General description of the disease
This is a painful condition during which the level of platelets in the blood falls below normal (less than 150,000 per 1 milliliter of blood). Due to this decrease, bleeding increases and there may be serious problems stopping bleeding.
Causes and forms of thrombocytopenia
Thrombocytopenia can be congenital or acquired. The most common form of the disease is the acquired form.
The acquired form of the disease comes in different types, which are distinguished depending on the causes of occurrence. Thus, thrombocytopenia can be:
- immune (the most common type, in which antibodies pass from a pregnant woman to her fetus);
- formed when cells located in the bone marrow are inhibited;
- consumption thrombocytopenia, which occurs in the presence of thrombosis and due to extensive hemorrhages;
- thrombocytopenia resulting from the transformation of bone marrow into a tumor;
- a decrease in the level of blood clots, which occurs due to mechanical damage to platelets that occurs with hemangioma.
The hereditary form includes diseases with abnormal damage (defects) to platelet membranes, which cause disturbances in their functioning.
The main factors contributing to the development of thrombocytopenia are: allergies to drugs (allergic or drug thrombocytopenia), infections and intoxications of the body provoke the development of symptomatic thrombocytopenia (causes of development include HIV, herpes, hepatitis, infectious mononucleosis, influenza, acute respiratory infections, rubella, chickenpox , systemic lupus). Additionally, Gaucher disease can cause low platelet levels.
There is also an idiopathic type of this disease. In this case, the cause of thrombocytopenia cannot be identified.
Symptoms of thrombocytopenia
The main signs of this problem are bleeding gums, constant and heavy bleeding from the nose, the appearance of bruises on the body and limbs for no apparent reason, difficult to stop bleeding after tooth extraction or with minor damage to the skin, blood streaks in the discharge, when urinating or defecation, heavy bleeding in women during menstruation, rash on the body and legs (the rash appears in the form of small red dots).
Also, hemorrhages may appear on the face and lips. This may indicate a cerebral hemorrhage.
Diet
Dietary ways to increase white blood cells in the blood if they have fallen include proper balanced nutrition and consumption of foods that promote production.
The menu must include products with vitamin C, E, potassium, Omega-3, and zinc. Recommendation: After chemotherapy you need to consume protein, otherwise it is more difficult for the body to cope. Products that increase the level:
- Drink liquid. The recommended intake for an adult is two liters of clean water per day. It is imperative to boil it before use.
- Berries and fruits containing vitamin C.
- Fiber found in vegetables.
- Dietary white meat.
- Eggs.
- Fish, seafood.
- Vegetable fats: nuts.
- Cereals, cereals, legumes.
Tips: vitamin A. The main useful vitamin needed by a convalescent person, its essence is to increase white blood cells. It is found in orange fruits, vegetables, and salmon. Vitamin C to support immunity is found in citrus fruits.
Prohibited foods include: fatty foods, smoked, spicy, canned. Eliminating these foods from the body will facilitate the healing process.
The danger with low levels of immunity consists of insufficiently washed fruits and vegetables that contain parasite eggs, infection, and bacteria. Undercooked meat is also dangerous. Due to reduced resistance, these products will lead to additional diseases and complications
Therefore, it is important to follow preventive measures, thoroughly wash products, and heat-treat them. Maintain hand hygiene
Diet for the third blood group
Weight gain in people with this immunogenetic trait is provoked by the following products:
- corn;
- wheat;
- buckwheat;
- tomatoes;
- peanut;
- sesame.
They affect metabolism by retaining fluid in the body, causing fatigue and hypoglycemia (a sharp decrease in blood sugar levels). Maintaining normal glucose levels is the key to preventing overeating.
Also, people with blood type O should avoid chicken, which contains agglutinating lectins in the breast. This circumstance increases the risk of strokes and immune disorders. Dr. D'Adamo suggests eating lamb, rabbit and game instead of chicken.
To lose weight you need to consume:
- green vegetables;
- eggs;
- healthy meat (except chicken);
- low-fat dairy products.
By maintaining food balance, it is easier for people with blood type 3 to maintain a healthy weight.
How to increase platelets in the blood at home?
With a slight decrease in platelet levels associated with a vegetarian diet, physiologically heavy menstruation, etc. Vitamin therapy and diet may be prescribed. However, it is necessary to understand that a pronounced decrease in platelet levels cannot be treated with diet. In this case, the prescription of thrombocytopoiesis stimulants is required.
At the same time, such herbal preparations as: extract of shepherd's purse, nettle, yarrow, water pepper, etc. do not stimulate platelet maturation in the bone marrow.
These plant extracts contain vitamin K, which is necessary for the synthesis of prothrombin, which is also involved in the process of blood clotting.
They are also able to enhance the ability of platelets to form a platelet thrombus.
Diet for low platelet levels
The diet for thrombocytosis is aimed at providing the body with the necessary vitamins, microelements, sufficient amounts of protein, etc. However, it cannot be considered as a stimulator of platelet production in the bone marrow. Adequate nutrition helps restore hemoglobin levels, reduce the severity of symptoms of anemia, normalize vascular permeability, etc.
The patient's diet should be balanced, easily digestible and nutritious. Consumption of animal protein is strictly necessary. A vegetarian diet is one of the risk factors for the development of thrombocytosis.
It is recommended to increase the consumption of boiled fish, chicken, quail, rabbit, turkey, liver, kidneys, eggs, seafood, hard cheeses, etc.
You should also increase the consumption of buckwheat and rice cereals, legumes, fresh herbs, vegetables and fruits, pomegranates, figs, nuts, etc.
Additionally, it is recommended to take multivitamin complexes containing B vitamins, zinc, iron, ascorbic acid, vitamin A, etc.
Patients should stop drinking alcohol, smoking, and also limit the consumption of strong tea, coffee, sweets, fatty, fried, spicy, salty and smoked foods.
Also, patients are advised to do dosed physical activity (walking), spending time in the fresh air, proper rest, etc.
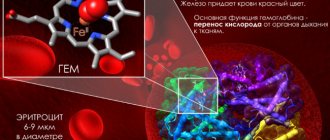
Why is low hemoglobin dangerous?
A low level of hemoglobin in the blood causes anemia, or anemia, a condition in which cellular oxygen supply is disrupted. Anemia may indicate the presence of a disease or occur due to poor lifestyle choices.
Anemia is a condition caused by a lack of oxygen in cells. It may be a marker of a serious illness. A person suffering from anemia has pale skin, decreased appetite, is prone to insomnia, frequent mood changes and nervous breakdowns.
