Occlusion of the subclavian artery is an atherosclerotic lesion of one of the most important arteries of the body.
The process of development of occlusion (literally “closing”) of the subclavian artery is accompanied by the deposition of cholesterol and fat cells in its walls, the proliferation of connective tissue (sclerosis), and the deposition of calcium salts (calcification). This leads to the formation of the so-called. plaques - pieces of tissue that seem to stand across the path of blood flow.
This process leads to a narrowing of the subclavian artery, which in turn contributes to the development of cerebrovascular insufficiency and ischemia (that is, insufficient blood supply) of the upper extremities. The development of atherosclerosis also threatens with more serious consequences, since the detachment of plaques from the walls of the artery can cause blockage of blood vessels, which can also lead to death.
Occlusion of the subclavian artery is not an independent disease, but is a consequence of atherosclerotic changes in the arteries (overgrowth of connective tissue and plaque formation) and stenosis (narrowing of the walls of blood vessels).
Symptoms
The main role among developing disorders belongs to ischemia of tissues that are supplied with blood from the subclavian vessel.
Symptoms of the first stage of blood supply failure:
- increased sensitivity to cold;
- a feeling of chilliness and numbness appears;
- paresthesia;
- are formed by vasomotor reactions.
Symptoms of the second stage of blood supply failure:
- weakness;
- pain appears;
- numbness;
- the hands, fingers and forearm muscles become cold.
Symptoms of the third stage of blood supply failure:
- constant coldness and numbness of the hands;
- muscle wasting;
- decreased muscle strength;
- inability to perform subtle and precise movements with the fingers.
Symptoms of the fourth stage of blood supply failure:
- cyanosis and swelling of the phalanges;
- cracks and trophic ulcers develop, which turn into necrosis and gangrene of the phalanges.
- Thrombosis and cerebral ischemia contribute to the rapid development of the disease. The result may be acute ischemic stroke.
Symptoms of closure of the lumen of the first segment:
- dizziness, frequent headaches;
- vestibular ataxia and hearing loss;
- visual disturbances;
- ischemia of the upper extremities;
- coronary-mammary-subclavian steal syndrome.
Symptoms that are characteristic of any type of pathology:
- loss of consciousness;
- paresis;
- swallowing and speech disorders;
Causes of the disease
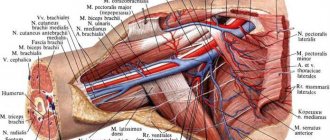
To function properly, blood vessels and nerves need a certain amount of space. Compression of the vessels in the costoclavicular space can lead to injury or, in rare cases, loss of a limb. In order for nerves and blood vessels to function properly, they need adequate space. When compression occurs, their function is accordingly impaired. Compression of the blood vessels at the outlet of the chest can impair blood flow to and from the arm. It can also promote the formation of a blood clot, which can further slow or completely block blood flow through the damaged vessel. If a clot ruptures, it can travel down into the arm, blocking small blood vessels in the arm. Sometimes, the clot migrates to the lungs, a life-threatening condition called pulmonary embolism. Nerves also need space to be able to stretch when the arm moves. If the nerve as it exits the chest wall is compressed or cannot move freely, the patient will not be able to move the arm as normal. Pain and sensory disturbances in the hand often accompany this condition.
Risk factors for scalene muscle syndrome (SMS):
- Gender – Women are more likely to have SLM syndrome than men.
- Age – The syndrome most often develops between the ages of 20-50.
- Diseases - SLM - syndrome is often associated with another disease, such as damage to the rotator cuff, osteochondrosis of the cervical spine, injury to the brachial plexus, diabetes mellitus, hypothyroidism.
Diagnostics
To begin with, a physical examination is performed. To do this, you need to make an appointment with a cardiologist. In case of visual impairment, consultation with an ophthalmologist is necessary. To confirm the diagnosis, the doctor prescribes the following:
- Doppler ultrasound;
- duplex scanning of all vessels of the upper limb;
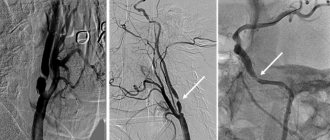
- peripheral arteriography;
- X-ray contrast angiography;
- rheovasography;
- thermography;
- sphygmography;
- magnetic resonance angiography;
- peripheral CT arteriography;
- MSCT angiography.
Symptoms
Symptoms of SLM vary depending on whether the blood vessels or nerves are compressed.
