4.1. Two-stage test in test tubes with antiglobulin
4.2. Compatibility test on a plane at room temperature
4.3. Indirect Coombs test
4.4. Compatibility test using 10% gelatin
4.5. Compatibility test using 33% polyglucin
An individual compatibility test allows you to make sure that the recipient does not have antibodies directed against the donor’s red blood cells and thus prevents the transfusion of red blood cells that are incompatible with the patient’s blood.
The compatibility test, performed on a plane at room temperature, is aimed at identifying complete group agglutinins of the AB0 system, MNSs, Lewis, etc. in the recipient. The compatibility test using 10% gelatin, 33% polyglucin, an indirect Coombs test is intended to identify incomplete group antibodies. A two-stage test in test tubes with antiglobulin involves the detection of both antibodies, including group hemolysins.
The most sensitive and recommended is a two-stage test in tubes with antiglobulin, then a combination of two tests - a flat test at room temperature and an indirect Coombs test. Instead of the indirect Coombs test, a conglutination reaction with 10% gelatin or a conglutination reaction with 33% polyglucin can be used. The last test is inferior in sensitivity to the first two, but takes less time.
4.1. Two-stage test in test tubes with antiglobulin
First stage.
Add 2 volumes (200 µl) of the recipient's serum and 1 volume (100 µl) of a 2% suspension of thrice-washed donor erythrocytes suspended in saline or LISS (low ionic strength solution) into a labeled tube. The contents of the tube are mixed and centrifuged at 2500 rpm (about 600 g) for 30 s. The presence of hemolysis in the supernatant is then assessed, after which the erythrocyte pellet is resuspended by lightly tapping the bottom of the tube with a fingertip, and the presence of erythrocyte agglutination is determined. In the absence of pronounced hemolysis and/or agglutination, proceed to the second stage of the test using antiglobulin serum.
Second phase.
The tube is placed in a thermostat at 37°C for 30 minutes, after which the presence of hemolysis and/or red blood cell agglutination is again assessed. Then the red blood cells are washed three times with saline, 2 volumes (200 μl) of antiglobulin serum for the Coombs test are added and mixed. The tubes are centrifuged for 30 s, the red blood cell sediment is resuspended and the presence of agglutination is assessed.
The results are recorded with the naked eye or through a magnifying glass. Severe hemolysis and/or agglutination of erythrocytes indicates the presence in the recipient's serum of group hemolysins and/or agglutinins directed against the donor's erythrocytes and indicates incompatibility of the blood of the recipient and the donor. The absence of hemolysis and/or agglutination of red blood cells indicates the compatibility of the blood of the recipient and the donor.
What is genetic incompatibility of partners?
Genetic infertility in women and men accounts for about 10% of all types of impaired fertility. The main reason lies in a change in the quality or quantity of genes that are stored on chromosomes. As a result, when the nuclei of eggs and sperm divide, cells with an incorrect chromosome complement can be formed.
The following factors increase the risk of genetic incompatibility:
- excessive doses of radiation;
- unfavorable environmental conditions;
- marriages between blood relatives;
- hereditary diseases.
Separately, it is worth dwelling on age. The older the partners, the higher the proportion of chromosomal mutations, and this applies to a greater extent to women. On average, after 35 years, the number of eggs that have genetic disorders increases. These changes become especially noticeable in the category of women 40+ (the proportion of mutant oocytes can reach 80%).
In case of severe genetic damage, the mechanism of natural selection is triggered. Embryos with the wrong chromosome set sooner or later stop in their development, which leads to miscarriage or missed abortion. Therefore, if there are repeated pregnancy losses, a genetic consultation is required for the couple.
As part of genetic counseling, a couple may undergo various types of tests:
- karyotyping;
- expert sperm analysis;
- analysis of mutations in specific genes that are most often associated with infertility or recurrent miscarriage;
- FISH study of sperm, eggs, etc.