The onset of anemia may be facilitated by the following non-genetic factors:
- presence of bad habits: excessive alcohol consumption, smoking, “sedentary” lifestyle;
- unhealthy diet: lack of vital elements in food;
- poor ecology: living in large cities, near unfavorable structures;
- lack of physical activity;
- stress.
All of the above circumstances are subject to human desire. First of all, to treat anemia it is necessary to give up bad habits, including those related to poor nutrition.
Eating right means, firstly, including in your diet foods that contain all the elements necessary, including maintaining the level of hemoglobin in the blood at the desired level.
Secondly, this means providing a systematic approach to nutrition, ensuring food intake at the same time every day, taking into account the individual characteristics of food absorption by the body.
Reasons for the decrease in platelets during cancer treatment
The most common cause of thrombocytopenia in patients undergoing cancer treatment is bone marrow suppression (or myelosuppression). Unfortunately, chemotherapy affects not only cancer cells, but also all cells dividing in the body, as a result of which the production of platelets by the bone marrow is inhibited.
In addition to thrombocytopenia, bone marrow suppression during chemotherapy can result in low red blood cell counts (chemotherapy-induced anemia) and white blood cell counts (chemotherapy-induced neutropenia).
Related article: Nadir, as the most common side effect of chemotherapy
Drugs
The use of most chemotherapy drugs does not lead to a serious decrease in platelet levels that require correction. Thrombocytopenia usually occurs with the use of the following chemotherapy drugs:
- Paraplatin (carboplatin)
- Platinol (cisplatin)
- Gemzar (gemcitabine)
- Taxol (paclitaxel)
How long does thrombocytopenia last?
Chemotherapy-induced platelet reduction is usually a short-term problem. Platelet levels begin to fall about a week after chemotherapy and reach their lowest level (nadir) about 14 days after the administration of cytotoxic drugs.
Platelets in the blood live for approximately 8 to 10 days, their number is quickly restored. It takes approximately 28 to 35 days to return to normal (assuming no further cycle of chemotherapy), and it may take up to 60 days to reach pre-treatment levels.
Other causes of low platelets in cancer
In addition to chemotherapy, there may be other reasons for platelet decline in cancer patients. For example:
- Immune thrombocytopenia (idiopathic thrombocytopenic purpura, Werlhof's disease) is a condition in which the body's immune system attacks and destroys platelets, resulting in thrombocytopenia. This most often occurs in Hodgkin's lymphoma and chronic lymphocytic leukemia.
- Viral infection.
- Certain medications, such as vancomycin and antiviral drugs.
- Metastatic bone marrow lesions (most often found in lymphoma, breast and lung cancer).
- Thrombotic microangiopathy: a condition in which the vascular endothelium (the lining of blood vessels) is damaged, sometimes with chemotherapy drugs such as mitomycin C and gemcitabine.
Nutrition for thrombocytopenia in adults to increase platelets. Nutrition for thrombocytopenia
It will be possible to increase the number of platelets using diet and folk remedies even with low levels in the blood, if you compensate for the lack of nutrients in the body such as vitamins C, K, B9, minerals calcium, iron, zinc.
The reason for the drop in platelets may be not only a lack of nutrients for the synthesis of new cells, but also a violation of the absorption of vitamins and minerals in the small intestine.
How to eliminate vitamin deficiency
A decrease in platelets is caused by a lack of vitamin C. 300 - 400 g of fresh herbs and fruits daily will help fill the deficiency. Quantitatively, this corresponds to two tangerines, an orange, two servings of a salad of tomatoes, cucumbers, and herbs.
Buckwheat, asparagus, spinach, green onions, tomatoes, beets will help increase vitamin B9 reserves in the body. Folic acid is a stimulator of thrombopoiesis - platelet production.
This vitamin is one of the most important for the production of new blood platelets. Just remember that folic acid is destroyed during heat treatment.
Vitamin K, known as an antihemorrhagic, helps increase the number of platelets in the blood. This compound is involved in blood clotting; if it is deficient, the prothrombin time, an indicator of blood clotting, lengthens.
The antihemorrhagic vitamin is synthesized by intestinal microflora and is supplied with food, but its absorption in the intestine may worsen due to inflammation of the gallbladder. The dinner table should include cabbage, spinach, eggs, liver, broccoli, kelp and other foods containing vitamin K.
How to compensate for mineral deficiencies
Calcium is required for platelet production. This macronutrient is found in sufficient quantities in dairy products.
There are conflicting opinions regarding the use of dairy products to increase blood platelets in thrombocytopenia. There is evidence that dairy products can increase the rate of autoimmune processes
This means that in case of autoimmune thrombocytopenia, dairy products should be used with caution.
For hematopoiesis, it is necessary to obtain sufficient amounts of iron from food. This mineral is found in meat, offal, dried mushrooms, pumpkin seeds, chicken egg yolk, brewer's yeast, and cocoa.
The diet should contain omega-3 acid, which is abundant in fatty fish, eggs, and flaxseed oil.
But in this regard, it is important not to overdo it. Excess omega-3 prevents platelet aggregation (sticking together), which increases bleeding and the risk of internal bleeding
Diet features
The diet should contain foods that increase platelets in the blood:
- rabbit, turkey, beef;
- offal - liver, kidneys;
- white fish;
- buckwheat;
- whole grain;
- legumes – peanuts, beans;
- nuts – hazelnuts, walnuts, almonds, pine nuts.
The diet should contain sources of vitamin C, which is abundant in leafy greens, fruits, and vegetables. Carrots, green apples, lingonberries are useful. Drinking green tea is useful for raising platelets.
Eating 2 kiwi fruits daily will help increase the number of blood platelets in conditions such as anemia, infection, vitamin B deficiency.
With dengue fever, residents of Southeast Asia and Africa who have suffered from this viral disease resort to eating pitaya fruits in order to increase platelets.
What foods increase platelets in the blood and their use is harmless to health?
- Chokeberry berries are consumed daily for 3 weeks in the amount of 50 pieces.
- A mixture of lemon and honey strengthens blood vessels and generally has a positive effect on hematopoiesis, as it contains a large amount of vitamin C (lemon), fructose, as an energy supplier.
- You can drink pomegranate juice every day, and in order not to harm the stomach, it is diluted with water in a ratio of 2:1.
