Myocardial infarction is a dangerous disease in which the blood supply to the body is disrupted, which leads to the development of tissue necrosis. Official statistics show that in 40% of cases the cause of death is a heart attack.
Thanks to the capabilities of medicine, in most cases the patient can be saved. But he will need to undergo a long course of rehabilitation to restore his functionality and return to a full life.
It is impossible to say exactly how long the recovery process after a heart attack will take, since its duration depends on the severity of the patient’s condition. With a small-focal uncomplicated heart attack, it is possible to return to your previous life within six months. With an extensive heart attack with large areas of necrosis, accompanied by complications, recovery may take 1-2 years.
Rehabilitation after myocardial infarction
Rehabilitation after myocardial infarction (MI) is a whole program for restoring health after a cardiovascular event.
Rehabilitation measures should begin from the moment a patient with a heart attack is admitted to the hospital. Each stage has its own tasks, but they all serve the same goal - to quickly and efficiently restore all functions affected by the disease. This is especially true for the functioning of the circulatory system, restoration of physical activity and ability to work. The most important principles are consistency and continuity. For each patient, a unique set of rehabilitation measures is developed. The timing and intensity of rehabilitation after a heart attack depend on the speed and quality of first aid, the severity of the disease, the condition of the body, the presence of concomitant diseases, severity class, characteristics of professional activity and other factors. Thus, patients with mild MI and low cardiovascular risk can undergo an accelerated program in 7-10 days (including early discharge within 3-5 days), and with a large heart attack and a high risk of complications, the time period can increase to 28-30 days or more.
Treatment and observation in hospital
Hospitalization is the first step towards recovery after myocardial infarction.
The inpatient stage lasts from 1 to 3 weeks, during this period the patient receives the following medical care:
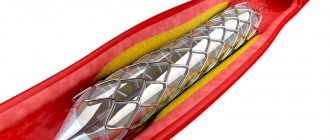
- surgical treatment - stenting in case of severe damage to the vessel walls;
- drug treatment - with the help of drugs, pain syndromes are eliminated, the load on the heart is reduced and the formation of new blood clots is prevented;
- feasible physical activity - the ability to sit, turn on the bed and wash is restored, light gymnastics and walks are allowed.
At this stage, careful attention from a strong medical team and constant monitoring of the patients' vital signs are of great importance. This is what helps to prescribe the correct treatment in a timely manner.
Stages of rehabilitation1
All stages are carried out under the supervision of specialists, starting from the resuscitation team in the intensive care unit (ICU) and ending with a cardiologist in the clinic.
Stage 1.
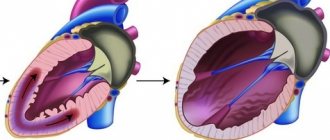
Inpatient – begins from the moment of admission to the hospital (cardiac intensive care unit, ICU, cardiology department). Main activities: diagnosis, treatment after restoration of patency of the coronary vessels, assessment of the prognosis and risk of complications of MI.
Stage 2.
Inpatient rehabilitation – takes up the entire acute period of MI (up to 28 days) after the patient is transferred to a specialized rehabilitation or heart attack department, and then to a cardiological sanatorium. This is where more intense physical activity becomes possible.
Stage 3.
Outpatient – carried out in a clinic and at home under the supervision of a cardiologist and a physical therapist. The prevention of recurrent heart attack, coronary heart disease, and treatment of atherosclerosis comes to the fore. Dispensary observation continues for a year or longer.
The division into stages is determined, among other things, by the periods of the disease:
- The most acute period is up to 6 hours,
- Acute MI – up to 7 days after the attack,
- Scarring stage – up to 28 days,
- The stage of a formed scar is from 29 days after the attack.
Rehabilitation covers all aspects of the patient’s health: physical, psychological, social. It includes drug and non-drug treatment methods, such as physiotherapy, lifestyle and diet adjustments, gradual return to physical activity and psychological support.
The effectiveness of rehabilitation affects the survival of patients after MI and quality of life.
