YES. Kuzhel, G.V. Matyushin, E.Yu. Egorova, N.V. Kovaleva
State Educational Institution of Higher Professional Education "Krasnoyarsk State Medical Academy"
KGBUZ "Krasnoyarsk Regional Hospital No. 2"
A test with dosed physical activity is an ideal method of functional diagnostics, which allows us to assess the usefulness of the physiological compensatory and adaptive mechanisms of the body, and in the presence of obvious or hidden pathology, the degree of functional inferiority of the cardiorespiratory system [1]. A stress test (ST) is considered one of the types of natural provocation, which is used to diagnose various diseases, and in cases where the pathology is already known, with the help of PT it is possible to determine the degree of its severity or the compensatory capabilities of the cardiovascular system. NP is one of several types of stress testing (along with transesophageal cardiac pacing, stress echocardiography), therefore the term NP more accurately reflects the essence of the technique than the often used definition of stress test.
The main point of application of the NP is the diagnosis of coronary artery disease. The most important advantages of NP are non-invasiveness, virtually unlimited availability and low cost of the study. The importance of NP is also emphasized by the fact that this technique allows us to identify a risk group, that is, patients at risk of developing cardiovascular complications and death. It is no coincidence that the recommendations for coronary angiography under class I indicate the following indication - “criteria for a high risk of cardiovascular complications identified by non-invasive testing, regardless of the severity of angina pectoris” [5]. However, the provocative nature of the test implies the possibility of various complications, many of which can be serious.
If non-dangerous complications are not taken into account, the incidence of fatal events during NP is relatively low. Thus, mortality during NP is estimated as one case per 50 thousand examinations. However, the incidence of non-fatal myocardial infarction and ventricular tachycardia remains quite high - one case per 2,500 studies, or 0.05% [6]. In this regard, it is important to note that complications of NP include events that occurred no later than 24 hours after the stress test [1, 4].
NP is usually performed using a treadmill or bicycle ergometer (VEM). Each method has certain advantages and disadvantages.
Treadmill (treadmill)
The treadmill must be electrically powered and capable of supporting a body weight of at least 157 kg [4]. The patient's movement during the treadmill test is forced, that is, the patient adapts to the speed of the treadmill, so any confusion during the load is fraught with injury. Taking this into account, for safety reasons it is recommended to equip the walkway with additional handrails on the sides of the device.
However, patients should avoid holding onto handrails if possible, as this reduces the amount of work being done due to some reduction in body weight. It may be recommended that patients hold handrails with their fingers to maintain body balance while walking, and an emergency stop button should be accessible to the patient and staff if necessary.
In most cases, the Bruce protocol (R. Bruce) is used to perform NP on the treadmill. In individuals with low exercise tolerance, a modified Bruce technique can be used. In this case, at the beginning of the test, steps with a less intense load are added (usually with a lower angle of elevation of the track at the same speed as in the first step of the Bruce protocol). At the same time, it must be especially emphasized that ideally the time of the NP itself should not exceed 9-12 minutes, therefore the protocol for both treadmill and VEM should be selected individually.
Preparing for load testing
Before the examination, shave the skin of the chest in the area of the electrodes. The patient should eat his last meal 3 hours before the ECG (diabetics should take it with them). However, you must take drinking water with you. Subject should abstain from smoking for 4 hours. Drinking alcohol is prohibited the day before the test and on the day of the stress ECG. The test is best carried out in comfortable clothes and shoes.
You should not come for an examination at the last moment; it is better to set aside half an hour to have time to rest.
VEM
VEM.
VEM may be considered as an alternative to the treadmill test in patients with orthopedic, vascular or neurological diseases. In addition, VEM is a less expensive and more portable system for performing NP. The intensity of work performed on the VEM can be adjusted by changing the pedaling frequency and resistance. The highest O2 consumption and heart rate values are usually achieved at a pedaling speed of 50-80 rpm. For NP, two types of stationary VEMs are used: with a mechanical or electric brake.
Mechanical ergometers require the patient to strictly follow the specified cadence in order to keep the amount of work performed constant. VEMs with electric brakes are more expensive and less portable, but automatically adjust resistance as cadence changes, thus keeping the work done constant. When performing HEM, the power of the first stage is usually 25 W (150 kgm/min) or 50 W (300 kgm/min) with a subsequent increase in load by 25 W until the final result is achieved. For individuals with high load tolerance, the load can be increased by adding 50 W.
