For some reason, diseases of the large intestine, anus, and anus are considered something shameful. It is not customary to talk about them. Patients often delay seeing a doctor, preferring, due to some fictitious rules of decency, to worsen their health and quality of life.
Hemorrhoids are considered such an indecent disease. This should not be considered a punishment from God or the prerogative of the female half of humanity. Pathology does not select the height, age and gender of the patient. Internal hemorrhoids occur equally often in both men and women. What are the signs of internal hemorrhoids?
Signs of the second stage of hemorrhoids
The second stage of hemorrhoids is characterized by a significant increase in internal nodes with constant bleeding, which is accompanied by severe pain, itching and burning in the anus. At the second stage, the nodes fall out of the anus, which are reduced on their own.
The patient constantly has a sensation of a foreign body in the rectum, a feeling of incomplete bowel movement after defecation. At this time, constipation often appears, since enlarged hemorrhoids create obstacles for the exit of feces. In addition, the act of defecation due to trauma to the hemorrhoids is often very painful and can also contribute to their prolapse.
Bleeding from the anus becomes constant, its traces are clearly visible on toilet paper, in stool and on underwear. The mucus and blood released when the node is damaged irritates the intestinal mucosa, causing itching and burning in the anus.
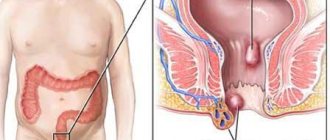
The disease can be acute or chronic, and depending on the location of the hemorrhoids, hemorrhoids can be internal, external or mixed.
Hemorrhoids: classification
Hemorrhoids can be either internal or external.
Among ordinary people, this disease is clearly associated with the prolapse of hemorrhoids during bowel movements or heavy work. Doctors divide this pathology into 3 groups:
- External hemorrhoids are symptoms familiar to many
- Internal hemorrhoids are an invisible but no less unpleasant pathology.
- Combined type - combines all the features of the first two
How to distinguish from external?
In fact, this type of pathology differs little from the external habitual disease. But nodular seals form inside the rectum. Therefore, this variety does not have external manifestations. You will not be able to diagnose this disease yourself. Only an experienced proctologist can establish the correct diagnosis.
Causes of the disease
Doctors identify several main causes of this pathology:
- Poor nutrition – heavy, fatty foods. Modern people do not consume enough vegetables and fruits and cereal products. But he abuses sweets, fried meat, smoked meats and other unhealthy foods. This imbalance in nutrition leads to disturbances in bowel movements - constipation occurs. And the more often a patient reads books on the toilet, the higher the likelihood of developing hemorrhoids of any type.
- Lack of physical activity - sofa at home, working in an office, traveling exclusively by car - this is the appearance of a modern city dweller. This leads to congestion in the pelvic area. The result is one form or another of hemorrhoids.
- Alcohol – a little wine won’t hurt. But excessive doses of ethyl alcohol lead to disruption in the body’s vascular system. The result may be hemorrhoids, cirrhosis or fibrosis of the liver, and mental degradation.
- Physical activity - it would seem that all problems are due to lack of physical activity. But excessive lifting of weights and heavy physical labor also contribute to troubles in the anus.
Pregnancy in women is a type of heavy physical stress on the pelvic veins. In addition, while waiting for the baby, intestinal motility is disrupted, and women suffer from constipation. Childbirth also does not add health.
No one is immune from the development of hemorrhoids. But you have the power to protect yourself from unpleasant symptoms.
Causes of hemorrhoids
The development of the disease is promoted by many reasons, including hereditary predisposition, excess weight, physical inactivity or bad habits. In addition, hemorrhoids often result from professional activities associated with prolonged exposure to one position (pilots, drivers, office workers, etc.). Various disturbances in the functioning of the intestines, caused by poor nutrition and abuse of spicy, fatty, fried foods, and fast food, are a provoking factor of the disease. In women, the disease most often progresses during pregnancy and childbirth, and in men, the development of the disease can be caused by a passion for strength training and lifting weights.
At the second stage of hemorrhoids, patients often seek medical help, because the disease brings significant discomfort and its symptoms can no longer be ignored.
Laser vaporization
Effective treatment of hemorrhoids is impossible without the use of laser vaporization.