Normal physical activity (acceptable load)
| Type of activity | Function class | |||
| I | II | III | IV | |
| Run | ++ | + | — | — |
| Walking: Fast (130 steps/min) Medium (100/120 steps/min) Slow (<= 80-90 steps/min) | +++ +++ +++ | ++ +++ +++ | — ++ +++ | — — — |
| Climbing stairs (floors) | 5 or more | up to 5 | 2-3 floors | — |
| Carrying heavy loads (kg) | 15-16 | 8-10 | 3 | — |
| Having sex | +++ | ++ | + | — |
Physical rehabilitation
At all stages of recovery after myocardial infarction, increasing physical activity is one of the most important components. Of course, certain restrictions make it possible to reduce the load on the myocardium, reduce its oxygen requirements and create conditions for speedy healing. However, unreasonable prolongation of strict bed rest can increase the risk of thromboembolic complications, contributes to the development of congestive pneumonia, disrupts the functioning of the digestive system and leads to muscle weakness. All this affects the terms of rehabilitation and reduces the quality of life.
At the inpatient stage, after acute pain has been relieved and early complications have been dealt with, the severity of the MI is determined. The depth, localization and extent of the heart muscle lesion, the severity of heart failure and the presence of complications are taken into account. It is this indicator that influences what kind of rehabilitation program will be offered to the patient.
Subsequently, depending on the dynamics and performance of the cardiovascular system, the patient is transferred from one level of activity to another. The level of blood pressure, electrocardiogram data, the presence of arrhythmia, as well as individual exercise tolerance are assessed.
Types of rehabilitation
The attending physician individually selects a rehabilitation program, taking into account the severity of heart failure, the severity of the condition, the presence of complications and other diseases, the nature of the heart attack, the age and physical fitness of the patient.
There are several types of rehabilitation:
- Medication;
- Physical;
- Psychological.
Drug rehabilitation
People who have had a heart attack must take medications.
In some cases, in addition to medication, surgical treatment may be necessary - stenting or coronary artery bypass grafting.
At the post-hospital and maintenance stages, the attending physician prescribes medications individually, taking into account the characteristics of the body, concomitant diseases, and the causes of thrombus formation. Regular monitoring of the condition is very important, which will allow the treatment to be adjusted at the slightest deterioration.
Physical rehabilitation
Particular attention is paid to the restoration of physical skills. This process must take place gradually. In the hospital, the patient relearns how to turn over in bed and sit, wash his face and brush his teeth. After some time, he begins to perform the simplest exercises and move around the ward. At the next stage, he is allowed to walk along the hospital corridor and then go up and down the steps.
In the post-stationary period, the loads are gradually increased.
Physical activity should include:
- Domestic activity - housework, gardening and gardening (hard work and heavy lifting are strictly contraindicated);
- Physiotherapy exercises – the doctor selects a set of exercises individually;
- Measured walking (terrenkur) - regular (walking) and Scandinavian, as well as going up and down the stairs;
- Cardio exercises (exercise bikes, treadmills, walking simulators, stair climbing simulators, skiing, rowing);
- Aerobic exercise (jogging, skiing, cycling, swimming, yoga).
At first, it is enough to practice every day for a quarter of an hour. Every week the duration of the classes is increased by five minutes until they reach an hour. You need to know that in the absence of physical activity, the likelihood of another heart attack increases by 25%. But you shouldn’t put too much stress on your body, which can also trigger a heart attack. Loads must be dosed and correspond to the person’s capabilities.
Mental rehabilitation
In the first month, you should pay increased attention to the psychological state of a person who has had a heart attack. It is at this stage that he especially acutely feels his helplessness, begins to realize the consequences of the disease, and experiences fear of a new attack. Therefore, the patient becomes nervous and irritable, and may show aggression, which often becomes the cause of depression or neurosis. In this case, you will need the help of a psychologist. A specialist will help you accept the situation and get rid of negative thoughts, tune in to the positive and believe that a normal life is possible even after a heart attack, and teach you how to control your emotions. Positive thinking will significantly speed up your recovery.
What is included in the post-infarction rehabilitation program
In addition to drug treatment, restoration of physical performance and stabilization of the psychological state, the rehabilitation program involves following a diet and maintaining a healthy lifestyle.