In assessing the information content of any diagnostic test, the main criteria are its sensitivity and specificity, which determine how effectively the test separates subjects with pathology from healthy individuals, that is, how well the test allows diagnosing the disease and its absence. A meta-analysis of 147 published studies, including 24,074 patients who underwent both coronary angiography and NP, showed wide variability in sensitivity and specificity with averages of 68% plus/minus 16% and 77% plus/minus 17%, respectively [3]. it is believed that treadmill and VEM have the same sensitivity and specificity.
For the clinician, the most important information is to assess the likelihood of the presence or absence of the disease. Such an estimate cannot be accurately derived from the ST segment depression score alone, so an estimate of pretest disease probability is also required to more accurately interpret NP results. Based on this, the interpretation of NP results, according to Bayes' theorem, assumes that the probability of a disease after performing a test (TP) will be a derivative of its pre-test probability.
The clinician often makes this assessment intuitively, for example when suggesting a false-positive finding of ST segment depression in a 30-year-old woman with cardialgia. Therefore, given the relatively low specificity of ST segment depression greater than/equal to 1 mm in the diagnosis of IHD, this indicator cannot be considered as an absolute criterion of the disease, but should be assessed in the context of the pre-test probability of the disease.
The pre-test probability of coronary artery disease is assessed based on medical history, age, gender and the nature of pain in the chest, as well as an objective examination and instrumental studies. Typical or definite angina makes the pretest probability of the disease so high (more than 90%) that the need for an NP to diagnose coronary artery disease virtually disappears, but the test can be performed for risk stratification purposes.
Taking into account the high prevalence of the use of both the treadmill test and VEM in healthcare institutions, we conducted a comparative assessment of the effectiveness of these methods in the diagnosis of coronary artery disease.
Indications for stress testing in cardiology
| Diagnosis of CHD in patients without a “coronary history”, especially in middle-aged people with an intermediate probability of CHD and with an interpretable ECG |
| Recurrent angina pectoris in patients with a history of coronary artery disease, previous myocardial revascularization, and having an interpretable ECG |
| Differential diagnosis of cardiac and pulmonary causes of shortness of breath during exercise and/or reduced performance* |
Assessment of prognosis in patients with:
|
Assessment of the functional state of patients with:
|
When prescribing increased physical activity and physical training to patients with:
|
Evaluation of the effectiveness of treatment of patients with:
|
Assessing the response to heart rate stress in patients with:
|
Examination of healthy individuals:
|
Note: * - conditions/diseases for which a cardiopulmonary test should be performed.
Material and methods
The study was carried out on 107 patients on a treadmill (average age was 52.5 years, men - 74.6% and women - 25.4%) and 108 patients on VEM (average age was 49.4 years, men - 76.8% and women – 23.2%). NP on the treadmill was carried out according to the protocol of Bruce and mod. Bruce, NP on VEM was carried out according to the 50+25 and 25+25 protocol. The ECG was monitored in 12 standard leads, blood pressure was monitored at baseline, at the 2nd minute of each load step and at every minute of the recovery period. Upon completion of the load as a result of achieving a submaximal heart rate without electrocardiographic and clinical signs of angina, the test was regarded as negative.
If atypical discomfort in the chest appeared during exercise without ECG signs of myocardial ischemia, as well as ST segment depression of 1 mm or more in people with a low pre-test probability of coronary artery disease, the test was regarded as doubtful. A test terminated as a result of fatigue when submaximal heart rate was not achieved in the absence of clinical and ECG signs of myocardial ischemia was considered incomplete. Horizontal or other ST segment depression of 1 mm or more in individuals with an average or high pre-test probability of CAD was considered a positive test. The results of the study are presented in the table .
Diagnosis of coronary heart disease: what is expected and what is gained from functional diagnostics
Download Slideshow
Author: Tikhonenko, V. M.
PDF file
The widespread prevalence and great social significance of coronary heart disease (CHD) necessitates timely and as complete diagnosis as possible. IHD, angina pectoris, is a pathology where functional diagnostic methods come to the fore, since at rest all parameters of the heart are usually normal, and in some patients, anatomical damage to the coronary arteries is absent or insignificant. Diagnosis of this pathology and assessment of its severity is based on identifying signs of transient myocardial ischemia using ECG or imaging techniques.
During the development of transient myocardial ischemia, the following sequence (“cascade”) of events usually develops—impaired myocardial perfusion, impaired contractility of areas of the heart muscle, changes in the action potential of myocardial cells, pain. Accordingly, signs of ischemia can be detected using different methods - ECG, echocardiography, computed tomography, myocardial scintigraphy... Of course, not all disorders can be seen in all patients - many may not have changes on the ECG or echocardiogram. As a result, the sensitivity of functional diagnostic methods never reaches 100%.