LHP technology (laser submucosal destruction) is possible thanks to the use of equipment from. Advantages of laser vaporization:
- no injuries;
- no postoperative stitches;
- relief of inflammation during the recovery period;
- minimal exposure time to hemorrhoidal formation;
- short period of rehabilitation;
- reduction of relapses.
The essence of the technique is to evaporate the hemorrhoidal node with a laser.
The patient does not feel pain during the procedure and recovers quickly. The use of special proctological underwear and local anesthetics are additional means to create patient comfort during laser vaporization. How to stop hemorrhoids without pain and surgery? There is only one answer - to use the latest technologies to combat the problem.
Treatment of second stage hemorrhoids
For second-stage hemorrhoids, the doctor may treat it conservatively, or the doctor will suggest minimally invasive manipulations - sclerotherapy, ligatures (suture ligation or ligation with latex rings). The question of choosing the most effective therapy is decided individually after examining the patient.
In the acute phase of the disease, only conservative treatment is carried out. Drug treatment is aimed at relieving symptoms of the disease and reducing inflammation. Anti-inflammatory, wound-healing, analgesic, hemostatic suppositories and ointments that improve local blood flow are used locally.
Patients with hemorrhoids are prescribed a special diet to normalize intestinal function, and are also recommended to adjust their lifestyle, physical activity, normalize weight, and give up bad habits, which will help avoid relapse of the disease.
On the medical basis, diagnosis and treatment of all forms of hemorrhoids are carried out using modern methods of therapy in proctology. Modern diagnostic equipment and specialists with many years of experience guarantee impeccable treatment results.
You no longer need to endure pain and experience constant discomfort. Contact a multidisciplinary medical center and our specialists will solve your delicate problems as quickly, tactfully and painlessly as possible. You can make an appointment by phone: +7 or using the online registration form on the website.
Application of latex ligation
It is possible to eliminate hemorrhoids at the second stage of the disease using a low-traumatic and painless treatment method - latex ligation.
The essence of the technology is to throw special latex rings onto the base of the knot. This is done using a vacuum ligator. The device is placed in the area of the hemorrhoid and the vacuum pushes out a ring that compresses the lower part of the formation.
The nutrition of the hemorrhoid gradually stops and it is reduced and spontaneously exits. The ring is small in size, with an outer diameter of only five millimeters.
The hemorrhoidal node dies after latex ligation after 1-2 weeks. The ring and reduced formation are removed during natural bowel movements.
During this manipulation, which lasts only 15 seconds, the patient does not experience any discomfort or pain. The patient lies on the couch with his knees tucked to his stomach and can even communicate freely with the proctologist.
In agreement with the patient, the doctor uses local anesthesia.
Methods of treating the disease
Treatment of grade 2 hemorrhoids includes an integrated approach using drug therapy, auxiliary methods of traditional treatment, and minimally invasive surgical techniques. In addition, the patient needs to adjust his lifestyle, adhere to a certain diet, and perform physical exercises recommended by the attending physician. Second stage therapy is carried out more often at home after diagnosis and selection of the type of treatment for a particular patient.
Use of medications
Treatment of stage 2 hemorrhoids with medications involves the use of suppositories, ointments and oral medications, the action of which is aimed at reducing the symptoms of the disease and preventing complications.
When choosing a particular medicine, the doctor is guided by which symptom predominates in the patient.
Painkillers
In case of severe pain, a person is prescribed painkillers in the form of suppositories, ointments and tablets. These include:
- Anestezol suppositories - relieve pain and inflammation well, promote healing of anal fissures;
- Relief ointment - a drug based on shark liver oil, rarely causes side effects, copes well with most manifestations of hemorrhoids at all stages;
- Procto-Glivenol suppositories - the medicine relieves pain, promotes blood circulation in the pelvic organs, strengthens the walls of blood vessels, increases their elasticity. Candles are used in courses as prescribed by a proctologist;
- suppositories with adrenaline - used in patients with acute illness, have a powerful analgesic effect;
- Neo-Anuzol suppositories – have a bactericidal, anti-inflammatory effect, relieve pain, redness and swelling.
Procto-Glivenol perfectly eliminates unpleasant symptoms of the disease
In addition to drugs in the form of rectal suppositories, ointments are very popular. The following medications have a good effect:
- Heparin ointment – anesthetizes, relieves itching, redness, irritability;
- Proctosan ointment – contains bismuth, thanks to which the drug quickly eliminates pain and other manifestations of hemorrhoids;
- Levomekol is a safe drug that is prescribed to patients for the treatment of varicose veins in the rectal area, including after surgical removal of hemorrhoids.