4.2. Compatibility test on a plane at room temperature
Apply 2-3 drops of the recipient's serum to the plate and add a small amount of red blood cells so that the ratio of red blood cells to serum is 1:10 (for convenience, it is recommended to first release a few drops of red blood cells from the container through a needle onto the edge of the plate, then from there transfer a small a drop of red blood cells into the serum). Next, the red blood cells are mixed with the serum, the plate is gently rocked for 5 minutes, observing the progress of the reaction. After the specified time, 1-2 drops of physiological solution can be added to the reaction mixture to remove possible nonspecific aggregation of red blood cells.
Accounting for results. The presence of red blood cell agglutination means that the donor's blood is incompatible with the recipient's blood and should not be transfused. If after 5 minutes there is no agglutination of red blood cells, this means that the donor’s blood is compatible with the recipient’s blood for group agglutinogens.
Classification and characteristics of blood groups and Rh factor
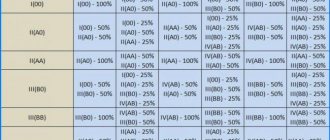
Group antigens are classified according to a single AB0 system (a, b, zero). The established concept divides the composition of blood cells into 4 main types. Their differences are in alpha and beta agglutinins in plasma, as well as the presence of specific antigens on the membrane of red blood cells, which are designated by the letters A and B.
Table "Characteristics of blood classes"
| Variety | Description |
| 1 group or zero | There are no antigens in blood cells. Plasma contains alpha and beta agglutinins |
| Group 2 (A) – the most common | Group A antibodies are present in the membrane of blood cells, and only beta-agglutinin is present in the plasma itself |
| Group 3 (B) | Red blood cells contain B antigen, but plasma contains only alpha antibody |
| Group 4 (AB) | Blood cells in their membrane contain antigens of both groups (A and B), but there are no agglutinins in the plasma |
People's nationality or race does not affect group membership.
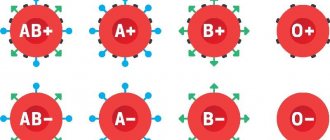
Rh factor
In addition to the AB0 system, biological material is classified according to the blood phenotype - the presence or absence of a specific antigen D in it, which is called the Rh factor (Rh). In addition to protein D, the Rh system covers 5 more main antigens - C, c, d, E, e. They are contained in the outer membrane of red blood cells.
The Rh factor and the class of blood cells are formed in the child in the womb and are passed on to him from his parents for life.
4.3. Indirect Coombs test
One drop (0.02 ml) of the sediment of thrice washed donor erythrocytes is added to the test tube, for which a small drop of erythrocytes is squeezed out of the pipette and touched to the bottom of the test tube, and 4 drops (0.2 ml) of the recipient's serum are added. The contents of the tubes are mixed by shaking, after which they are placed for 45 minutes in a thermostat at a temperature of +37°C. After the specified time, the red blood cells are washed again three times and a 5% suspension is prepared in physiological solution. Next, add 1 drop (0.05 ml) of red blood cell suspension onto a porcelain plate, add 1 drop (0.05 ml) of antiglobulin serum and mix with a glass rod. The plate is rocked periodically for 5 minutes.
The results are recorded with the naked eye or through a magnifying glass. Agglutination of red blood cells indicates that the blood of the recipient and the donor are incompatible; the absence of agglutination is an indicator of the compatibility of the blood of the donor and recipient.