Methods for diagnosing transient ischemia are divided into two groups - provocative tests and observation of spontaneously occurring ischemia. The appearance of myocardial ischemia can be provoked with the help of exercise (bicycle ergometry or treadmill test), with the help of rapid stimulation of the heart (transesophageal EPI - ischemic test), with the help of the administration of pharmaceuticals (dipyridamole, isoproterenolol, ergonovine...) and some other influences (cold, psycho-emotional tests ). The advantage of provocative tests is the possibility of using different methods for recording ischemia - from ECG and echocardiography to computed tomography and myocardial scintigraphy. In many cases, methods are used in combination, which increases sensitivity; for example, stress echocardiography involves recording not only the structure of the heart, but also the ECG. The disadvantage of provocative techniques, in addition to their potential danger, is the inability to achieve ischemia in some patients.
Most often in the clinic, stress tests (ST) are used on a bicycle ergometer or exercise machine. They are highly sensitive (especially for exertional angina), quite physiological, and allow not only to confirm the diagnosis of coronary artery disease, but also to determine the functional class of the disease, taking into account exercise tolerance. In Russia, bicycle ergometry is more common (not so expensive equipment), abroad - treadmill (for many patients, walking is more familiar than pedaling a bicycle). The advantages of NP include their low risk (complications among experienced doctors are observed in isolated cases) and ease of burden for the patient, as a result of which they can be repeated several times if necessary (for example, to monitor treatment).
However, there are many contraindications for NP - from high blood pressure to obliterating diseases of the lower extremities, from heart defects and heart failure to bronchial asthma... The proportion of patients in whom stress tests are contraindicated reaches 20 - 35%, especially in old age. In these cases, pharmacological tests or ischemic testing are an alternative. The former are used less frequently due to their potential danger, and rapid atrial pacing is used in many clinics. A comparison of these samples is given in table. 1. It can be seen that in most characteristics the ischemic test is inferior, and the only advantage is the possibility of performing it in patients with contraindications to NP.
Table 1. Advantages and limitations of exercise testing and ischemic testing.
| Ischemic test | Load tests (bicycle ergometer or treadmill) |
| Fewer contraindications (possible with high blood pressure, diseases of the lower extremities, heart failure...) | A wide range of contraindications (up to 20 - 35%). |
| Less sensitivity (up to 60 – 70%), | High sensitivity (up to 75 – 85%), |
| Not used in all hospitals and clinics. | Widely distributed in practical healthcare institutions |
| Unpleasant for the patient. | Familiar for the patient - can be repeated several times. |
It should be noted that a wide range of provocative tests are used to confirm the diagnosis of angina pectoris (HF). In HF, using certain tests, it is possible to induce transient myocardial ischemia in 85–90% of patients. Carrying out tests for angina at rest is less common, due to their low sensitivity not reaching even 50% (cold, psycho-emotional test) or due to the high risk of conducting (ergonovine test).
Observation of spontaneously occurring ischemia is possible in the intensive care unit, when recording an ECG during an attack of angina, but most often it is currently carried out using Holter monitoring (HM) - recording an ECG in conditions of everyday life using wearable recorders [1]. The advantages and limitations of HM are presented in Table. 2.
Table 2. Advantages and limitations of Holter monitoring and stress testing.
| Holter monitoring | Load tests (bicycle ergometer or treadmill) |
| It is possible to identify any type of angina (rest, cold, emotional, decubital...). | Only exertional angina is detected |
| In ordinary life, diagnostically significant loads are achieved less frequently (up to 65-80%) | More often, a diagnostically significant level of load is achieved (up to 85 - 90%). |
| No contraindications | A wide range of contraindications (up to 20 - 35%). |
| It is impossible to assess exercise tolerance | Exercise tolerance is assessed in absolute units |
| There are no complications | Complications are possible (up to 1 – 2%). |
| Objectification of ischemia only using ECG | Objectification of ischemia is possible using different methods. |
As you can see from the table, both methods have advantages and disadvantages. The use of CM is essentially the “method of choice” for confirming the diagnosis in the following cases:
- Angina at rest, since NP is useless,
- HF with significant fluctuations in exercise tolerance and with special types of angina (cold, emotional), since NP can often be negative,
- Unstable angina, since NP is contraindicated [2].
There is even a purely “Holter” diagnosis – Prinzmetal’s angina or variant angina or a special form of angina. [3]. In this form, attacks of resting angina are accompanied on the ECG by ST segment elevation (as happens with myocardial infarction, but quickly disappearing), which can usually be detected only with CM (Figure 1).