Important! Painkillers for hemorrhoids should be used only on the recommendation of the attending physician; self-medication often causes serious consequences.
Anti-bleeding drugs
If the patient has a predominant sign of pathology such as bleeding, he may be prescribed the following medications:
- suppositories with propolis - stop bleeding due to the presence of propolis in its composition, which has a positive effect on blood clotting, preventing bleeding;
- Methyluracil ointment - the medicine stops bleeding and promotes the healing of anal fissures;
- Natalsid suppositories - used for mild or intense bleeding, help relieve the inflammatory process;
- suppositories with sea buckthorn oil - heal wounds and microdamages well, eliminate mild and moderate bleeding.
Natalsid suppositories are often prescribed to stop bleeding in grade 2 hemorrhoids.
Among oral medications, tablets are used: Detralex, Phlebodia, Hemoroidin and other drugs intended to strengthen blood vessels, treat bleeding and other signs of the disease.
Complications of hemorrhoids
Many patients associate the disease with only pain during bowel movements and bleeding, and therefore do not attach much importance to it in the early stages. Meanwhile, it is developing rapidly. And if yesterday everything was limited to discomfort when going to the toilet, tomorrow it may result in:
- Thrombosis and suppuration.
- Inflammation and swelling of the rectum.
- Formation of fistulas.
- Acute paraproctitis.
- Other diseases that cannot be cured without surgery.
Types of Hemorrhoids
Based on the location of hemorrhoidal cones, 3 types of disease are distinguished. These include:
- internal hemorrhoids - here cavernous formations are located above the dentate line under the mucous membrane of the rectum in the area of the internal venous plexus;
- external - bumps appear below the dentate line and are easily detected during external examination;
- combined – is a combination of internal and external forms of pathology.
There are internal, external and mixed hemorrhoids
External and internal hemorrhoids of the 2nd degree are diagnosed in a hospital setting. A preliminary diagnosis is made by a doctor through a visual and digital examination. To obtain additional data, methods such as anoscopy, irrigoscopy, sigmoidoscopy, X-ray and other types of examination may be needed.
Modern technologies in the treatment of chronic hemorrhoids
Goncharov D.Yu. Ph.D. Hemorrhoids are one of the widespread diseases of the adult population of industrialized countries. It has been established that in people over 40 years of age, symptoms of hemorrhoids are found in 60-70% of cases. Hemorrhoids account for about 40% of the structure of coloproctological diseases.
In recent years, minimally invasive methods of treating hemorrhoids have become firmly established in the daily practice of coloproctologists. The advantages of these methods over surgical interventions are the possibility of their use on an outpatient basis, without loss of ability to work; high efficiency in the initial stages of the disease; a small number of complications.
The most commonly used minimally invasive methods are:
- hardware ligation of hemorrhoids with latex rings,
- sclerotherapy,
- infrared photocoagulation of hemorrhoids,
- suture ligation of hemorrhoidal arteries under Doppler control,
- electrocoagulation of hemorrhoids.
The indication for minimally invasive surgical interventions is uncomplicated internal hemorrhoids of stages I - III.
When choosing a method of treating patients with hemorrhoids, it is advisable to use a classification that subdivides chronic hemorrhoids into stage IV.
- I Art. Discharge of scarlet blood from the anus without prolapse of hemorrhoids.
- II Art. Prolapse of hemorrhoids with self-reduction into the anal canal (with or without bleeding).
- III Art. Periodic prolapse of hemorrhoids and the need for their manual reduction into the anal canal (with or without bleeding).
- IV Art. Constant prolapse of hemorrhoids along with the rectal mucosa, inability to reduce them into the anal canal using a manual aid (with or without bleeding).
Contraindications include: a combination of hemorrhoids with an anal fissure, rectal fistula, inflammatory diseases of the anal canal and perineum, acute hemorrhoids.
Ligation of hemorrhoids with latex rings is the most commonly used technique (32-82%), and sclerotherapy, due to the frequent development of complications (11-47%), is used less and less. Other minimally invasive treatment methods are used in less than 5% of cases.