Symptoms of nerve compression
- Pain or tenderness in the neck, shoulder, arm
- Numbness or tingling in the neck, shoulder, arm
- Muscle weakness or areas of muscle failure in the arm
- Difficulty performing fine motor tasks; fast fatiguability
Arterial Compression Symptoms
- Swelling of the hand
- Pain or deep tenderness in the neck, shoulder, or arm
- Numbness, tingling, or heaviness in the arm
- Changes in skin color - the hand or fingers turn pale
- Changes in skin temperature – the arm or fingers are cooler than the rest of the skin
- Small black spots on fingers
- Weak or absent pulse in the arm
- Pulsating tumor in the collarbone area
Venous Compression Symptoms
- Swelling of the hand
- Pain or deep tenderness in the neck, shoulder, or arm
- Numbness, tingling, or heaviness in the arm
- Changes in skin color - the hand or fingers become blue
- Seal in the area of the subclavian vein
- Visually noticeable venous network on the chest.
Prevention
Measures to prevent the development of occlusion of the subclavian artery are aimed at preventing diseases that cause this pathology. They consist of giving up smoking and other bad habits, eating right (especially excluding fried and fatty foods), regularly monitoring blood pressure and preventing stress and traumatic situations.
Occlusion of the subclavian artery is accompanied by complete blockage of the lumen of this blood vessel and insufficient blood supply to the brain and upper extremities. This pathology can lead to a significant deterioration in performance, stroke and disability. If there are pronounced signs of occlusion of this artery, the patient is indicated for surgical treatment aimed at restoring its patency.
Complications
For a long time, some patients reflexively react to pain with muscle fixation. They have to hold a rigid certain position in order to reduce pain. But, unfortunately, this reflex muscle defense aggravates the course of the disease and, ultimately, leads to increased pain. Muscle defence, in turn, then requires separate treatment. It is important to begin treatment for SLM in its early stages. If left untreated, SLM can cause significant nerve or vascular damage, including limb loss.
Treatment
Conservative therapy for occlusion of the subclavian artery turns out to be ineffective, and with pronounced signs of blockage of this vessel, patients are recommended to undergo surgical treatment aimed at restoring its patency. Indications for intervention are severe symptoms:
- subclavian-vertebral steal;
- vertebrobsillar insufficiency;
- hand ischemia.
To eliminate occlusion, the following types of angiosurgical correction can be performed:
- Endovascular operations (stenting, dilatation, ultrasound or laser recanalization followed by angioplasty and stenting). These interventions are minimally invasive and are performed under local anesthesia. During the operation, a catheter is inserted into the lumen of the artery and delivered to its affected segment. The vascular surgeon can then install a stent. If it is impossible to pass the blockage zone with a soft catheter, ultrasound or laser recanalization is used, after which a stent or angioplasty is installed.
- Bypass surgery (aorto-subclavian, carotid-axillary, carotid-subclavian, cross subclavian-subclavian). The essence of such vascular operations is to create additional blood flow channels that bypass the affected area. Such shunts are created using vascular prostheses. Shunt operations are effective at any stage of occlusion.
- Plastic surgeries (resection followed by prosthetics, endarterectomy, implantation of the subclavian artery into the common carotid). The goal of these types of vascular interventions is to create new blood delivery routes by connecting the blocked vessel to the carotid artery. In some cases, part of the affected vessel is removed and replaced with a prosthesis made of synthetic materials.
Each of the above-mentioned vascular surgery techniques has its own indications and contraindications, advantages and disadvantages. That is why a surgical treatment plan is drawn up only after assessing all the data from diagnostic studies and taking into account the patient’s concomitant diseases.
Possible complications of surgical treatment
One of the symptoms of this pathology is headache.
The complex anatomical structure of the neck and the extreme susceptibility of the brain to insufficient blood supply mean that angiosurgical treatment of occlusion of the subclavian artery can lead to the following complications during or after surgery:
- stroke;
- cerebral edema;
- swallowing disorder;
- lymphorrhea;
- plexitis;
- pneumothorax;
- paresis of the dome of the diaphragm;
- damage to the sympathetic trunk, leading to Horner's syndrome;
- bleeding.
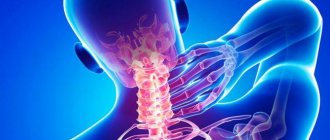
What is extravasal compression of the vertebral artery?