Figure 1. Registration of ST segment elevation during an attack of resting angina allows one to diagnose a special form of angina – Prinzmetal’s angina. Shown are graphs of ST segment displacement, ECG fragments – at baseline and during an attack (on the right). In the center is an overlay of the averaged ECG during an attack (red) on the initial one (blue). HM was carried out on the Cardiotechnika-04 system from INKART (Russia).
The value of CM in resting angina is so significant that if this form is suspected, the absence of attacks during 24 hours of observation is an indication for multi-day ECG monitoring (Figure 2). Indeed, it is possible to confirm the diagnosis of isolated angina at rest other than CM only with the help of tests with ergonovine, but due to the high danger of these tests, they are very rarely used.
Figure 2. Modern Holter monitors are very miniature and can record 12 ECG leads for a week.
HM is of particular importance in cases of painless ischemic heart disease [4], when only with its help it is possible to assess the severity of the patient’s condition.
In classical HF, both methods can confirm the diagnosis, but to obtain high sensitivity, CM must be properly organized. Obviously, if a patient with HF is in a hospital on bed rest, then the probability of registering transient myocardial ischemia during CM will tend to zero. However, many doctors perform CM in such conditions and talk about the low sensitivity of the method. In case of heart failure, the HM method shows good sensitivity only if on the day of observation the patient performs his usual loads.
It is impossible not to note such a limitation of CM as the objectification of myocardial ischemia only with the help of an ECG, while in case of NP, echocardiography and other methods can be used. This limitation is especially significant for patients who have initial ECG changes that mask those that appear during ischemia. These are complete blockades of intraventricular conduction, manifesting WPW syndrome, and constant stimulation of the ventricles. With coronary artery disease, up to 3–5% of patients with such changes occur and the assessment of ischemia by ECG is impossible in them.
In the past, HM had another limitation - the small number of leads recorded - only 2 or 3, while with NP 12 were recorded. This reduced sensitivity by 25 - 30%. Modern Holter monitors record 12 leads and this limitation is removed. However, in many organizations CM is still carried out on old devices, which must be taken into account when interpreting the results.
By using 12-lead monitors and instructing the patient about the need for exercise during observation, the sensitivity of CM can be obtained comparable to that of NP. The results of a comparison of the two methods in a group of patients (n - 220) with verified coronary artery disease and angina are shown in Figure 3. It can be seen that in the presence of angina at rest, the sensitivity of CM is higher than that of NP and adding samples to the patient’s examination scheme does not increase it.
Figure 3. Sensitivity of Holter monitoring and exercise tests on a bicycle ergometer in patients with verified coronary artery disease.
In isolated HF, the sensitivity of the methods was equal (82% each), but the combination of methods increased it to 88%. Patients were observed who did not reach the threshold during everyday activities, but reached the threshold level during NP. On the other hand, there were patients in whom ECG changes were not detected during NP, whereas they appeared during more severe attacks during CM. Thus, in HF, a combination of both methods is advisable. We definitely perform NP for patients who have not experienced HF attacks during CM.
Taking into account the capabilities of various functional diagnostic methods, the following diagnostic algorithm can be proposed to confirm the diagnosis of IHD:
- If the patient has ECG signs that can mask ischemic changes, the examination begins with stress echocardiography or isotope methods, if not, then with CM,
- If ECG changes specific to myocardial ischemia are detected during Holter monitoring, then their combination with pain is assessed, if not, then provocative tests are performed for HF or multi-day monitoring for angina at rest,
- If ECG changes are not detected during CM, then if there are contraindications to NP, an ischemic test is performed, if there are no contraindications, a bicycle ergometry or treadmill test is performed,
- If during CM or NP there is a combination of ECG signs of myocardial ischemia with pain, the diagnosis is confirmed; if not, then the diagnosis is confirmed by stress echocardiography or using isotope methods.
The main points of this algorithm were substantiated earlier, but it is probably worth clarifying the point about the combination of ECG changes with pain. The fact is that the specificity of typical ECG changes is quite high - about 80% (a very good figure in medicine). But if these changes are not confirmed by anything else, then the probability of an incorrect diagnosis is still about 20%, which is unacceptable. Therefore, the ischemic nature of ECG changes must be confirmed by other methods. If they are combined with a typical attack of angina, the specificity of which approaches 75%, then the combination of these two independent signs will give us 95% confidence in the correctness of the diagnosis.