Diet
A properly formulated diet will not only help restore the body after a serious illness, but also prevent relapse. In the first days, the patient is given small portions to reduce the load on the heart. The menu consists of soups and vegetable purees without adding salt or spices.
In the future, you will have to follow the principles of rational nutrition:
- Eat often, but little by little;
- Avoid unhealthy foods (fried and fatty foods, spicy foods, sauces, smoked meats, spices, pickles, canned food, sweets, fast foods, processed foods, coffee);
- Increase consumption of seafood, vegetables and fruits, fish, lean meat, dairy products;
- Drink no more than one and a half liters of liquid per day.
If you are overweight, you need to lose weight. To do this, you should reduce the caloric content of food. Under no circumstances should you “go on” a strict diet.
Lifestyle
To prevent a second attack, you will have to “forget” about bad habits: quit smoking and stop drinking alcoholic beverages. It is also necessary to fully rest and sleep for at least 8 hours, refuse to visit the steam room, bathhouse and sauna, learn to avoid stress and dose physical activity, formulate the correct life guidelines, remain calm and emotionally stable.
Regular preventive examinations with a cardiologist, laboratory tests, ultrasound, ECG and stress tests are required, which will allow timely detection and prevention of possible complications.
Stages and approximate terms of physical rehabilitation:
I. On the first day after hospitalization, strict bed rest is most often prescribed, which is expanded from the second day and supplemented with therapeutic exercises, consisting of individually selected exercises. Gradually, the patient can increase the time he can sit, stand, and later walk around the ward. Usually, after 7-18 days, walks of up to 2-3 km at a slow pace and exercise on an exercise bike are allowed.
At the end of the stage, the level of cardiovascular risk is calculated. To do this, a repeat electrocardiographic examination is carried out, the severity of atherosclerotic changes is determined, and the heart’s abilities are assessed using echocardiography (ultrasound examination of the heart).
II. After transfer to a rehabilitation department or sanatorium, tests with physical activity are carried out. Based on their results, the optimal physical activity and its type are selected. They also take into account methods for restoring blood flow in the coronary arteries, the speed of development of various stages of activity at the previous stage, and the general condition.
The complex of physical therapy (physical therapy) gradually includes walking at a faster pace, swimming, and training on exercise machines.
III. At the outpatient stage, the determining factor is the functional class of coronary heart disease (CHD), which is determined using a study that evaluates the increase in oxygen consumption during physical activity (bicycle ergometry, treadmill test - walking on a “treadmill”). This test reflects not only the functioning of the cardiovascular system, but also the respiratory system.
Depending on the functional class of IHD, physical therapy is carried out in a training or gentle mode.
Studies have shown that the longer physical rehabilitation is carried out, the better the long-term results - the risk of recurrent MI and death is reduced to a greater extent.
Magazine "PARTNER"
“Partner” No. 8 (227) 2021
Matters of the heart
Dr. Olga Grishchenko (Heppenheim)
Recovery after myocardial infarction
In Germany, people who have suffered a myocardial infarction, after treatment in a clinic, usually receive a referral to a resort, where, under the supervision of specialists, they recover from the illness. But both those who recovered at the resort and those who have not been to the resort will find the following information useful.
Do not rush to turn the page, as this material is intended not only for those who, unfortunately, have already experienced the manifestations of coronary heart disease (CHD), but also for all young people, full of health and strength, who have not yet thought about how to maintain your health and well-being.
Unfortunately, without wanting it ourselves, we often create numerous problems for our heart, sometimes putting it in unbearable conditions. The rhythm of modern life with constant stress, an excess of negative information, poor ecology, a sedentary lifestyle and poor nutrition often turn out to be serious tests for the entire cardiovascular system, which was originally designed for healthy and active activity in a good environment and has not changed since our times distant ancestors.
Did you know that according to official statistics, heart disease claims more than six million lives every year in the world? According to the conclusion of the World Health Organization, the incidence of coronary heart disease (CHD) and myocardial infarction (MI) has long assumed the character of a kind of epidemic. In addition, myocardial infarction and atherosclerosis have become significantly younger. Nowadays, MI is not uncommon for people aged 30 years, but for those who are 40-50 years old, it has become commonplace, which makes the problem under consideration especially acute and relevant.
