive care staff often do not have the time to regularly turn patients over, nor the strength to shift large immobilized bodies, so modern intensive care units must have special anti-decubitus beds or functional beds that facilitate patient care.
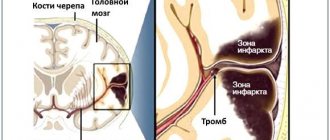
What is myocardial infarction
Acute myocardial infarction is damage to the heart muscle due to blockage of one of the arteries of the heart - thrombosis. Thrombosis leads to cessation of blood supply and death of a section of the heart muscle, followed by replacement of connective tissue - scarring. Its signs are clearly visible on the ECG.
A heart attack is a complication of coronary heart disease (CHD), which means it does not occur out of nowhere. When complications occur, atherosclerotic plaques and cholesterol deposits form on the walls of the arteries, which are the main cause.
That is why comprehensive rehabilitation in combination with secondary prevention of heart disease, based on the fight against risk factors and practical lifestyle correction, contributes to reducing mortality.
Can relatives not be allowed into intensive care?
The public has achieved the official right to have relatives visit a patient in intensive care, but the Ministry of Health has not yet prepared standard all-Russian rules for admission to the department, so at present everything depends on the attitude of the administration of the medical institution to this issue.
Many employees of public hospitals speak out against visiting the intensive care unit, as if relatives “bring the infection” and interfere with work, this is partly true, especially since an unconscious patient does not need the presence of relatives. Relatives are afraid that without their vigilant supervision, the patient may do something wrong or even harm. This, of course, is not true: intensive care unit staff are extremely interested in the patient’s speedy recovery and transfer to another department.
In private clinics, relatives are allowed into the ICU, at the same time showing sympathy for the misfortune and demonstrating therapeutic activity in the fight for the life and health of the cancer patient.
When can relatives not be allowed into intensive care?
Relatives are not allowed in if there is a threat to the health of an intensive care patient, that is, with signs of an infectious disease, including a runny nose. The ICU patient is weak and it is extremely difficult for his body to resist infection.
Children are not allowed and there are enough reasons for that. Firstly, a child with an infection does not realize that he is not healthy, especially since his activity decreases little even at high temperatures, so parents may not notice the onset of the disease. Secondly, he may touch tubes and medical devices with his hands, run or move awkwardly, disrupting the operation of equipment and disturbing personnel. Thirdly, children take death lightly, but the shock of what they see in the hospital will disrupt the child’s psychological comfort for a long time.
When performing medical manipulations and procedures, relatives are also not needed, it is unpleasant for them to see it, and the staff feels psychological pressure.
The presence of several relatives in the intensive care unit is excessive; one or two close people for a short time is quite enough to maintain the spirit of a cancer patient; do not forget that it is hard for him, he gets tired very quickly. Sitting all night long is not good for anyone, healthy people are exhausted, and the patient is simply not aware of round-the-clock vigil at the bedside.
Duration of sick leave for myocardial infarction
After discharge, the patient is given a sick leave, which is drawn up by the attending physician. If it is necessary to extend its validity, a special medical commission is appointed. The specific duration of sick leave for incapacity for work after a heart attack depends on the severity of the pathology:
- small focal infarction without complications – 60 days;
- extensive large-focal and transmural – 60-90 days;
- complicated heart attack – 3-4 months.
If the following conditions are present, the patient is referred to a medical and rehabilitation expert commission to determine the fact of permanent disability:
- repeated (recurrent) heart attack;
- the presence of severe heart rhythm disturbances;
- chronic heart failure.
The commission determines the severity of the patient's condition and assigns him to one of the functional classes. Depending on the class, doctors decide the future fate of the patient - extend his sick leave, or give him a disability group.
There are four functional classes:
- I – ability to work is preserved, but patients are removed from night shifts, additional workloads, and business trips. In this case, it is recommended to change heavy physical work to lighter work;
- II – only light work is allowed, without significant physical exertion;
- III – patients are recognized as disabled if their activities are associated with physical work or psycho-emotional stress;
- IV – patients are considered absolutely unable to work, they are given a disability group.
Further rehabilitation
A heart attack is not a diagnosis, but a way of life. After the patient leaves the hospital bed, he will have a long period of rehabilitation, during which he will restore his health and performance.
A specific program is prescribed by a cardiologist and physiotherapist. In addition to drug therapy, it includes:
- Spa treatment;
- physical therapy – in accordance with the functional class of the disease;
- dieting and weight control - avoidance of flour and fatty foods, split meals;
- quitting smoking and alcohol, which can significantly reduce the risk of relapse;
- avoiding stress, including psychological training or meditation;
- constant independent monitoring of blood pressure and pulse.