Thus, modern functional diagnostic methods allow the doctor in almost all cases to objectively confirm the diagnosis of coronary heart disease and angina. With the correct choice of the sequence of application of methods and their organization, such an examination does not take much time and is not very burdensome for the patient. Of course, functional diagnostic methods make it possible not only to confirm the diagnosis, but also to assess the severity of the disease, its pathogenesis, determine the prognosis, choose the right treatment tactics and monitor its effectiveness and safety, but this is the topic of another article.
Literature:
- Norman J. Holter. New Method for Heart Studies: Continuous electrocardiography of active subjects over long periods is now practical \\ .-SCIENCE, 1961, V. 134. p. 1214
- Almazov V.A., Ermilov L.M., Kuleshova E.V. Unstable angina: issues of diagnosis, pathogenesis and medical tactics.\\ Cardiology., 1984, T. 24, N 10, p. 5.
- Prinzmetal M., Kennemer R. Angina pectoris: A variant form pectoris: Preunary report\\ Amer.J.Med., 1959, V. 27. p. 375.
- Stern S., Trivoni D. Early detection of silent ischemic heart diseases by 24-hour electrocardiographic monitoring of active subjects\\ Brit/ Heart J., 1974, V.36, p. 481.
Discussion
The clinician, and with him the patient, are usually interested in two questions before performing NP. First, is there coronary atherosclerosis? The answer to this question seems quite ambiguous and may be misinterpreted, since the NP can confidently diagnose only hemodynamically significant occlusion of the coronary arteries. Secondly, is there a need for intervention [2]. Based on this, risk assessment or prognostic stratification is one of the turning points in medical practice.
Most studies using NP have focused on the relationship between stress test scores and survival, whereas the relationship between NP scores and the risk of myocardial infarction is less clear. This is due to the fact that in most cases, significant cardiac events (sudden death, acute myocardial infarction and unstable angina) are caused by microscopic ruptures or damage to the atherosclerotic plaque. However, most vulnerable plaques appear to be angiographically insignificant before rupture (ie, with stenosis of less than 75% of the vessel diameter) and therefore may not produce clinical manifestations during loading. On the other hand, most significant plaques (those with greater than 75% stenosis) are stable on coronary angiography and have a low risk of rupture. Thus, the ability of any type of NP to detect vulnerable atherosclerotic plaques may be limited by the small size and reduced impact on coronary blood flow of these plaques, which may explain the acute coronary events that may occur soon after a negative stress test.
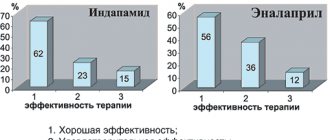
As can be seen from the results of our study (table)
The treadmill test was more sensitive in diagnosing IHD compared to VEM. A positive test was detected in 24.1% of patients on the treadmill and only in 9.6% on VEM. Of course, the results obtained, due to the small sample and, therefore, possible population differences, are of an evaluative nature and do not claim to be universal. However, it is possible that the more familiar, physiological nature of the treadmill load led to a greater number of completed trials, that is, studies reaching endpoints (submaximal heart rate, clinical angina, significant ST segment depression). On the other hand, VEM was accompanied by more frequent cases of incomplete tests, that is, termination of the test due to local fatigue of the muscles of the lower extremities before the development of clinical manifestations of the disease.
It is also noteworthy that VEM and treadmill test were relatively effective in identifying patients with angina pectoris of functional class III-IV, while the number of people with angina pectoris of functional class I-II diagnosed on a treadmill was significantly larger. Identification of patients with angina pectoris of medium and heavy loads is all the more valuable because it allows one to influence the process of coronary atherosclerosis through therapy at earlier stages, and also makes it possible to dynamically monitor patients and, therefore, control the disease process.
Table
Physiological basis of tests with gradually increasing cardiovascular load
Cardiovascular response
At the first stages of the stress test (up to 50% of the maximum load), cardiac output increases due to an increase in both heart rate and stroke volume; at a higher intensity of the load, the increase in cardiac output is caused mainly by an increase in heart rate; this adaptation mechanism allows, during maximum stress, to increase cardiac output by 4-6 times.