Ligation of hemorrhoids with latex rings
Blaisdell first developed and used a tool for applying a circular latex ligature to the pedicle of a hemorrhoid in 1954. Subsequently, other, more advanced models of ligators were developed.
The use of this method is indicated for internal hemorrhoids II, sometimes III degree. Contraindications for performing ligation of hemorrhoids are: a combination of internal hemorrhoids with an anal fissure and rectal fistula; acute hemorrhoids; inflammatory diseases of the anal canal; treatment with anticoagulants.
Direct ligation (clamping) of hemorrhoids occurs using a latex ring with an internal diameter of 1 mm, which has good elasticity and provides uniform, constant compression of the tissue. Rejection of the hemorrhoid along with the ligature occurs 5 to 9 days after manipulation. During this period, as a rule, there is a slight discharge of scarlet blood from the anal canal, which does not require the prescription of medications, since it stops on its own. A connective tissue scar forms at the site of the rejected hemorrhoid.
There are two main methods for ligating hemorrhoids. The first is based on drawing cavernous tissue into the sleeve of a mechanical ligator using a special soft clamp, after which one or two ligatures are dropped from the instrument onto the stem of the hemorrhoid. The ring should only compress the pedicle of the node, without capturing tissue located below the anorectal line.
The essence of the second method is to use a vacuum ligator, which is connected to a suction device. The working part of the instrument should be pressed tightly against the hemorrhoid. After turning on the suction, negative pressure is created in the device cylinder, and the assembly is gradually drawn into the ligator coupling. When the pressure reaches 0.7 - 0.8 atmospheres, two latex rings are dropped from the instrument onto the stem of the hemorrhoid.
During the first session, ligation of one or two hemorrhoids is performed. The next stage of treatment is prescribed no earlier than 15 days later.
If the technique is followed correctly, the patient should not experience severe pain. After the manipulation, slight pain, a feeling of pressure, a feeling of a foreign body in the rectum, and tenesmus may appear, which may persist for 1 to 2 days. These sensations can be relieved by taking non-narcotic analgesics.
Complications of ligation of hemorrhoids are: pain (noted if the manipulation is performed incorrectly), thrombosis of external hemorrhoids (occurs in 2-3% of patients), bleeding (observed in 1% of patients). The effectiveness of the technique is more than 80%.
Sclerotherapy
For the first time, sclerotherapy as a method of treating hemorrhoids was used by I.I. Karpinsky (Russia) in 1870, using iron persulfate and phenol for these purposes. However, frequently developing complications after such sclerotherapy have led to the limitation of the use of this method. With the advent of new sclerosing drugs, anoscopes, and special needles, interest in this technique has increased again.
In the Russian Federation, preparations from the detergent group are approved for use. These include: polidocanol-ethoxysclerol, thrombovar, fibrowein, sodium morruate, sodium tetradecyl sulfate. Detergents are the most effective and safe phlebosclerosing chemicals. The mechanism of action of this group of drugs is based on the ability to cause coagulation of endothelial proteins and desquamation of the epithelium. Detergents have a local effect on vascular tissue and do not lead to systemic thrombus formation.
The indication for sclerotherapy is internal hemorrhoids of stages I-II; continued bleeding from hemorrhoids.
Contraindications to this method include: external hemorrhoids, paraproctitis, thrombosis of hemorrhoids, ulceration of the mucous membrane, anal fissure.
The essence of the sclerotherapy technique is to introduce the drug into the thickness of the hemorrhoidal node, using a specially curved needle with a limiter. Depending on the size of the hemorrhoid, from 0.5 to 2.0 ml of detergent is administered.
On the first day after the procedure, a tissue reaction to chemical coagulation occurs and pain may develop. A pronounced pain reaction may be associated with the introduction of the drug not into the thickness of the hemorrhoid, but into the muscular layer of the intestine, as well as with the introduction of a concentrated sclerosing drug in a larger volume. In this case, thrombosis and necrosis of the mucous membrane of the hemorrhoidal node may occur.
In order to prevent the development of pain and inflammation, it is advisable to perform sclerosis of no more than two hemorrhoids in one session. The second stage of treatment is prescribed no earlier than after 2 weeks. During a follow-up examination on days 12-14 after the procedure, a flat, round, painless, sclerotic area of cavernous tissue with unchanged mucosa is determined in the anal canal.