Medical educational portal kbmk.info
Blood transfusion device
Final state certification (IGA) Discipline/Topic: Surgery/Blood Transfusion/Transfusiology
“If a surgeon and a transfusiologist agree on a liter of red and a liter of white, it is quite possible that we are talking about blood and plasma transfusions”
See also other tests on surgery
No. 2 * 1 - one correct answer For hemostasis, blood is transfused in small doses in order to 1) increase the volume of circulating blood 2) accelerate blood clotting 3) increase blood pressure 4) improve heart function! 2 No. 3 * 1 - one correct answer When determining the Rh factor using the express method in a test tube, agglutination occurred. This means that the blood is 1) Rh negative 2) Rh incompatible 3) Rh positive 4) Rh compatible! 3 No. 4 * 1 - one correct answer Contraindications for blood transfusion 1) major surgery 2) severe liver dysfunction 3) shock 4) decreased blood pressure! 2 No. 5 * 1 - one correct answer The rate of blood infusion during a biological test is 1) 50-60 drops per minute 2) stream 3) 20-30 drops per minute 4) 30-40 drops per minute! 2 No. 6 * 1 - one correct answer When conducting a test for Rh compatibility of the blood of the donor and recipient, an agglutination reaction occurred in a test tube. This means that the blood is 1) Rh positive 2) Rh compatible 3) Rh negative 4) Rh incompatible! 4 No. 7 * 1 - one correct answer The Rh factor is contained in 1) plasma 2) leukocytes 3) erythrocytes 4) platelets! 3 No. 8 * 1 - one correct answer Blood type that contains agglutinogens A and B 1) first 2) second 3) third 4) fourth! 4 No. 9 * 1 - one correct answer Agglutinins A and a are found in 1) erythrocytes 2) leukocytes 3) blood plasma 4) other body fluids! 3 No. 10 * 1 - one correct answer Percentage of people with Rh-positive blood 1) 15% 2) 50% 3) 85% 4) 100%! 3 No. 11 * 1 - one correct answer Components of the test for individual compatibility of the blood of the donor and the recipient 1) donor plasma and recipient serum 2) recipient plasma and donor serum 3) donor plasma and recipient blood 4) recipient serum and donor blood! 4 No. 12 * 1 - one correct answer Signs of infection of the blood in the vial 1) the plasma is cloudy, with flakes 2) the plasma is colored pink 3) the plasma is transparent 4) the blood is 3-layered, the plasma is transparent! 1 No. 13 * 1 - one correct answer Hemodesis is mainly used for 1) parenteral nutrition 2) detoxification of the body 3) combating thrombosis and embolism 4) regulating water-salt metabolism! 2 No. 14 * 1 - one correct answer When determining the blood group using standard sera, agglutination occurred with serum of groups 1 and 3. This means that the blood is 1) the first group 2) the second group 3) the third group 4) the fourth group! 2 No. 15 * 1 - one correct answer When conducting a test for group compatibility of the blood of the donor and recipient, there was no agglutination. This means that the blood is 1) compatible by Rh factor 2) compatible by group affiliation 3) incompatible by Rh factor 4) incompatible by group affiliation! 2 No. 16 * 1 - one correct answer Composition of blood of group II 1) AA 2) BA 3) AB 4) O! 1 No. 17 * 1 - one correct answer Red blood cell mass is used for the purpose of 1) increasing the volume of circulating blood 2) parenteral nutrition 3) detoxification 4) treating anemia! 4 No. 18 * 1 - one correct answer Reinfusion is 1) transfusion of placental blood 2) transfusion of autologous blood 3) transfusion of canned blood 4) direct blood transfusion! 2 No. 19 * 1 - one correct answer Plasma-substituting action has 1) fibrinolysin 2) hemodez 3) manitol 4) reopolyglucin! 4 No. 20 * 1 - one correct answer The patient’s condition at the beginning of transfusion shock 1) adynamic 2) restless 3) non-contact 4) lethargic! 2 No. 21 * 1 - one correct answer The agglutination reaction is 1) a decrease in blood clotting 2) immunization of blood with the Rh factor 3) intravascular coagulation 4) gluing of red blood cells with their subsequent destruction! 4 No. 22 * 1 - one correct answer Blood of group B (III) can be administered to persons 1) only with III blood group 2) with any blood group 3) only with III and IV blood groups 4) with II and III blood groups! 1 No. 23 * 1 - one correct answer When examining a bottle of preserved blood, it was established that the blood was stored for 25 days. Your conclusion about the suitability of the blood: 1) the blood is infected and not suitable for transfusion 2) the blood is suitable for transfusion 3) the shelf life has expired, it cannot be transfused 4) the blood is hemolyzed, it cannot be transfused! 