Physiological response to gradually increasing load
| Index | Designation and unit of measurement | English designation | Peace | Peak load | Increase compared to rest |
| Heart rate | Heart rate (bpm) | HR (bpm) | 70 | 180 | 2,6 |
| Stroke volume | VO (ml) | SV(mL) | 80 | 140 | 1,7 |
| Cardiac output | SV (l/min) | CO (L/min) | 5,6 | 25 | 4,5 |
| Systolic blood pressure | SBP (mmHg) | SBP (mmHg) | 120 | 180 | 1,5 |
| Diastolic blood pressure | DBP (mmHg) | DBP (mmHg) | 80 | 80 | 1 |
| Average blood pressure | BP avg. (mmHg.) | MAP (mmHg) | 93 | 113 | 1,2 |
| Total peripheral vascular resistance | OPSS (mm Hg/l/min) | TPR (mmHg/L/min) | 16,6 | 4,5 | 0,27 |
| Arteriovenous difference in O2 | Δ(a-c)O2 (ml/dl) | Δa-vO2 (mL/dL) | 5 | 16 | 3,2 |
| O2 consumption | PO2 (ml/min) | VO2 (mL/min) | 280 | 4000 | 14,3 |
| Breath volume | OD (ml) | Vt (mL) | 500 | 1800 | 3,6 |
| Breathing rate | RR (breaths/min) | BF (breaths/min) | 12 | 40 | 3,3 |
| Minute breathing volume | MOD (l/min) | VE (L/min) | 6 | 72 | 12 |
Systolic and mean blood pressure increase in parallel with the gradual increase in load, while diastolic blood pressure does not change or even decreases. In addition, a redistribution of blood flow occurs due to selective vasoconstriction of the mesenteric and other visceral arteries and vasodilation of the arteries of skeletal muscles involved in physical activity; Systemic vascular resistance is significantly reduced at both submaximal and maximum load levels. Resting heart rate, as well as its increase in response to increasing physical activity (i.e., chronotropic capacity) have a clear prognostic significance in asymptomatic patients: according to the results of the Framingham study, resting heart rate was associated with the level of total, cardiovascular and coronary mortality in 5070 asymptomatic men and women over a 30-year follow-up period. The correlation was stronger in men than in women and was independent of the presence of other cardiovascular risk factors. The risk of sudden cardiac death was closely related to resting heart rate. A smaller cohort study, the Framingham Offspring Study, examined the clinical significance of heart rate response to stepwise exercise. In this study, failure to achieve target heart rate (85% maximum for age), less increase in heart rate in response to exercise, and the chronotropic response index were predictors of all-cause mortality and morbidity of coronary artery disease. Not only the load-induced increase in heart rate, but also the process of heart rate recovery immediately after physical activity is closely related to the initial level of training and the state of the cardiovascular system. Cole et al. 2428 people with no history of coronary artery disease were observed for 6 years. Study participants performed a symptom-limited exercise test; heart rate recovery was defined as a decrease in maximum heart rate during the first minute after cessation of exercise; a decrease of less than 13 beats per minute was considered pathological. Insufficient heart rate recovery was a predictor of death (relative risk 4.0, CI 3.0–5.2), even after adjustment for sex, age, drug therapy, standard cardiovascular risk factors, and resting heart rate. The close relationship between the increase in heart rate in response to exercise and the recovery of heart rate after cessation of exercise and cardiovascular mortality highlights the clinical importance of routine exercise testing in assessing patient prognosis.
Respiratory response
The respiratory response to exercise can be accurately assessed during cardiopulmonary exercise testing, in which minute ventilation and expired gases (O2in and CO2ex) are measured while breathing through a face mask connected through an air flow transducer to a gas analyzer. Due to the technical complexity of the study, the cardiopulmonary stress test is not used for routine assessment of physical performance, however, it allows one to obtain important additional information for understanding the physiology of the pathological process in special categories of patients: with CHF, diseases of the respiratory system, candidates for transplantation, patients with decreased exercise tolerance for unclear reasons. The table provides a short list of the main abbreviations and technical terms used when performing cardiopulmonary exercise testing.