Sclerotherapy for hemorrhoids is most effective for stage I hemorrhoids. As the stage of the disease increases, the number of good results decreases and the number of relapses increases. Sclerosing therapy does not allow achieving a radical cure of patients from the manifestations of hemorrhoidal disease, and good long-term treatment results are observed in only 20% of patients.
Infrared photocoagulation
With the beginning of the use of ultraviolet and infrared radiation in medicine, A. Neiger in 1978 proposed a technique for infrared photocoagulation of hemorrhoids. The method is distinguished by its simplicity and short exposure time. It is used in the initial stages of internal hemorrhoids, as well as to stop hemorrhoidal bleeding. Contraindications are external hemorrhoids, thrombosis of internal hemorrhoids, combination with paraproctitis and anal fissure.
The principle of operation of the photocoagulator is that the infrared light flux is focused and directed through the light guide into the cavernous tissue. The tip of the light guide transmits infrared light, which, penetrating the hemorrhoidal node, is converted into thermal energy. As a result, coagulation of submucosal structures occurs with the development of necrobiotic processes in the vascular endothelium, which leads to a decrease in blood supply to the cavernous tissue. The depth of necrosis depends on the duration of exposure.
The technique is carried out as follows. A photocoagulator tube is inserted into the anal canal through an anoscope. The tip presses the mucous-submucosal layer against the muscle layer and photocoagulation is performed. This effect is carried out at 3-4 points, at the stem of the hemorrhoid, leaving gaps between the coagulation zones. In this case, a defect with a diameter of 4-5 mm is formed on the mucosa with a zone of local coagulation necrosis, the depth of which extends to no more than 5 mm. A week after photocoagulation, a scab forms at the site of exposure, which is gradually replaced by connective tissue to form a scar.
It is advisable to carry out coagulation of no more than two hemorrhoids in one stage. The procedure is repeated after 2 weeks. Repeated courses of photocoagulation are possible.
Observation of patients and analysis of treatment results showed that this method is most appropriate to use in stage I of chronic hemorrhoids, as well as to stop hemorrhoidal bleeding.
Cryosurgical treatment
One of the minimally invasive methods of treating hemorrhoids is cold destruction. Cryotherapy is based on the rapid freezing of hemorrhoids with liquid nitrogen. The disadvantages of this method are: pronounced, uncontrolled swelling of the perianal tissues, a feeling of discomfort in the anal canal, pain, a weeping wound, as well as long recovery times. These manifestations are observed in more than 50% of patients. The limited use of this method is also due to the difficulty of controlling the boundary of the spread of cryotherapy, the danger of deep tissue necrosis, and the possibility of bleeding. In this regard, cryotherapy, as a method of treating hemorrhoids, has practically not been used in recent years.
Suture ligation of hemorrhoidal arteries under ultrasound Doppler control
A relatively new minimally invasive technique, which has not yet become widespread in our service market, is suture ligation of hemorrhoidal arteries under the control of Doppler ultrasound. This method is attractive due to its ease of implementation and targeted impact on the etiological factor in the development of hemorrhoids.
The method is based on the identification of hemorrhoidal arteries using Doppler ultrasound, followed by suturing and ligating them with a regular thread. This method was developed and proposed by the Japanese surgeon Morigana R. (1996)
For diagnostic Doppler testing, an ultrasonic surgical device with a sound transducer and an anoscope with an ultrasound sensor built into it are used. After installing this sensor over the hemorrhoidal artery, a light and sound signal is heard on the device. Through the incisura in the anoscope, above the internal hemorrhoidal node, the distal branch of the hemorrhoidal artery is sutured and ligated with a figure-of-eight suture. The criterion for correct ligation of the artery is the disappearance of sound and light signals. In the same way, hemorrhoidal arteries are ligated around the entire circumference of the rectum. This leads to interruption of excess blood supply to internal hemorrhoids and their fixation in the anal canal. This technique is most effective for stages I-III of hemorrhoids.
Contraindications are external hemorrhoids, thrombosis of hemorrhoids, inflammatory diseases of the anal canal, combination with paraproctitis and anal fissure.