To answer the question of what extravasal compression of the vertebral artery is, you should understand this complex term step by step.
“Compression” in medicine means “squeezing something,” in this case the vertebral artery. The vertebral arteries pass through the intervertebral foramina of the cervical vertebrae towards the spinal canal, where they supply the spinal cord. Compression of the vertebral artery is not an independent disease, but rather a consequence of the development of another pathology.
Most often, this pathology is an intervertebral hernia. It is the resulting hernia that can compress the vertebral artery, thereby disrupting the blood supply to the spinal cord. Extravasal compression of the vertebral arteries is usually localized in the area of the 4th-5th vertebrae.
Links[edit]
- Labropoulos, N; Nandivada, P; Bekelis, K. (July 2010). "Prevalence and impact of subclavian steal syndrome". Annals of Surgery
.
252
(1):166–70. DOI: 10.1097/SLA.0b013e3181e3375a. PMID 20531004. S2CID 2165442. - ^a b Potter, B.J.; Pinto, D.S. (June 3, 2014). "Subclavian steal syndrome". Circulation
.
129
(22):2320–3. DOI: 10.1161/CIRCULATIONAHA.113.006653. PMID 24891625. - Meumann, E.M.; Chuen, J; Fitt, G; Pepper, Y; Pond, F; Dewey, H. M. (May 2014). "Thromboembolic stroke associated with thoracic outlet syndrome." Journal of Clinical Neuroscience
.
21
(5):886–9. DOI: 10.1016/j.jocn.2013.07.030. hdl: 11343/123833. PMID 24321459. S2CID 41769069. - Roldan-Valadez, E; Hernandez-Martinez, P.; Osorio-Peralta, S; Elizalde-Acosta, I; Espinoza-Cruz, V; Casian-Castellanos, G (September 2003). "Imaging diagnosis of subclavian steal syndrome secondary to Takayasu arteritis affecting the left subclavian artery." Archive of Medical Research
.
34
(5): 433–8. DOI: 10.1016/j.arcmed.2003.06.002. PMID 14602512. - Saalouke, M. G.; Perry, L. W.; Breckbill, D. L.; Shapiro, S.R.; Scott LP 3rd (July 1978). “Cerebrovascular abnormalities in postoperative coarctation of the aorta. Four cases demonstrating left subclavian bone steal on aortography.” American Journal of Cardiology
.
42
(1):97–101. DOI: 10.1016/0002-9149 (78) 90991-8. PMID 677042. - Kurlan, R; Krall, R.L.; Deweese, J. A. (March 1984). “Vertebrobasilar ischemia after total repair of tetralogy of Fallot: the significance of the subclavian steal created by the Blalock-Taussig anastomosis. Vertebrobasilar ischemia after correction of tetralogy of Fallot." Stroke
.
15
(2): 359–62. DOI: 10.1161/01.str.15.2.359. PMID 6701943. - Dig, K.H.; Hofbeck, M; Singer, H (December 1993). "Diagnosis of subclavian steal in infants with aortic coarctation and aortic arch interruption using color-coded Doppler sonography". Journal of Ultrasound in Medicine
.
12
(12): 713–8. DOI: 10.7863/jum.1993.12.12.713. PMID 8301709. S2CID 42139662. - Klingelhöfer J, Konrad W, Benecke R, Frank W (1988). "Transcranial Doppler sonography of the carotid-basilar collateral circulation in subclavian theft". Stroke
.
19
(8): 1036–42. DOI: 10.1161/01.STR.19.8.1036. PMID 3041649. - Lord, R., Adar, R., Stein, R. (1969). "Contribution of the Circle of Willis to subclavian steal syndrome". Circulation
.
40
(6):871–8. DOI: 10.1161/01.CIR.40.6.871. PMID 5377222. - Takacs T, Reul G, Cooley D, Duncan J, Livesey J, Ott D, Gregoric I (2006). "Myocardial theft: coronary subclavian steal syndrome." Ann Thorac Surg
.
81
(1):386–92. DOI: 10.1016/j.athoracsur.2005.05.071. PMID 16368420. - ↑
Lee S, Jeong M, Rhew J, Ahn Y, Na K, Song H, Bom H, Cho J, Ahn B, Park J, Kim S, Kang J (2003).
"Simultaneous coronary-subclavian and vertebral-subclavian steal syndrome". Circ
J.
67
(5): 464–6. DOI: 10.1253/circj.67.464. PMID 12736489.