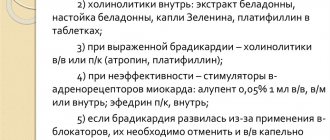
Medical drugs
The choice of drug and therapeutic regimen depend on the severity of the patient’s condition and his individual characteristics. Drugs that increase PLT in the blood:
- Corticosteroid hormones (Hydrocortisone, Dexamethasone and Prednisolone). Promote the release of blood platelets and slow down the process of their utilization in the spleen.
- Immunostimulants and immunomodulators (Methyluracil, Immunoglobulin, Derinat, etc.). Neutralizes toxins, replenishes missing IgG antibodies, increases the rate of cellular regeneration, and stimulates humoral immunity.
- Hemostatic agents. The group is represented by several types of drugs:
- Antifibrinolytics intended to inhibit the process of fibrinolysis - dissolution of blood clots and resorption of blood clots (Aprotinin, Tranexamic acid, Aminocaproic acid, etc.);
- Coagulants that can increase blood clotting (Vikasol, Menadione sodium bisulfite, Phytomenadione);
- Medicines that reduce vascular permeability (Etamzilat, Rutin).
- General strengthening elixir Sodecor (water-alcohol tincture, including ten medicinal plants).
Synthetic glucocorticoid drugs used in the complex therapy of thrombocytopenia
Most drugs are not prescribed to women during pregnancy due to their teratogenic effects on the fetus. Self-medication of thrombocytopenia is prohibited. The use of medications is allowed only as prescribed by a doctor. Vitamin and mineral supplements should be selected taking into account the presence of magnesium, calcium, zinc, folic acid (B9), cyanocobalamin (B12).
Additionally
Rehabilitation of hematopoietic processes is often carried out after chemotherapy, since the aggressive nature of the treatment negatively affects the composition of the blood. To restore platelet balance, the following are used:
- medications that activate the production of flat blood cells;
- course therapy with recombinant thrombopoietin, a liver hormone that regulates platelet synthesis;
- vitamin B9 (folic acid), which has a regenerating effect on bone and other tissues of the body.
Dietary nutrition is mandatory. The use of traditional medicine is allowed if there are no individual allergies and contraindications from the underlying disease (for the treatment of which a chemotherapy method was used).
Treatment of thrombocytopenia
The choice of treatment tactics for thrombocytopenia depends on its origin, type and severity. Conservative methods are used - hormonal therapy, treatment with immunostimulants, plasmapheresis to cleanse the blood of antibodies and their decomposition products.
In case of autoimmune processes of platelet destruction, drugs that suppress the immune system are prescribed. Treatment of thrombocytopenia with folk remedies is used as an additional component. If therapy does not produce results within 4–6 months, surgery is performed to remove the spleen.
Symptoms of thrombocytopenia
Thrombocytopenia increases the risk of life-threatening symptoms for the patient. Symptoms are more pronounced if the level of platelets is reduced, more than three times the standard. The norm is 180-320 x 109/l for men and women. A sudden and noticeable decrease in components in the blood is characterized by the indicator:
- gum bleeding for a long time;
- blood oozes systematically and intensely from the nose;
- increase in the duration of menstruation in women;
- increased size of the spleen;
- sudden formation of bruises;
- the appearance of petechiae - small red dots on the epidermis;
- there are feces with bloody manifestations, urine with blood clots;
- pain in the muscular and joint systems;
- cough and vomiting with blood;
- secretion of blood in hemorrhoidal areas;
- bleeding in the stomach and intestines.
The patient is not always notified of the development of thrombocytopenia while taking potent drugs. At the initial stage, the problem does not show symptoms. Due to the chemotherapy procedure, platelets and white blood cells drop, increasing the likelihood of developing diseases. Complications lead to a poor prognosis. The outcome in such cases is often fatal. Knowledge of methods for increasing hemoglobin in the blood if platelet volumes have fallen will help the patient prevent an unpleasant list of consequences.
Diet for thrombocytopenia
The diet of a patient with ITP should be complete. Foods that can cause allergies in the patient should be avoided. For an additional effect on blood clotting, you can take medicinal plant herbs, for example, drink their decoction instead of tea. Hemostatic collection: chamomile flowers 20 g, peppermint leaves 40 g, shepherd's purse herb 40 g. Pour 1 tablespoon of the collection into 1 glass of boiled water, heat in a water bath for 15 minutes, cool for 45 minutes, strain, drink ½ at a time glasses 2 times a day. It is also useful for ITP to eat viburnum fruits, infusion of nettle leaves, and water pepper extract. These herbal preparations reduce capillary permeability and improve blood clotting. They are an additional means of preventing bleeding in thrombocytopenia.
Blood counts after chemotherapy
During chemotherapy treatment, the patient is constantly prescribed blood tests to monitor the slightest changes in the composition of the blood. Usually, under the influence of toxins, the blood formula changes significantly.
- Leukocytes. The level of leukocytes during chemotherapy treatment is greatly reduced, which can be very dangerous for the patient, because his immune status drops sharply. As a result, the patient becomes defenseless even against the simplest microorganisms and infectious agents. Therefore, increasing white blood cells after chemotherapy is an important and necessary task.
- Hemoglobin. Chemotherapy has a depressing effect on hematopoietic functions (hematopoiesis). The patient experiences a sharp drop in hemoglobin to critical levels and develops severe anemia. Hemoglobin drops especially after a combination of radiation and chemotherapy or when undergoing a repeated course of chemotherapy. Normalizing the hemoglobin level significantly increases the patient’s chances of a speedy recovery, because the survival rate of cancer patients directly depends on hemoglobin.
- Red blood cells. Since toxins during chemotherapy inhibit hematopoietic processes, the content of red blood cells in the blood of a cancer patient also decreases. He develops pronounced erythrocytopenia, which is accompanied by a sharp loss of strength and rapid fatigue.
- Platelets. Platelet counts also decrease, and acute thrombocytopenia develops. This condition is critically dangerous for the patient, since the patient’s blood clotting ability is practically zero and the slightest wound can cause severe bleeding with large blood losses. Bruises appear on the patient's skin, bleeding occurs from the gums and nose, as well as bleeding in the digestive tract.
As you can see, the blood picture becomes very dangerous for the health of a cancer patient, so it is necessary to take urgent measures to restore the blood after a chemotherapy course of treatment.
Treatment of thrombocytopenia
Therapy for thrombocytopenic purpura includes treatment with glucocorticosteroid hormones, removal of the spleen, the use of immunosuppressants, immunoglobulin, danazol, α2-interferon. Plasmapheresis and platelet transfusion are performed. When bleeding develops, symptomatic treatment is used.