A small number of complications include short-term retention of urination, a feeling of discomfort in the anal canal for 2-3 days after the procedure. However, it should be remembered that if the ligature is excessively tightened, the hemorrhoidal artery may erupt with the development of massive arterial bleeding. To prevent delayed arterial bleeding, it is advisable to stitch no more than 2 hemorrhoidal arteries in one session. Subsequent sessions are carried out 2 weeks after the first procedure. Suture ligation of hemorrhoidal arteries under Doppler ultrasound control may be a promising minimally invasive method for the treatment of hemorrhoids. However, to assess the effectiveness of this method, like other techniques, it is necessary to study the long-term results of treatment.
Electrocoagulation of hemorrhoids
One of the modern minimally invasive techniques is electrocoagulation of hemorrhoids. This method of treating patients with hemorrhoids was first proposed by A. Gain in 1939. The literature reports on coagulation of hemorrhoids using various devices such as AKM, Bicap, Ultroid, WD-II. All these devices are based on the principle of diathermic action of electric current, by conducting it through a conductor to the mucous-submucosal structures. Through thermal and chemical effects on cavernous tissue, necrosis occurs, followed by fibrosis and the formation of scar connective tissue.
The manipulation technique is quite simple. Depending on the type of device used, application electrocoagulation of the mucous membrane near the stem of the hemorrhoidal node (Bicap device) is performed, similar to the photocoagulation method. When using the WD-II device, the mucous membrane of the hemorrhoidal pedicle is pierced with the two-point electrode included in the kit to a depth of 0.5 cm, and when the device is activated, electrocoagulation of the cavernous tissue gradually occurs. The current strength is adjusted individually. The disadvantage of this method when using this device is the long exposure time of the electrode in one hemorrhoidal node (10-15 minutes). During this period of treatment, both the patient in the corresponding position and the doctor performing the procedure become tired. Therefore, in one session, it is possible to coagulate only one hemorrhoid.
Indications for this technique are internal hemorrhoids of stages I - II, and contraindications are acute hemorrhoids, paraproctitis, anal fissure.
According to domestic and foreign researchers, treatment of hemorrhoids using electrocoagulation allows one to obtain good results only in patients with stages I - II of hemorrhoids.
In conclusion of this section, it should be said that the accumulated personal experience of using various minimally invasive techniques, observation of patients and analysis of long-term results of treatment of such patients has shown that these techniques are most effective in the initial stages of hemorrhoids. In stages IV and III of the disease, it is advisable to use a surgical treatment method. Minimally invasive techniques in late stages of hemorrhoids can be used to stop hemorrhoidal bleeding, which can be the first stage of further radical treatment of such patients, as well as in elderly, somatically burdened patients with palliative purposes. In our opinion, no more than 10-15% of patients diagnosed with chronic hemorrhoids can be radically cured using minimally invasive methods. However, the combination of various methods makes it possible to expand the indications for their use. Of course, the positive side of minimally invasive techniques is their ease of use, a small number of complications, low trauma, good tolerability of the procedure, and the possibility of using them on an outpatient basis, which is economically beneficial in modern conditions of insurance medicine.
Surgery
Currently in Russia, the most common method of treating hemorrhoids is hemorrhoidectomy. Most coloproctologists and surgeons in our country use a technique aimed at excision of the main collectors of cavernous tissue, proposed by Milligan E. and Morgan G. in 1937. This operation is used in two modifications. Some doctors use closed hemorrhoidectomy, when after excision of the hemorrhoid, suturing and ligation of the vascular pedicle, the mucous membrane is sutured tightly. Other coloproctologists use an open technique, without restoring the integrity of the rectal mucosa, leaving a solid mucocutaneous strip of tissue between the excised hemorrhoids. Each modification has its own advantages and disadvantages. In connection with the development of new technologies and the development of modern devices, they began to be used when performing hemorrhoidectomy, in order to reduce the number of postoperative complications and reduce the recovery time for patients after surgery. The most commonly used are the ultrasonic harmonic scalpel, the LigaSure electrothermal system, and the radio wave scalpel. In recent years, the method of circular resection of a section of the muco-submucosal layer of the distal rectum using a circular stapler (Longo method) has become widespread.
Ultrasonic harmonic scalpel
This method in our country began to be used in the practice of surgical treatment of hemorrhoids relatively recently, but immediately attracted attention. The operating principle of a harmonic scalpel differs from other electrosurgical devices in that it is based on a high frequency of vibration of the working blade in the longitudinal direction. This allows for simultaneous coagulation and dissection of tissue through mechanical cutting, cavitation and temperature effects. The installation allows you to reliably coagulate vessels up to 5 mm in diameter. It is important to note that in this case, a strictly targeted effect on tissue occurs, and the depth of thermal damage to adjacent structures does not exceed 1.5 mm, which distinguishes this device from electrocoagulators.