Of course, practical medicine has made significant progress in the treatment of MI; The best specialists and the most advanced achievements of mankind are involved in the fight against the “number one killer” in the world, but the prevention of cardiovascular diseases, unfortunately, does not always achieve the desired results. Most often, a person learns how to deal with a heart attack too late, having already become a victim, and hopes, first of all, for the help of modern medicine. Well, this is quite natural!
“No matter how skillful the specialists are who treat you and help you recover at the resorts, there comes a moment when you yourself become the master of your health, and it is up to you whether you will return to a full life and work or whether you will remain helpless and sick.”
A heart attack is successfully treated only if the patient is not passive and actively helps the doctor in the fight against the disease. A calm, good mood, positive emotional tone, like magical “living water,” contribute to the rapid healing of damaged heart muscles and normalization of its functioning. A person who has suffered a myocardial infarction should not “go into illness” (although this is sometimes very difficult, especially at first). It is necessary to tune in to a favorable outcome, knowing, however, that healing of the damaged myocardium will require a long time (3-4 months) and a certain regimen that must be strictly and consistently followed.
Diet
The success of treatment largely depends on whether you follow the recommended diet. The purpose of the diet after a heart attack is to create gentle conditions for the cardiovascular system, strengthen the myocardium, and activate the process of removing nitrogenous waste and under-oxidized metabolic products from the body. It is recommended to eat at least four times a day, in small portions, the last meal should be no later than 2-3 hours before bedtime; in the evening it is better to drink a glass of low-fat yogurt or juice. It is advisable to exclude hot seasonings, smoked foods, strong tea and coffee, which excite the nervous system and provoke vascular spasms, as well as foods rich in cholesterol.
In addition, it is necessary to limit the amount of free liquid (1.2-1.5 liters per day, including liquid included in dishes), reduce the consumption of table salt and mainly include foods that have a reduced calorie content due to the restriction of fat in them. Of the vitamins, ascorbic acid (vitamin C) is especially important, as well as B vitamins. Potassium salts contained in raisins, dried apricots, prunes, and potatoes have a beneficial effect on myocardial contractility, dilate blood vessels and increase urine excretion. Magnesium salts (there are many of them in nuts, rose hips, soybeans, figs) - lower blood pressure, have a calming effect on the nervous system, and reduce cholesterol levels in the blood.
Physiotherapy
At the resort you will definitely do therapeutic exercises. Before you start exercising, your doctor will determine your level of physical activity. The intensity of the load will depend on this. However, there are universal rules for performing any complex of therapeutic exercises after a myocardial infarction:
1. You can exercise only if you feel well.
2. If you feel unwell, shortness of breath or pain in the heart area, the load must be reduced or stopped altogether.
3. The duration of classes should not exceed 20-30 minutes.
4. Exercises are performed without sudden movements; the load increases gradually.
5. Classes must be carried out in a ventilated room, clothing should be light and not restrict movement.
6. While performing breathing exercises, inhale smoothly, with moderate depth, through the nose. Exhalation is through the mouth; it is longer and slower than inhalation.
7. Walking on level ground is measured by distance, number of rest stops, pace, and duration of the walk.
8. Training is carried out first once a day, in the morning, then in the afternoon, at least two hours before bedtime.
9. Those who started training at the resort should definitely continue them at home.
All issues of changing the motor mode must be agreed with a doctor and specialists in therapeutic exercises.
The Importance of Self-Control
In order to correctly calculate your strength during physical activity, you need to learn self-control, the main criterion of which is your well-being. An absolute contraindication for training is pain in the heart, chest, intense shortness of breath, cold sweat, increased heart rate (more than 120 beats per minute), general fatigue, pain in the legs and joints. If such complaints appear, you should immediately stop any physical activity and inform your doctor about your condition.
Unfortunately, some people mistakenly believe that with such symptoms one should not stop exercising, but the pain should be overcome. This dangerous misconception can lead to tragic consequences.