Treatment with glucocorticosteroid hormones
The use of glucocorticosteroids is one of the main methods of treating idiopathic thrombocytopenic purpura (hereinafter ITP). These hormones disrupt the interaction of platelets and antibodies to them, as a result, their destruction is reduced. In addition, these drugs reduce the rate of destruction of platelets in the spleen, which leads to an increase in their number in the blood. Treatment with glucocorticoids begins immediately after diagnosis. Typically, prednisolone or methylprednisolone is used in a daily dose of 1–1.5 mg/kg of the patient’s body weight. This dosage is usually observed for 2 weeks. After the blood platelet count increases to a certain level, the dose is gradually reduced. The duration of the course of glucocorticosteroid therapy is 4–6 weeks (sometimes up to 4 months). In severe forms of ITP, so-called pulse therapy is performed, when the drug is administered intravenously in large doses for 3 days, and then switched to maintenance treatment. The effectiveness of such treatment can be judged by the results of the first course. If it was effective, then in future relapses one can expect the same positive effect. If glucocorticosteroids do not help during the first course, their further use is unpromising.
Splenectomy
Surgical removal of the spleen, or splenectomy, is indicated in the following situations:
- Ineffectiveness of glucocorticosteroid therapy. This operation is recommended if the disease lasts more than 1 year and there are 2-3 exacerbations after the first course of hormonal therapy.
- Contraindications to glucocorticosteroid therapy or serious side effects from its use.
- Relapses of thrombocytopenia after hormone withdrawal.
- Severe thrombocytopenia with severe hemorrhagic syndrome, with hemorrhages in the face, tongue, sclera; hemorrhages in the brain, retina.
When the spleen is removed, platelet destruction decreases and their life expectancy increases. After surgery, platelet levels rise quickly, so it can be life-saving for patients with life-threatening bleeding. Splenectomy is indicated for exacerbation of the disease during pregnancy, if there is severe hemorrhage.
Treatment with non-hormonal immunosuppressants
This treatment is carried out when hormonal therapy and splenectomy are ineffective. With this therapy, the production of antibodies against one’s own platelets is inhibited, which leads to a decrease in their destruction and an increase in life expectancy. Such drugs as Vincristine, Cyclophosphamide, Azathioprine are used for several weeks. Treatment with cytostatic drugs is carried out with regular monitoring of blood tests. Many patients with ITP, even with low platelet levels, do not have hemorrhagic phenomena. It is believed that in this case long-term immunosuppressive therapy is unjustified.
Treatment with danazol
Danazol suppresses the production of gonadotropic hormones by the pituitary gland. The mechanism of its action in ITP is unclear, but with long-term use there is a gradual increase in the platelet count in the blood. This method is more effective in patients over 45 years of age.
Treatment with immunoglobulin
This is one of the most effective methods of immunotherapy for autoimmune diseases. Immunoglobulin is obtained from blood serum; this preparation contains the entire spectrum of immunoglobulin G (antibodies to external antigens, autoantigens and autoantibodies). Intravenous immunoglobulin suppresses the synthesis of antibodies to one's own platelets (autoantibodies) and suppresses their activity. It normalizes the function of T-lymphocytes. Immunoglobulin preparations cause a rapid but short-term increase in the number of platelets in the blood. Their administration is especially indicated before surgery or in severe hemorrhagic syndrome.
Treatment with α2 interferon
It is known that α2 interferon not only has an antiviral effect, but also inhibits the synthesis of antibodies against one’s own platelets. For ITP, it is used in the form of subcutaneous injections in courses under the control of a blood test. Treatment with α2 interferon is advisable if there is no effect from glucocorticosteroids.
Plasmapheresis
With this method, antibodies to the patient’s own platelets are removed from the patient’s blood. Plasmapheresis is carried out in combination with glucocorticosteroid therapy, which increases its effectiveness. Usually 2–4 sessions are performed, the removed plasma is replaced with fresh frozen plasma.
Transfusion of platelet concentrate
Due to the fact that ITP is based on the formation of autoantibodies to platelets and their destruction, platelet transfusion is carried out only for health reasons (bleeding during operations, during childbirth). In this case, it is preferable to transfuse platelets received from close relatives. The lifespan of transfused platelets is very short because they are quickly destroyed by antiplatelet antibodies. Their repeated transfusion causes increased formation of these antibodies and increases thrombocytopenia.
Symptomatic treatment of hemorrhagic syndrome
When hemorrhages and bleeding develop, aminocaproic acid is used orally, intravenously and locally. Courses of treatment with Etamzilat are carried out. This drug increases the strength of the capillary wall, reduces its permeability, and increases the formation of blood clots at the site of injury. Vitamin K preparations (Vikasol) are ineffective and can lead to further deterioration of platelet function.
Free quota surgery: how to get it and what’s changing in 2020
Cancer treatment >> Chemotherapy for cancer >> One of the most dangerous consequences of chemotherapy is the development of thrombocytopenia, which manifests itself in a significant decrease in the number of platelets in the blood. A decrease in platelets in the blood below normal affects blood clotting, which leads to bleeding of varying degrees of intensity.
As a result, intoxication and pancytopenia increase, which worsens the patient’s prognosis for recovery. In this situation, chemotherapy treatment has to be reduced, up to complete cessation.
Bleeding, together with infectious complications, often causes deaths in cancer. The patient must inform the doctor about cases of “unreasonable” appearance of bruises on the skin, indicating capillary hemorrhages, bleeding from the nose or gums, and cases of blood appearing in the urine and feces. During chemotherapy, the attending physician must monitor coagulogram parameters and platelet levels in the blood in order to prescribe adequate treatment in a timely manner.
Experts recommend that patients receiving chemotherapy:
- avoid using aspirin and other medications that contain acetylsalicylic acid, - do not use an electric razor, - blow your nose with extreme caution, - after injections, use pressure bandages until the bleeding stops, - it is advisable for women to use medications that inhibit the onset of menstruation, - surround yourself in everyday life with soft objects that are not capable of causing bruises, cuts, etc., - be extremely careful when working with sharp objects (for example, scissors). An increase in the level of platelets in the blood after chemotherapy is facilitated by:
An increase in the level of platelets in the blood after chemotherapy is facilitated by:
- platelet transfusion (recommended for platelet levels less than 20*10⁹, when the likelihood of bleeding is very high).
- administration of recombinant rhombopoietin immediately after chemotherapy for 10 days leads to an increase in platelets by 5-10 times. The effect lasts for 2 weeks after discontinuation of the drug.