When performing hemorrhoidectomy using an ultrasonic scalpel, the first stage is dissection of the perianal skin using an electrocoagulator and separation of the external hemorrhoid from the fibers of the subcutaneous portion of the external sphincter. Then, using the coagulation and cutting mode, the external and internal hemorrhoids are excised en bloc. The vascular pedicle is treated only in coagulation mode. The remaining hemorrhoids are removed in a similar way. The wounds are not sutured, but left open.
Reliable coagulation and virtually bloodless excision of hemorrhoids allows reducing the time of surgical intervention. Shallow thermal damage to tissue leads to a decrease in pain response in the postoperative period. All this has a positive effect on the incidence of dysuric disorders and reduces the postoperative rehabilitation period for patients.
Hardware-controlled bipolar electrocoagulation
Designed for bipolar electrocoagulation and vascular division, the LigaSure electrothermal system delivers controlled energy to the jaws of the clamp. As a result, denaturation of collagen and elastin occurs in the tissues with the formation of a zone of coagulative necrosis. In addition, the clamp mechanically compresses the tissues, to which electric current is dosed. The strength of the treatment zone, consisting of partially denatured protein, is comparable to the strength of stitched fabric. In this regard, there is no need to isolate and additionally ligate the vascular pedicle of the hemorrhoid. The whole process takes about 5 seconds. The device allows you to coagulate vessels up to 7 mm in diameter. The depth of thermal effect on tissue, according to the characteristics, is 2 mm.
The LigaSure electrothermal system allows hemorrhoidectomy to be performed almost bloodlessly, without using suture material. At the same time, the operation time is significantly reduced. However, in some patients, in the immediate postoperative period, a fairly intense pain reaction develops, which may be associated with a deep thermal effect on the tissue of the anal canal. In this regard, this device, in our opinion, is most appropriate to use for hemorrhoidectomy of large hemorrhoids.
Radio wave scalpel
Some researchers suggest using a radio wave scalpel for hemorrhoidectomy, which has proven itself in cosmetic surgery.
The device emits a radio wave, which causes the formation of heat in the tissues, under the influence of which the breakdown of cellular structures occurs and tissue separation occurs. In this regard, the device has good dissection properties. Thermal damage to tissue is minimal, which creates optimal conditions for wound healing. However, the hemostatic properties of a radio wave scalpel are low, especially in the presence of biological fluids, which does not allow the use of this device alone (without an electrocoagulator) to perform hemorrhoidectomy.
Operation Longo
This operation differs from other methods of surgical treatment of patients with hemorrhoids in that the hemorrhoids are not removed. Due to circular excision of a section of the mucous membrane of the distal rectum, using a circular stapler, the hemorrhoids are proximally tightened and fixed in the anal canal. In this case, the terminal branches of the hemorrhoidal arteries are crossed, which leads to a significant decrease in the blood supply to the cavernous plexuses. All this determines the relief of clinical manifestations of hemorrhoids after this operation. The method was proposed in 1998. Italian surgeon A. Longo.
Indications for this type of surgical intervention are grade III-IV hemorrhoids. with loss of nodes, but without a pronounced external component, as well as relapse of the disease. Contraindications: inflammatory diseases of the anal canal and perineum, rectal fistula, prolapse of only one hemorrhoid.
The advantage of hardware hemorrhoidopexy is low trauma and short duration of the operation, mild postoperative pain syndrome, and short rehabilitation time for patients. However, it should be mentioned that in some patients, intense hemorrhage was noted in the postoperative period, requiring reoperation.
Despite the widespread use of this technique abroad, in Russia this operation is performed relatively rarely. Limiting factors are the high cost of the device and the lack of data on long-term treatment results. Of course, it is necessary to have information about what happens to the remaining hemorrhoids in long-term follow-up. It remains unclear whether revascularization of the remaining cavernous tissue occurs after a few years, whether the fixation of hemorrhoids in the anal canal is reliable, or whether the clinical manifestations of the disease will return in the long-term follow-up period.