3 No. 24 * 1 - one correct answer To conduct a biological test, you should 1) inject a single stream of 25 ml of blood and observe the patient’s condition for 5 minutes. 2) inject a stream of 25 ml of blood three times with an interval of 5 minutes, observing the patient 3) inject a drip of 25 ml of blood, observe the patient’s condition for 5 minutes 4) inject three times a drip of 25 ml of blood! 2 No. 25 * 1 - one correct answer During the blood transfusion, the patient’s condition worsened, pain appeared in the lower back and behind the sternum. This indicates 1) hemorrhagic shock 2) citrate shock 3) blood transfusion shock 4) pyrogenic reaction! 3 No. 26 * 1 - one correct answer When signs of transfusion shock appear during blood transfusion, it is necessary to 1) change the system and administer blood substitutes 2) turn off the system, remove the needle from the vein 3) reduce the speed and continue blood transfusion 4) continue blood transfusion and urgently administer drugs! 1 No. 27 * 1 - one correct answer The result of the agglutination reaction when determining the blood group using standard sera is determined after 1) 1 min 2) 2 min 3) 3 min 4) 5 min! 4 No. 28 * 1 - one correct answer To stabilize donor blood, use 1) glucose 2) 2.6% sodium citrate solution 3) glycerin 4) isotonic solution! 2 No. 29 * 1 - one correct answer Maximum shelf life of whole blood 1) 7 days 2) 14 days 3) 21 days 4) 28 days! 3 No. 30 * 1 - one correct answer The blood product is 1) albumin 2) erythrocyte mass 3) leukocyte mass 4) native plasma! 1 No. 31 * 1 - one correct answer In case of hemorrhagic shock, first of all, the patient should be transfused with 1) whole blood 2) plasma 3) polyglucin 4) platelet mass! 3 No. 32 * 1 - one correct answer After a blood transfusion, the nurse monitors 1) pulse 2) pulse and blood pressure 3) diuresis 4) pulse, blood pressure and diuresis! 3 No. 33 * 1 - one correct answer The blood component that has the most pronounced hemostatic effect 1) leukocyte mass 2) plasma 3) erythrocyte mass 4) erythrocyte suspension! 2 No. 34 * 1 - one correct answer Donor blood is stored in a refrigerator at a temperature of 1) -2-0 degrees 2) 0-2 degrees 3) 4-6 degrees 4) 7-10 degrees! 3 No. 35 * 1 - one correct answer If the blood transfusion technique is violated, complications may develop: 1) citrate shock 2) anaphylactic shock 3) blood transfusion shock 4) air embolism! 4 No. 36 * 1 - one correct answer The shelf life of a bottle with residual blood after a transfusion is 1) 6 hours 2) 12 hours 3) 24 hours 4) 48 hours! 3 No. 37 * 1 - one correct answer When determining the blood group, after a preliminary assessment of the result, add 1) sodium citrate 2) isotonic sodium chloride solution 3) hypertonic sodium chloride solution 4) distilled water! 2 No. 38 * 1 - one correct answer The standard serum titer for determining blood group must be at least 1) 1:8 2) 1:32 3) 1:64 4) 1:16! 2 No. 39 * 1 - one correct answer The number of cells on the plate filled with standard sera when determining the blood group 1) 3 2) 6 3) 7 4) 4! 2 No. 40 * 1 - one correct answer Plasma substitutes do not include 1) polyglucin 2) blood serum 3) gelatinol 4) rheopolyglucin! 2 No. 41 * 1 - one correct answer A healthy person aged from 1) 16 to 55 years old 2) 18 to 60 years old 3) 18 to 55 years old 4) 16 to 50 years old can be a blood donor! 3 No. 42 * 1 - one correct answer Donation is contraindicated if there is a history of 1) otitis media 2) appendicitis 3) viral hepatitis 4) pneumonia! 3 No. 43 * 1 - one correct answer 1) hydrolysin 2) gelatinol 3) polyglucin 4) albumin are prepared from human blood! 4 No. 44 * 1 - one correct answer Polyglucin is primarily used for 1) parenteral nutrition 2) detoxification 3) combating shock 4) accelerating blood clotting! 3
4.4. Compatibility test using 10% gelatin
Add 1 small drop (0.02 - 0.03) ml of donor erythrocytes into the test tube, for which squeeze out a small drop of erythrocytes from a pipette and touch the bottom of the test tube with it, add 2 drops (0.1 ml) of gelatin and 2 drops (0.1 ml) recipient serum. The contents of the tubes are mixed by shaking, after which they are placed in a water bath for 15 minutes or a thermostat for 30 minutes at a temperature of +46 - 48°C. After the specified time, add 5 - 8 ml of physiological solution to the test tubes and mix the contents by inverting the test tubes 1 - 2 times.