Some medications help raise platelets after chemotherapy, for example, derinat, made from salmon nucleic acids, or codecor, which contains various herbs. Etamzilate helps strengthen the walls of blood vessels and increase the ability of blood to clot. Some hormonal drugs, such as dexamethasone, prednisolone, etc., also have similar properties. Drugs such as immunoglobulin, folic acid and panavir help fight thrombocytopenia.
In case of thrombocytopenia, all spicy, spicy foods and alcoholic drinks should be excluded from the diet. The daily menu should include foods rich in ascorbic acid and vitamin A (before using them, you should consult an oncologist), for example, bell pepper, rose hips, parsley, celery, carrots, green apples, buckwheat, liver, fish oil, etc. Foods such as almonds, pine nuts, peanuts, grape leaves and lingonberries improve blood clotting. An old folk remedy – nettle juice – has a beneficial effect on improving blood composition.
Thrombocytopenia
This is a painful condition during which the level of platelets in the blood falls below normal (less than 150,000 per 1 milliliter of blood). Due to this decrease, bleeding increases and there may be serious problems stopping bleeding.
Causes and forms of thrombocytopenia
Thrombocytopenia can be congenital or acquired. The most common form of the disease is the acquired form.
The acquired form of the disease comes in different types, which are distinguished depending on the causes of occurrence. Thus, thrombocytopenia can be:
- immune (the most common type, in which antibodies pass from a pregnant woman to her fetus);
- formed when cells located in the bone marrow are inhibited;
- consumption thrombocytopenia, which occurs in the presence of thrombosis and due to extensive hemorrhages;
- thrombocytopenia resulting from the transformation of bone marrow into a tumor;
- a decrease in the level of blood clots, which occurs due to mechanical damage to platelets that occurs with hemangioma.
The hereditary form includes diseases with abnormal damage (defects) to platelet membranes, which cause disturbances in their functioning.
The main factors contributing to the development of thrombocytopenia are: allergies to drugs (allergic or drug thrombocytopenia), infections and intoxications of the body provoke the development of symptomatic thrombocytopenia (causes of development include HIV, herpes, hepatitis, infectious mononucleosis, influenza, acute respiratory infections, rubella, chickenpox , systemic lupus). Additionally, Gaucher disease can cause low platelet levels.
There is also an idiopathic type of this disease. In this case, the cause of thrombocytopenia cannot be identified.
Symptoms of thrombocytopenia
The main signs of this problem are bleeding gums, constant and heavy bleeding from the nose, the appearance of bruises on the body and limbs for no apparent reason, difficult to stop bleeding after tooth extraction or with minor damage to the skin, blood streaks in the discharge, when urinating or defecation, heavy bleeding in women during menstruation, rash on the body and legs (the rash appears in the form of small red dots).
Also, hemorrhages may appear on the face and lips. This may indicate a cerebral hemorrhage.
For thrombocytopenia, no specific diets have been developed. You need to eat right, that is, the body must receive the right amount of proteins, carbohydrates, fats and all macro- and microelements, vitamins. For anemia, it is useful to eat foods containing iron (buckwheat, nuts, corn, beef liver, barley porridge, oatmeal, peas, dogwood, sprouted wheat).
It is useful to drink freshly squeezed juice from raspberries, strawberries, wild strawberries, apples, beets, cabbage leaves and black radish.
If you suffer from bleeding gums, then you need to eat currants, drink teas from the branches and leaves of currants and blackberries.
Traditional medicine for thrombocytopenia:
- To improve the condition of the blood with increased bleeding, you should drink decoctions of nettle, yarrow, rowan fruits (especially chokeberry), chicory, rue, rose hips, strawberries, medicinal verbena, water pepper.
- Sesame oil has excellent properties of regulating the number of platelets and increasing blood clotting.
For treatment, you just need to add 10 milliliters of this oil to your food several times a day. - To increase hemoglobin levels, you need to eat three walnuts a day with a teaspoon of honey.
- For the purposes of prevention and safety, you need to avoid dangerous sports and outdoor activities.
Children should only be allowed outside under adult supervision and must wear knee pads, elbow pads and a helmet. Such a child should be told about the characteristics of his body.
- fatty, salty, spicy foods;
- products with all kinds of dyes, additives, impurities;
- smoked meats, sauces, seasonings;
- fast food restaurant dishes;
- semi-finished products;
- pickled vegetables and fruits;
- brine and all dishes containing vinegar;
- alcohol;
- all products that can cause allergies.
Also, vegetarianism is strictly prohibited. You should also stop taking blood thinning medications. These include “aspirin”, “ibuprofen”, “noshpa”, “voltaren”, “acetylsalicylic acid”. This entire list disrupts the functioning of platelets.
Editor of the section “Nutrition for Diseases” Natalya Stefan, Food+
How to diagnose thrombocytopenia
A person may not suspect the presence of thrombocytopenia for a long time, since at first it is not accompanied by any specific symptoms.
As the pathology develops, the first symptoms appear:
- bleeding time from wounds increases;
- bleeding of the nose, gums, etc. is observed;
- in women – the duration and abundance of menstrual flow increases;
- hematomas and hemorrhagic rashes appear on the skin.
Having noticed a problem repeating itself over and over again, a person goes to the doctor. Most patients presenting with such complaints are referred for a general blood test. The laboratory conducts research on several indicators, including determining the number of platelets.
Doctors are not interested in the total volume of blood cells, but in their number compared to white blood cells, red blood cells and other blood components.
Attention!
If platelet levels are low, medical manipulations are dangerous because they damage the integrity of the skin and mucous membranes.
Blood for analysis is taken from a finger or a vein - it depends on the equipment of the laboratory. If questions arise, the doctor additionally prescribes a biochemical blood test. The study allows us to identify inflammatory processes, disorders in the endocrine system and water-salt balance, and other indicators.
The diagnosis of thrombocytopenia is made after a blood test for the content of proteins, carbohydrates, enzymes, pigments, and microelements. The nitrogen metabolism rate is also determined.
Blood clotting (platelet aggregation) is determined using special tests:
- According to Sukharev. For analysis, biomaterial is taken - blood from a finger, on an empty stomach. The material is placed in a special test tube, which is tilted in different directions. A stopwatch is used to measure the time until the blood loses its ability to move freely in the vessel.