There is another extreme, when a person who has suffered a heart attack completely immerses himself in illness and is afraid of any, even the most insignificant, physical activity. This behavior is also wrong.
It is known that an attack of angina develops when the need for oxygen consumed by the heart muscle is not met due to the inability of the coronary artery to deliver it. Physical exercises specially selected by a specialist, performed at a slow pace, as well as breathing exercises mobilize extracardiac circulatory factors, help activate the arterial and venous beds, thereby facilitating the work of the heart, improve metabolism, increasing the absorption of oxygen and nutrients by tissues, normalize the functioning of the excretory organs (kidneys, sweat glands), intestinal mucous membranes. All of the above leads not only to an increase in physical performance, but also to a significant improvement in the psychological state of the patient. Mood improves, fear of physical activity disappears, and self-confidence appears.
Universal Council of Cardiologists of the World
Step by step, a person suffering from coronary artery disease and having had a heart attack must restore his health and return to a normal lifestyle. And on this path he needs positive emotions so much! Do not forget about the well-known truth: you need to respect the whole world, starting with yourself. Give others your generosity and kindness, positive emotions and good mood. This must be done sincerely, openly, and not under duress, since violence against oneself, insincerity, even with a “plus” sign, do not give a positive therapeutic result. By “feeding” those around us with our true kindness and attention, we simultaneously restore our spiritual potential, receiving in return a charge of positive emotions. Friends and loved ones, good books and films, warm family relationships are the basis for the prevention of all cardiovascular diseases.
Psychological rehabilitation
Any disease is stressful. Urgent hospitalization, the need for long-term treatment, and sometimes surgical intervention, and a sharp restriction of activity often become the causes of quite serious mental changes. Therefore, at all stages of rehabilitation, psychological and psychotherapeutic work is carried out with the patient.
A big role in recovery is played by the patient’s attitude, attitude and support of loved ones.
It is also important to overcome the fear of physical activity and form an adequate assessment of your capabilities. Patients feel differently about their condition. There are those who are afraid to make unnecessary movements and delay rehabilitation, and those who underestimate the severity of the disease and too quickly strive to return to their usual rhythm. The doctor’s task is to give an objective assessment, explain the tasks of each stage of rehabilitation and the acceptable level of activity.
At the stage of outpatient observation, it is important to prevent the development of neurosis and depression, which occur in many patients4 and can negatively affect adaptation capabilities.
Rehabilitation at home
However, if you do not end up in a sanatorium, physical rehabilitation can and should be carried out independently. The easiest way is to walk every day. You need to choose a rhythm that is comfortable for you, slow or moderate, and go for walks at least 5 times a week for 30-60 minutes. If you feel tired or weak, sit down to rest or return home. In just a few days you will be able to walk further.
The load should not lead to the development of an attack of angina pectoris
or severe shortness of breath and palpitations, only mild shortness of breath is acceptable.
Monitor your pulse;
during exercise, your heart rate should definitely increase. At the first stage, achieve a small increase of 20-30% (for example, 15-20 beats per minute). In the future, if you have good exercise tolerance, continue to monitor your pulse and do not allow the value to exceed 200 - your age (for example, you are 56 years old: it is not advisable for your pulse to exceed 200-56 = 144).
According to the recommendations of Russia’s leading specialist in the rehabilitation of patients with heart disease, Professor D.M. Aronova, depending on the severity of angina manifestations (functional class), there are different acceptable types and volumes of physical activity.
Below are tables developed by prof. D.M. Aronov, by which you can determine the physical activity possible for you. We remind you that angina is divided into 4 functional classes, I f.k - the mildest, when angina attacks develop only during high-intensity loads, IV f.k. the most severe - an attack can develop at the slightest physical exertion and even at rest. The sign (-) indicates loads that are not permitted. (+) – activity is allowed, the number (+) reflects the volume or intensity of the load performed.
Non-drug methods of prevention
After myocardial infarction, atherosclerosis, which most often causes vascular accidents, continues to develop. To prevent its progression and recurrent MI, it is necessary to minimize the effect of risk factors. For this purpose, non-drug and drug methods of secondary prevention of coronary heart disease (CHD) are used.