So, the modern possibilities of surgical treatment of patients with chronic hemorrhoids are significant. The arsenal of methods for treating this common disease is large. It is impossible to adapt any one treatment method available in the clinic to all stages of hemorrhoids. It is necessary to skillfully determine the indications for treatment and, depending on the stage of the disease, choose the most appropriate method. It should be remembered that minimally invasive treatment methods, which patients readily agree to, especially those used on an outpatient basis, are most effective in the initial stages of hemorrhoids. When the stage of the disease increases, as well as when hemorrhoids are combined with other diseases of the anal canal and pararectal tissue, surgical treatment is indicated.
Internal hemorrhoids: treatment and diagnosis
The only sure way to get a complete picture of the disease is a comprehensive diagnosis. It includes a proctological examination, endoscopic examination, laboratory and clinical studies of the intestinal walls and feces.
Treatment can be divided into 2 types of therapy. Conservative involves taking venotonic drugs with angioprotective properties. In more severe stages, medications will not bring the desired effect, but will only remove symptoms. In such cases, it would be advisable to choose an operational method to solve the problem:
- Sclerotherapy;
- Hemorrhoidectomy;
- Laser vaporization;
- Ligation with latex rings.
“Phlebodia 600” is a treatment for internal hemorrhoids and varicose veins of the lower extremities, which can reduce the symptoms of the disease, tone the vessels and normalize blood flow in the affected vein. You can find out about the medicine in more detail and get advice from a phlebologist on our website in a special window.
Causes
The main reason for the development of internal forms of hemorrhoids is a violation of the inflow and outflow of blood in the cavernous (cavernous) bodies. In a healthy person, these corpuscles fill with blood when the intestines are filled with feces, which causes them to increase and makes it easier to control the urge to defecate. After successful bowel movement, blood flows out and the cavernous bodies shrink.
If the regulation of outflow is disrupted and the cavernous bodies are constantly in an increased size, then over time this leads to varicose veins and thinning of the venous vessels. The main causes of blood outflow disorders traditionally include the following factors:
Relevance of the problem
Although published data on the prevalence of hemorrhoidal disease among populations in developed countries vary, 1,2 it can be said that it is one of the most common diseases in surgical practice. In the United States, more than 2.2 million new cases are diagnosed as outpatients each year3. There is a wide variety of clinical symptoms that can be misinterpreted by doctors and patients as a manifestation of hemorrhoidal disease. Thus, it is necessary to determine exactly what hemorrhoids are causing the symptoms before starting treatment for the disease. These recommendations are devoted to both diagnostic methods and modern approaches to the treatment of hemorrhoids.
Desarterization
Termination of access of arterial blood supply to the hemorrhoidal node is the main goal of disarterization. Treatment of hemorrhoids is carried out by “flashing” the arteries that supply the node.
From two to six arteries are sutured by a proctologist using special, state-of-the-art equipment. The coloproctologist learns about the detection of a hemorrhoidal node by the signal that comes from the Doppler, a special sensor placed in the anal canal.
The doctor does the firmware through the anoscope, or more precisely, through its side window. The manipulation lasts up to half an hour, and the patient then needs up to two hours to recover. The procedure is done without general anesthesia.
In the day hospital, the patient is observed for one to two hours after treatment. One procedure is enough to obtain effective treatment for hemorrhoids using the disarterization method.
Identifying the source of rectal bleeding
1. Endoscopic examination of the colon is indicated in selected patients with symptomatic hemorrhoids and rectal bleeding. Recommendation level IV.
Although hemorrhoidal disease is the most common cause of blood in the stool (hematochezia), there are many diseases, such as colorectal cancer, inflammatory bowel disease, various types of colitis, diverticular disease, and angiodysplasia, that can also cause bleeding.7 In most patients with colon cancer are not the cause of hematochezia, yet many doctors neglect this symptom and miss the opportunity to diagnose the tumor.8
Personal and family history, as well as physical examination, which may include proctoscopy and/or flexible sigmoidoscopy, will identify high-risk patients who require a more thorough diagnostic search. Previous endoscopic records should be reviewed whenever possible. Table 2 outlines the criteria for patients who should undergo a full colon examination using colonoscopy or another method of screening for colorectal cancer.9 If colonoscopy is not possible for one reason or another, flexible sigmoidoscopy should be considered in combination with other diagnostic methods given in the recommendations on colorectal cancer screening.10