- According to Lee-White. During the study, the rate of venous blood clotting is determined. Analysis - 3 ml of blood, taken on an empty stomach. Normal clotting time is considered to be 4-7 minutes (at 37°C). Blood taken for analysis is poured into three tubes heated to 37°C. They are installed with the floor tilted at an angle of 50 degrees. And then they record the time on a stopwatch and determine how many minutes it will take for the blood to clot completely. Complete clotting occurs when blood does not flow out when the tube is tilted.
Both analyzes are accurate and informative. Their implementation allows us to obtain additional information about the patient’s condition. Both methods are carried out in a hospital, since testing is carried out immediately after blood collection - due to its rapid clotting.
Nutrition for thrombocytopenia. Symptoms of low platelet levels
A condition in which the level of platelets in the body decreases is called thrombocytopenia. It is provoked by bad habits and poor nutrition. The pathology is dangerous because it disrupts all parts of homeostasis, which is accompanied by excessive bleeding.
The deviation is regulated with the help of medications and a special diet. The second method is more preferable, since medications have a systemic effect on the entire body.
The most pronounced symptoms of thrombocytopenia include:
- bleeding gums;
- heavy menstruation;
- slow regeneration of the skin;
- causeless appearance of bruises;
- nosebleeds.
Attention! Alcoholic drinks increase the risk of thrombocytopenia
Norms
To ensure control over hemostasis, standards are provided. The number of platelets in the blood is determined by laboratory tests. The norm for men is 200-400 thousand units/µl, and for women – from 180 to 320 thousand units/µl. During menstruation, the volume of blood cells decreases.
Causes
A sudden decrease in platelets in the blood is a serious reason for a comprehensive examination. Cells can be destroyed by the body’s own or simply not produced in the required quantity. In some cases, a decrease in the indicator indicates a malfunction of the spleen. Possible causes of the pathological process include the following:
- vitamin B12 deficiency;
- heavy metal poisoning;
- infectious diseases (chickenpox, HIV, hepatitis C, etc.);
- autoimmune diseases;
- toxic poisoning;
- blood cancer;
- Werlhof's disease;
- taking medications that affect blood clotting.
Enhancement Methods
To increase the platelet count, the doctor, if necessary, prescribes medications. If there is a slight decrease in the indicator, then a vitamin-mineral complex or special dietary nutrition will be sufficient.
Medications
Traditional treatment, which involves taking certain groups of medications, is used in case of critical deviation from the norm. Among the most common and frequently used means by which platelets can be raised are the following:
- Etamzilat. Available in the form of a solution intended for intravenous administration. The drug has a stimulating effect, which helps to increase the production of platelet cells by the bone marrow. The effectiveness will be noticeable 5-15 minutes after the solution is administered.
- Prednisolone is a steroid hormone that is sold in tablet form. An increase in platelets is observed within seven days.
- Immunoglobulin. The composition includes substances that help stimulate the immune system. After completing the course of treatment, the level of the cells in question increases to 75 percent compared to the initial levels.
- Vikasol. Prescribed to prevent the development of internal bleeding.
- Sodecor is a herbal preparation that normalizes the process of hematopoiesis.
All medications should be taken only as prescribed by a doctor. You should not self-medicate with medications, since the result of incorrect actions can provoke dangerous complications.
Traditional medicine
To quickly increase platelets in the blood, you can use folk remedies.
For treatment at home, the following drugs will be most effective:
- Nettle decoction. It is considered one of the best for stopping bleeding. In addition, the plant helps cleanse the blood and normalize its composition. To get the most positive result, you need to drink 200 milliliters of decoction daily.
- Lemon and honey. Good for strengthening blood vessels. For administration, the components are mixed in equal proportions. To enhance the healing effect, it is recommended to add flaxseed or sesame oil to the composition.
- Oak bark. To prepare a medicinal infusion, you need to pour a tablespoon of raw material with 200 milliliters of boiled water and let it brew. The decoction is used as a rinse, which is effective for bleeding gums, which also indicates a decrease in platelet cells in the blood.
- Pomegranate juice. For effective treatment, it is recommended to use only natural products. Before use, it is usually diluted with water in a 2:1 ratio. If you have stomach problems, it is better not to drink juice on an empty stomach.
- Chokeberry. Helps increase blood viscosity. To increase platelet levels, you need to eat about 50 berries per day for 20 days.
Despite the effectiveness of natural ingredients, treatment with traditional medicine should only be carried out with the permission of the attending physician.
It is important to take into account contraindications, the general condition of the body, concomitant pathologies, etc.
Special food
A properly formulated diet also plays an equally important role in increasing the number of these cells. It must include foods rich in iron:
- pumpkin seeds;
- soy;
- spinach;
- carrot;
- buckwheat;
- liver;
- Brewer's yeast;
- strawberry;
- potato;
- beet;
- bananas and other foods that increase the number of platelet cells.
For the purpose of treatment and prevention of low indicators, the following must be excluded from use:
- ginger;
- citrus;
- blueberries and raspberries
- alcohol;
- olive oil;
- chocolate products.
The menu is designed so that it includes a maximum of healthy products, which contain all the important vitamins and microelements. There should be no dishes that thin the blood.
Products that reduce their level
If the goal is to increase platelets in the blood, then it is strongly recommended to avoid or minimize their consumption of the following foods:
- Dairy products. Cottage cheese is especially “dangerous”, as are some varieties of cheeses based on goat’s milk. Their main feature is their high calcium content, which tends to reduce the bioavailability of iron. If it is impossible to give up dairy products, then it is better to give preference to low-fat kefir, yogurt, and sweet desserts.
- Ginseng. Increases red blood cells, but inhibits platelet production. Moreover, in men the platelet concentration decreases faster than in women, which is explained by some physiological characteristics of their bodies.
- Red wine. It acts similarly to ginseng - it increases the rate of red blood cells in the blood, but reduces platelets. Concentrated grape juice is less effective in this regard. That is, it should also be abandoned.
- Coffee. Although it increases blood pressure, it slightly reduces the platelet rate. That is why, in case of diseases of the cardiovascular system, coffee (and tea, since it also contains caffeine) must be avoided.
Platelets as blood cells
Nuclear-free blood plates are formed in the bone marrow from the semi-liquid content of its giant cells (megakaryocytes). The process of thrombocytopoiesis (formation of blood platelets) is regulated by the hormone thrombopoietin, synthesized in the liver, spleen and kidneys.
Approximately one third of all platelets produced are contained in the spleen, the rest circulate throughout the body in the bloodstream. The lifespan of flat cells is ten days, after which they are utilized (digested) by tissue phagocytes of the spleen.