Abbreviations used when performing a cardiopulmonary test and interpreting its results
| Index | Designation and unit of measurement | English designation |
| Minute breathing volume | MOD (l/min) | VE (L/min) |
| Oxygen consumption per 1 min | O2vd (l/min) | VO2(L/min) |
| Carbon dioxide release in 1 minute | CO2out (l/min) | VCO2(L/min) |
| Oxygen partial pressure | PO2(mmHg) | PO2 (mmHg) |
| Partial pressure of carbon dioxide | PCO2 (mmHg) | PСO2 (mmHg) |
| Tidal volume (breathing volume) | OD (l) | VT(L) |
| Dead space volume | MP (l) | VD(L) |
| Functional residual capacity | FFU (l) | EELV(L) |
| O2 partial tension at end tidal expiration | PoutO2 (mm Hg) | PETO2(mmHg) |
| Partial pressure of CO2 at the end of quiet expiration | PoutCO2 (mmHg) | PETCO2(mmHg) |
| Ventilatory anaerobic threshold (if calculated per unit of body weight - ml/min×kg) | VAP (ml/min) | VAT (mL/min) |
| Peak oxygen consumption, measured at peak load individually for each patient, characterizes maximum performance (if calculated per unit body weight - ml/min×kg) | AUC (ml/min) | Peak VO2(mL/min) |
The respiratory response during the test with a gradually increasing load increases in proportion to the CO2 formed in the process of energy metabolism, which is necessary for its adequate removal from the body. Excess CO2, which is formed when lactate is buffered above the anaerobic threshold, leads to irritation of the respiratory center, as a result of which the minute volume of respiration (MVT) increases, which helps to maintain a linear relationship between MVT and produced CO2 (CO2 exhaled), resulting in the partial pressure of CO2 at the end of expiration ( PexCO2) remains unchanged. However, at the end of the stress test, hyperventilation also develops in relation to CO2 - as a respiratory compensation of load-induced metabolic acidosis, which leads to an increase in the ventilatory equivalent of CO2 (MOD/CO2out) and a decrease in PoutCO2. The ventilatory requirement to remove CO2 formed during metabolism is described by the modified alveolar equation:
MOD = (863 × CO2ext) / (PexCO2× [1 - MP/DO]),
where MP/DO is the ratio of physiological dead space (MD) to tidal volume (TV).
Metabolism in skeletal muscle
During gradually increasing physical activity, a level of energy demand is reached, above which the concentration of lactate in the blood plasma begins to rapidly increase (“anaerobic threshold”). This is a consequence of the activation of anaerobic glycolysis, which occurs under conditions where the rate of oxygen delivery is insufficient for the rapid oxidation of nicotinamide adenine dinucleotide (NADH) in the cytoplasm. Almost all H+ ions formed in cells from lactic acid (La) are neutralized by the bicarbonate buffer system:
H+ + La- + HCO3- ↔ H2O + CO2 + La-
Anaerobic metabolism is accompanied by excessive production of CO2 (excess CO2), this leads to the fact that the slope of the graph reflecting the dynamics of the ratio of CO2out to O2in becomes steeper. By measuring changes in the composition of exhaled gas caused by metabolic disorders, it is possible to determine the “ventilatory anaerobic threshold” by analyzing the ratio of CO2out to O2in. The ventilatory anaerobic threshold is the transition point from exclusively aerobic metabolism, when CO2ext / O2in ‹1, to aerobic-anaerobic metabolism, when CO2ext / O2in>1. In healthy people and cardiac patients without CHF, the ventilatory anaerobic threshold is usually at the level of 50-60% of peak O2 consumption, and in patients with CHF this figure increases.
Calculation of the respiratory anaerobic threshold: By measuring changes in the composition of exhaled gas caused by metabolic disorders, the “ventilatory anaerobic threshold” (VAT) can be determined by analyzing the ratio of CO2exhaled to O2inhaled (respiratory gas exchange coefficient). The ventilatory anaerobic threshold is the transition point from exclusively aerobic metabolism, when CO2exO2in ‹1, to aerobic-anaerobic metabolism, when CO2ex/O2in>1.
Criteria for achieving maximum load level
Achieving the maximum level of tension during a test with a gradually increasing load is a key point for assessing both the functional status and prognosis of patients; it can be determined by the following criteria:
- insufficient increase in O2bp and/or heart rate, its inconsistency with the increasing amount of work
- peak respiratory gas exchange coefficient (CO2ex/O2in) ≥1.10-1.15
- blood lactate concentration after exercise ≥8 mmol/dl (used in athletes, rarely achieved in patients)
- self-assessment of effort ≥8 (on a 10-point Borg scale)
- the patient's appearance (exhaustion).