It is also necessary to periodically undergo preventive examinations according to the following scheme:
- first month - every week;
- the first six months - once every two weeks;
- the next six months - once a month;
- in the future – once a quarter.
How should a relative behave in intensive care?
- You must be in clean clothes, a medical gown, clean hands, shoe covers on your feet, and a mask on your face.
- Perfume odors are irritating, since in a serious condition the sense of smell changes; you should not perfume yourself on this day.
- Phone beeps must be turned off, or better yet, all gadgets must be turned off. Maintaining silence is mandatory; loud sounds disturb staff and cause stress in patients.
- Without the permission of the staff, you cannot perform any actions with the patient: turn over, sit up, put on your feet, take you to the toilet, change clothes, and so on.
- You cannot feed - the patient receives a specific and, as a rule, very strict diet or is generally on intravenous nutrition.
- You should not give medications, homemade decoctions, pharmacy tinctures, dietary supplements and nutritional supplements previously prescribed for chronic diseases. Biological supplements may not be compatible with the medications the patient is receiving. Everything must be agreed with the attending physician.
A sick person and a patient in the intensive care unit are two very different things; some cannot recognize their loved one, his appearance changes so much. Not only because of the tubes and wires, but the tissues swell, the eyes become sunken, and the unconscious state changes facial features. Many are shocked by what they see; one must be prepared for an unpleasant experience or not enter the intensive care unit.
In the Euroonko intensive care unit they always help patients and support the spirit of relatives. We know what needs to be done and when, you can be confident in us. We do not guarantee immortality, but we help to live without suffering.
Book a consultation 24 hours a day
+7+7+78
Bibliography
- Clinical recommendations. Anesthesiology and resuscitation / ed. Zabolotskikh I.B., Shifmana E.M. - M.: GEOTAR-Media, 2016.
- Moroz V.V., Bobrinskaya I.G., Vasiliev V.Yu. and others/Cardiopulmonary resuscitation// M.: FNKTs RR, MGMSU, NIIOR, 2017.
- Order of the Ministry of Health of the Russian Federation dated November 15, 2012 N 915n “On approval of the Procedure for providing medical care to the population in the field of oncology”
- Order of the Ministry of Health of the Russian Federation dated July 4, 2017 No. 379n “On amendments to the Procedure for providing medical care to the population in the field of oncology, approved by order of the Ministry of Health of the Russian Federation dated November 15, 2012 No. 915n”
What kind of care is provided to a patient in intensive care?
A patient diagnosed by an ambulance with acute coronary syndrome is immediately taken to the intensive care unit.
Often, large cardiology clinics have separate specialized infarction intensive care units. Resuscitation during a heart attack primarily consists of providing the damaged heart muscle with oxygen, stopping the developed life-threatening arrhythmias, and correcting hemodynamic disorders and thrombus formation.
To do this, the following procedures are used:
- oxygen therapy - the patient is connected to a ventilator to combat hypoxia;
- infusion therapy - indicated to restore normal blood supply to tissues, water and electrolyte balance, and is used to provide parenteral (intravenous) nutrition;
- sedation – during a heart attack it is very important to calm the patient’s nervous system, for which appropriate medications are used;
- pain relief – ischemia of the heart muscle is accompanied by intense pain, which can lead to the development of shock, so it is relieved with the help of narcotic analgesics;
- prevention of thrombus formation or dissolution of a formed thrombus - it is very important to prevent a recurrent attack or to ensure access of oxygen to the ischemic area, for which anticoagulants such as heparin or warfarin are prescribed;
- strict bed rest is necessary to minimize physical activity and restore the body.
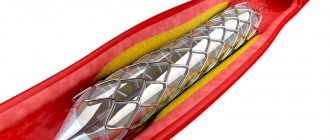
While in intensive care, the patient can be treated surgically:
stenting of coronary arteries;- coronary artery bypass grafting;
- laser angioplasty;
- balloon dilatation of coronary vessels.
Patients are in intensive care after a heart attack under constant supervision of medical personnel. They are connected to equipment around the clock, which automatically takes an ECG, monitors blood pressure, respiration, heartbeat and other indicators. If the patient develops clinical death, he is urgently given cardiopulmonary resuscitation, which consists of the following actions:
- indirect cardiac massage;
- artificial ventilation;
- defibrillation;
- drug support for the patient.