Functional responsibilities of platelets include:
- Providing primary hemostasis (vascular-platelet response to blood loss). When microtrauma of capillaries or rupture of large vessels occurs, a significant number of platelets quickly move to the site of damage. Due to aggregation (the organic ability of flat cells to stick together), a blood clot is formed, stopping bleeding.
- Maintaining the integrity and trophism of the endothelium (the inner layer of the vascular wall). For the endothelium, platelets are both suppliers of nutrients and objects of nutrition (1/15 of the total cell volume is absorbed by the inner layer of the vascular wall).
Important! The main responsibility of platelets is to protect blood vessels from damage and ensure the process of normal coagulation (blood clotting). Normal platelet count in a general clinical analysis (CCA) of blood
| For women | For men | For children |
| 180–320 (*109 cells/l) | 200–400 (*109 cells/l) | 180–380 (*109 cells/l) |
The general blood test takes into account the platelet count (PCT) - the percentage of platelet mass to the total blood volume. Reference thrombocrit values for adults and children range from 0.22 to 0.24%. PLT and PCT are closely correlated, their indicators in the OKA increase and decrease in proportion to each other.
A feature of platelet parameters is their variability under the influence of physiological factors and climate:
- In women, in the first week of the follicular phase of the menstrual cycle, the level of PLT and PCT can decrease by half, which is associated with blood loss. Thrombocytopenia during the perinatal period is due to the natural protection of the expectant mother’s body from the risk of thrombosis. The normal platelet count for a pregnant woman ranges from 100–310 (*109 cells/l).
- PLT and PCT indicators decrease slightly at night and in the spring season. This is not an anomaly, since the body does not show physical activity at night, and in the spring it often experiences a state of vitamin deficiency.
- A reduced platelet count is a clinical sign of underweight in newborns.
Deviation of PLT values from the norm is not a basis for diagnosing a specific pathology. The doctor must evaluate the comparative characteristics of all indicators of OKA and refer the patient for an extensive examination (analysis of venous blood for platelet indices and biochemical composition, ultrasound, MRI, CT).
Complex therapy, including:
- medications and vitamin-mineral complexes;
- nutrition correction;
- traditional medicine.
Treatment of thrombocytopenia is prescribed in accordance with the diagnosed cause of deviation from the norm. To restore normal values of platelet parameters, it is strongly recommended to stop drinking alcoholic beverages and maintain a drinking regime (at least 2 liters of water per day). A patient diagnosed with thrombocytopenia needs to adhere to a rational work and rest regimen. The body should not be physically overloaded.
Traditional medicine against thrombocytopenia
Treatment with folk remedies is aimed at strengthening the vascular walls, increasing the platelet mass in the blood and, as a result, reducing bleeding. One of the important components of home treatment is diet therapy.
Proper nutrition
There is no special diet developed for patients with thrombocytopenia. In dietetics they are shown a common table. And yet, doctors talk about the need to change eating habits. The diet should contain a sufficient amount of animal and plant proteins. Therefore, a vegetarian diet is excluded for thrombocytopenia.
Severe degrees of the disease cause stomach bleeding. This must be kept in mind when choosing the type of processing and method of cooking. It should be crushed so as not to injure the mucous membranes of the gastrointestinal tract. Hot, cold, spicy, smoked and fatty foods are contraindicated. You will have to give up blood thinners and include foods rich in vitamin B12 and folic acid in your menu. Meals should be fractional. What you can and cannot eat if you have thrombocytopenia.
| Authorized Products | Prohibited foods (injuring the mucous membrane and lowering the platelet count) | Foods containing vitamin B12 | Foods containing folic acid |
| Liver | Hot spices, sauces and marinades | Green salads | Pulses |
| Cheeses | Semi-finished products | Spinach | Broccoli and Brussels sprouts |
| Egg yolk | Products containing dyes | Asparagus | Whole wheat bread |
| Buckwheat | Canned food | Baked goods made from rye or whole wheat flour | Avocado |
| Nuts | Pickled vegetables | Pumpkin | Carrot |
| Barley porridge | Vinegar | Avocado | Turnip |
| Oatmeal | Alcohol | Apricots | Lemon |
| Corn | Seafood | Beef by-products (heart, tongue, liver) | Pears and apples |
| Yeast | Fatty fish | Rabbit meat | Melon |
| Beet | Garlic | Low-fat dairy products | |
| Pomegranate | Coffee | ||
| Lean meat and fish | Cinnamon | ||
| Cucumbers, zucchini, radishes | |||
| Cherries, raisins and oranges | |||
| Mushrooms |
The diet for thrombocytopenia should be high in calories, and the food should be easily digestible. Freshly squeezed juices from berries (strawberries, wild strawberries, raspberries), vegetables (cabbage, beets, herbs, black radish), fruits (apples, bananas) are useful. Bleeding gums will be reduced by currants, blackberries and decoctions of their leaves. This diet will prevent anemia that develops with prolonged bleeding.
Medicinal herbs for thrombocytopenia
Popularly, medicinal herbs that raise platelet levels are called hemostatic. Together and separately, they help stop minor hemorrhages and reduce the external manifestations of thrombocytopenia.
The most common and effective recipes:
- Nettle juice and milk, mixed in a 1:1 ratio. For 7 days, take three servings of the medicine (1 serving - 100 ml). Then they take a week break and repeat the course.
- Add sesame seed oil to your morning salad or simply drink a tablespoon of the product in the morning on an empty stomach.
- Beetroot juice. The vegetable is grated, infused with sugar for 8 hours, then squeezed through cheesecloth. You should drink it for 14 days in the morning shortly before breakfast. After a month's break, the course is repeated.
- Hemostatic mixture of peppermint and shepherd's purse (40 g of dry raw materials) and chamomile (20 g). The mixture is infused in a water bath and taken a glass twice a day.
- A collection of verbena, nettle, rose hips, strawberries and yarrow in the amount of 3 tablespoons is poured with boiling water (0.5 l) and infused for half an hour. This amount of infusion is enough for 7 days. It can be taken for several months.
In addition to the herbs listed, you can brew and drink tea from saffron, blueberries, white mistletoe, knotweed, and walnuts every day. Any herbal treatment must be agreed upon with the attending physician.
Lifestyle changes
In acute thrombocytopenia, the patient is prescribed bed rest. As soon as the platelet count approaches the lower limit of normal, the patient is recommended to do light exercises and moderate physical activity, long walks, if possible, not in the open sun.