Non-drug methods, in addition to physical rehabilitation, include lifestyle correction. This concept includes:
- Complete cessation of smoking
, both active and passive. It has been proven that nicotine and other chemical compounds damage the inner lining of blood vessels (endothelium) and contribute to an increase in the level of “bad” cholesterol, that is, low-density lipoproteins. In addition, smoking leads to vasospasm and an increase in blood pressure, which can provoke new attacks of coronary artery disease. Research data has shown that quitting smoking reduces the risk of death by 36%! - Avoid or minimize alcohol consumption .
The heart primarily suffers from alcoholic drinks: tachycardia, arrhythmia appear, blood pressure increases, the toxic effect of ethanol can lead to another heart attack or sudden death. The permissible dose is 30 g per day for men and no more than 20 g for women. - Weight control and healthy eating.
It is necessary to balance the diet so as to maintain normal body weight and metabolism. Basic principles: reducing animal fats, replacing them with plant foods that do not contain cholesterol. Preference should be given to vegetables, fruits, nuts, lean meats and sea fish, and whole grain cereals. Smoked, canned, fried and salted foods are excluded. It is convenient to control your weight using your body mass index (the result of dividing your weight in kg and height in meters squared). It should be within 25-27 kg/m. In addition, the waist circumference is assessed: for men this figure should not exceed 94 cm, for women – 80 cm.
Dietary recommendations
Excess weight is one of the main factors leading to stroke. The main principles that should be followed are reducing the energy value of the diet, limiting animal fats and reducing the amount of sugar.
The post-stroke diet involves an abundance of a variety of vegetables and fruits; meals are divided into 5 or 6 meals a day. Preference should be given to low-fat fish, light fermented milk products, and vegetarian soups. It is allowed to eat cereals, cereals, wholemeal bread, potatoes and, in limited quantities, pasta.
Main groups of drugs:
1. Beta blockers
. Prescribed to almost all patients after MI, regardless of the presence or absence of heart failure. They reduce the myocardial oxygen demand and reduce the risk of sudden death, and also help to increase life expectancy.
2. Antiplatelet agents.
They prevent the formation of blood clots in blood vessels, reduce inflammation in the inner choroid, and reduce the risk of developing vascular accidents (heart attacks, strokes).
3. Statins.
They reduce the level of atherogenic cholesterol (low-density lipoprotein cholesterol - LDL-C), preventing the progression of atherosclerosis and the formation of new atherosclerotic plaques in blood vessels. It has been proven that reducing the concentration of LDL cholesterol by 1 mmol/l reduces the risk of death from coronary artery disease and its complications by 34%, as well as the need for surgical treatment.
4. Nitro drugs.
They are used if the patient continues to have angina attacks, or signs of silent ischemia are recorded on the electrocardiogram.
5. Antiarrhythmic drugs.
Prescribed if necessary for the treatment of various types of arrhythmias, which sometimes occur in patients who have had a myocardial infarction.
6. Antihypertensive drugs.
Prescribed if it is necessary to treat hypertension, usually several drugs are selected, the combination of which gives the optimal result for each patient.
Drug therapy is carried out under the supervision of a cardiologist. Before discharge, patients meet with the doctor daily, then 1-2 times a month in the first year and once every three months in the second. Periodically, you need to repeat an ECG, blood lipid test, exercise testing and other examinations as necessary.
A comprehensive rehabilitation program, subject to all principles, helps patients recover in a shorter time, improve their quality of life, and prevent recurrent heart attacks and other complications.
SARU.CLO.19.05.0797
OTHER INFORMATION
Please note that if our company (or any part thereof) is sold or placed into receivership, information we hold may be part of the assets transferred; however, such information will continue to be used solely in accordance with the terms of the Policy on the processing and protection of personal data.
For quality control or training purposes, we may monitor or keep a record of your correspondence with us.
•Policy of AstraZeneca Industries LLC in the field of processing and ensuring the security of personal data • Policy of AstraZeneca Pharmaceuticals LLC in the field of processing and ensuring security of personal data