Borg Physical Exercise Severity Rating Scale (Borg)
| Point | Interpretation |
| 0 | No load |
| 0,5 | Extremely light |
| 1 | Very light |
| 2 | Lightweight |
| 3 | Moderate |
| 4 | A little heavy |
| 5 | Heavy |
| 6 | |
| 7 | Very heavy |
| 8 | |
| 9 | |
| 10 | Extremely heavy |
| • | Maximum |
However, it must be remembered that all indicators of physical performance are only close to the actual maximum load level. In most cardiac patients, it becomes necessary to stop the stress test before achieving the listed criteria due to the development of cardiac symptoms (i.e., a symptom-limited stress test is performed). Peak physical performance, measured for example by maximal oxygen consumption, depends on three key physiological systems:
- efficiency of gas exchange in the lungs
- maximum cardiac output
- aerobic metabolic capacity of working skeletal muscles
Comparative results of the effectiveness of the treadmill test and bicycle ergometry
| Research result | Treadmill test number of patients /% | VEM number of patients /% |
| I. Negative test | 47 / 43,9% | 61 / 56,5% |
| II. Doubtful sample | 21 / 19,6% | 9 / 8,3% |
| III. Unfinished sample | 13 / 12,2% | 28 / 25,9% |
| IV. Positive test | 26 / 24,3% | 10 / 9,3% |
| 1. Low tolerance (III-IV FC) | 5 | 6 |
| 2. Average tolerance (II FC) | 20 | 4 |
| 3. High tolerance (I FC) | 1 | 0 |
Given the limitations of analyzing only ST segment depression in risk stratification, a number of authors have proposed using other indicators obtained during NP in prognostic assessment. Thus, using regression analysis, Mark et al [3] created the Duke score scale.
Duke scale
The Duke scale is calculated as follows: NP time according to the Bruce protocol (or MET) – 5 * (degree of maximum deviation of the ST segment in mm) – 4 * (angina index during NP). The angina index has a value of 0 if angina was not observed during NP, 1 if angina was recorded and 2 if angina was the reason for cessation of NP. If the ST segment deviation was less than 1 mm, the value entered into the ST deviation score was 0. Based on this scoring scale, a high-risk group was defined as having a score greater than/equal to -11 (average annual cardiovascular mortality greater than 5% ), as well as a group of low-risk patients – greater than/equal to +5 points (average annual cardiovascular mortality 0.5%).
Based on the data obtained, patients at high risk according to the Duke scale should be offered coronary angiography and, possibly, revascularization procedures [2]. Low-risk patients do not require additional examination and can receive conservative therapy. Patients at intermediate risk should undergo stress echocardiography as a test for further risk stratification. Patients with intermediate risk, dyssynergia of no more than one segment on stress echocardiography and normal heart size have a low risk of death and can receive conservative therapy. On the other hand, patients with the development of local contractility disorders of two or more segments on stress echocardiography should be referred to coronary angiography [2, 3].
Load Test Security
Indications and contraindications
Over the past decades, data on the risk-benefit ratio of stress testing in various diseases have been systematically studied. As a result, the indications and contraindications for exercise testing have been clearly formulated, as outlined in the recommendations of the American Heart Association and the European Society of Cardiology. Exercise testing is seen as a valuable tool not only for identifying or ruling out exercise-induced myocardial ischemia, but also for determining the patient's fitness level before initiating an exercise program. Its implementation is necessary to determine the heart rate that provides an aerobic level of exercise, and to prevent the potential risk of developing complications such as exercise-induced rhythm disturbances or excessive increases in blood pressure during physical training. Indications for load testing are presented above. Large epidemiological studies have demonstrated an association between physical endurance and mortality; stress tests are widely used to objectify the degree of limitation of exercise tolerance caused by the disease, for risk stratification of patients with CHF.
Information about the frequency of complications
Despite their undeniable clinical value, maximal stress testing carries a certain risk of adverse events. In the general population of patients referred for stress testing, deaths were recorded in ‹0.01% of patients, other pathological conditions - in ‹0.05% of patients. When performing a stress test in the first 4 weeks of acute myocardial infarction, the incidence of death increases to 0.03%, and non-fatal myocardial infarction or the need for cardiac resuscitation reaches 0.09%. In patients with a stable course of compensated CHF, there is no additional (relative to patients without CHF) risk of performing a test with a maximum load level; As reported in one study, no serious complications were identified in an analysis of 1286 bicycle ergometers. The absolute risk of severe complications during stress testing can be minimized by strictly following accepted patient selection criteria, careful medical history, detailed clinical examination, continuous monitoring of a 12-lead ECG, blood pressure and their recording during exercise and every minute (minimum - every 3 minutes ) immediately after its completion.
Requirements for the conditions of the event
Although the absolute number of serious complications during stress testing is small, they can be expected to occur from time to time due to the large number of tests performed. The testing area should have CPR equipment available, including emergency medications, a defibrillator, and an endotracheal intubation kit. The stress test must be carried out by a doctor with special training or specially trained nursing staff, providing the possibility of an emergency call to a doctor. An emergency telephone number must be available at all times. To ensure that the necessary emergency care is provided efficiently and in a timely manner, staff must be regularly trained in cardiopulmonary resuscitation.