The result is taken into account by viewing the test tubes with the naked eye or through a magnifying glass. Agglutination of red blood cells indicates that the blood of the recipient and the donor are incompatible; the absence of agglutination is an indicator of the compatibility of the blood of the donor and recipient.
What can incompatible couples do?
The method of treating marital incompatibility depends on the established diagnosis.
- In case of immune infertility, lymphocyte immunotherapy can be performed, which allows changing the state of the mother's immune system in the direction of protecting the embryo. This treatment method can be combined with immune drugs or hormone therapy.
- In case of genetic infertility, it is recommended to use assisted reproduction methods, which make it possible to evaluate its chromosomal and gene set before embryo transfer in order to exclude the transmission of hereditary diseases.
- If there are antisperm antibodies, the couple is recommended to live with a condom for at least 1 month in order to reduce the level of sensitization in the male and female body. At the same time, desensitizing and immunosuppressive therapy is prescribed.
4.5. Compatibility test using 33% polyglucin
Add 2 drops (0.1 ml) of recipient serum, 1 drop (0.05) ml of donor erythrocytes into the test tube and add 1 drop (0.1 ml) of 33% polyglucin. The test tube is tilted to a horizontal position, shaking slightly, then slowly rotated so that its contents spread over the walls in a thin layer. This spreading of the contents of the test tube along the walls makes the reaction more pronounced. Contact of erythrocytes with the patient’s serum while rotating the tube should continue for at least 3 minutes. After 3-5 minutes, add 2-3 ml of physiological solution to the test tube and mix the contents by inverting the test tube 2-3 times without shaking.
The result is taken into account by viewing the test tubes with the naked eye or through a magnifying glass.
Agglutination of red blood cells indicates that the blood of the recipient and the donor are incompatible; the absence of agglutination is an indicator of the compatibility of the blood of the donor and recipient. [/td]
When is blood type determination performed?
Indications for determining blood group are:
- the need for blood transfusion;
- preparation for operations. Any operation is a risk; under certain circumstances, it may be necessary to replace blood loss, and then doctors should know what kind of blood can be used for this;
- management of pregnancy. In some cases, there may be incompatibility between the blood groups of mother and child. If there is a blood type conflict, the child may be born with hemolytic disease of the newborn (hemolytic jaundice). To determine the baby's blood type, umbilical cord blood is taken for analysis immediately after birth. But a conflict based on blood type can also be judged during pregnancy – by the level of antibodies in the mother’s blood. The risk of blood type incompatibility between mother and child is calculated based on the likely blood type of the child, which, in turn, depends on what blood type the mother and father have. To assess this risk, it is necessary to take a test to determine your blood type during pregnancy.
Blood group determination
When doctors need to find out the blood type, the analysis is usually done again. This is done to completely eliminate the possibility of errors resulting from the use of incorrect data. The doctor will not ask the patient’s blood type, since he is responsible for his life and must have one hundred percent confidence that the blood type is determined correctly.
But knowing your blood type (and the blood type of your children) is still useful. Firstly, no one can be immune from emergencies. And secondly, there is a certain relationship between blood type and predisposition to various diseases.
Is it possible to do IVF if the spouses are incompatible?
Yes, sure! In vitro fertilization is the method of choice to help couples who are faced with incompatibility. Reproductologists have a unique opportunity to neutralize the negative impact of unfavorable internal environmental factors that disrupt the process of pregnancy.
In reproductive services, couples can receive a full range of services for the diagnosis and treatment of even the rarest forms of infertility. Our center conducts examinations that help identify the exact cause of incompatibility between spouses in order to select the most optimal ways to solve the problem. We accompany the couple at all stages of the journey to long-awaited parenthood. Sign up for a consultation at SM-Clinic at convenient office hours!