With thrombocytopenia, a full night's sleep of at least 8 hours and a daytime sleep of 1–2 hours is necessary. The cause of platelet destruction may be a viral infection, so contact with people suffering from viral or infectious diseases is excluded.
RESPONSIBILITY
the registry ÑгогогоÑмонР° â коÑÑизона. RESULTS е, еÑли Ñ Ð¿Ð°Ñ¸ÐµÐ½Ñа ÑÑомбоÑиÑопенР¸Ñ поÑле ÑимиоÑеÑапии.
RESULTS registry ½Ð¾ÑÑÑ › а ÑÑомбоÑиÑов. RESULTS ROOM °ÐµÑ дейÑÑвие иммÑниÑеÑа, коÑоÑÑй и Ñак пÑак ÑиÑеÑки оÑÑÑÑÑÑвÑÐµÑ Ñ ÑÐ°ÐºÐ¸Ñ Ð»Ñдей.
RESEARCH, RESEARCH, RESEARCH °ÑаллелÑно with the елÑно. RESULTS 4-6 RESULTS , ROCK 2 пµÑеÑÑва.
RESULTS AND RESPONSIBILITIES леÑении ÑÑомбоÑиÑоп ении. RESULTS RESULTS, RESULTS ¾Ð³Ð¾ мозга. RESULTS RESULTS, ASSESSMENTS ¸Ð»Ð»ÑÑов и Ð¼ÐµÐ»ÐºÐ¸Ñ ÑоÑÑдов.
RESPONSIBILITY AND RESPONSE RESULTS ÐºÑ Ð¼Ð¾Ð»Ð¾ÐºÐ¸ оÑеÑа. RESULTS, RESULTS ¾ÑÑÑанавливаÑÑее и ÑегенеÑаÑивное дейÑÑвР¸Ðµ, ноÑмалР¸Ð·ÑÐµÑ ÑиÑло ÑÑомбоÑиÑов в кÑови и дÑÑÐ³Ð¸Ñ ÐºÐ»Ð µÑок. RESULTS ASSURANCE. RESULTS, ROOM ASSURANCE.
ROOM ½ÐµÐºÐ¾ÑоÑÑм болÑнÑм Ñ ÑÑомбоÑиÑопенией. RESULTS.
ROOM µÐ½ÐºÐ¸) â Ñп¾Ñоб, к коÑоÑÐ¾Ð¼Ñ Ð¿Ñиб RESULTS, RESULTS µÐ½Ð½Ñе ÑпоÑÐ¾Ð±Ñ Ð½Ðµ даÑÑ ÑезÑлÑÑаÑа.
Thrombocytopenic purpura
The essence of the disease
Idiopathic thrombocytopenic purpura (ITP) is a disease characterized by a significant decrease in the level of platelets in the blood, which usually leads to hemorrhagic syndrome, that is, increased bleeding. The term “Werlhof's disease” is also used in honor of the doctor who first described the disease. It has also been proposed to use the term “primary immune thrombocytopenia”.
Antibodies to his own platelets are formed in the patient’s body, the rate of destruction of blood platelets increases several times, and a deficiency of these cells occurs. It is ITP that is the most common cause of hemorrhagic syndrome in patients observed by hematologists.
There are acute and chronic forms of ITP. Acute forms (which make up the majority of cases of the disease in children) last less than 6 months. Chronic forms differ in the frequency of relapses: from ITP with rare relapses to a continuously relapsing course.
Incidence and risk factors
The frequency of ITP is, according to various sources, from 5 to 20 cases per 100,000 people. The disease occurs in both adults and children of any age, but the frequency depends on age: young adults from 20 to 40 years old are most often affected, and children and the elderly are least likely to get sick. Girls and women suffer from ITP several times more often than boys and men. In young children, an acute form of the disease is more often observed, while in adolescents and adults, a chronic form is observed.
The causes and mechanism of development of the disease are still not fully understood. But it is known that the disease can be triggered by a previous viral infection: acute respiratory viral infection, rubella, measles, cytomegalovirus (CMV), Epstein-Barr virus (EBV), etc. In addition, possible provoking factors include pregnancy, taking a number of medications, stress, physical overload, excessive sun exposure, etc. ITP is not a hereditary disease.
Signs and symptoms
ITP is characterized by hemorrhagic syndrome, that is, signs of increased bleeding. As a rule, the disease occurs suddenly. Subcutaneous hemorrhages are observed: pinpoint (petechiae) and larger (ecchymosis), areas of hemorrhage can merge with each other. Bruises easily, especially on the arms and legs. Hemorrhages into the mucous membranes and bleeding from them may occur. Bleeding from the nose, gums, and uterine bleeding in girls are common. Intestinal bleeding and the presence of blood in the urine are less common. If platelet levels are very low, life-threatening complications such as cerebral hemorrhages are possible. Significant blood loss with the development of severe anemia is also dangerous.
On the other hand, if the decrease in platelet count is not too significant, the disease may not have any obvious symptoms and can be detected only by the results of a blood test, the appearance of isolated bruises, and in girls, also by longer and heavier menstruation.
Diagnostics
The first sign of ITP is a low level of blood platelets - thrombocytopenia. Other blood counts remain normal. Changes in the coagulogram are observed, such as an increase in bleeding time. However, for an accurate diagnosis, it is necessary to exclude other causes of decreased platelet levels: leukemia, myelodysplastic syndrome, aplastic anemia, systemic lupus erythematosus and other autoimmune diseases, etc. When examining the bone marrow, a normal or increased number of megakaryocytes (cells from which platelets are formed) is observed. ; this means that platelet deficiency is not due to insufficient production, but to their destruction in the blood. Tests often detect antibodies to platelets in significant quantities. An enlarged spleen is not typical for ITP.
When diagnosing, it may be useful to study the medical history, including previous viral infections, since, as mentioned above, they can provoke the development of ITP.
Treatment
Therapy for patients with ITP is based on an individual approach. The need for treatment is determined by the requirement to achieve and maintain a safe level of platelets - because with deep thrombocytopenia, life-threatening hemorrhages are possible. Specific therapy is also determined by factors such as the degree of bleeding (severity of hemorrhagic syndrome), concomitant diseases, etc.
For example, if the platelet level is not too low, there are no signs of hemorrhages on the skin or they are gradually decreasing, and there are no severe bleedings, then simply careful monitoring of the patient may be recommended.
In more severe cases, however, treatment is necessary. Glucocorticoid hormones (prednisolone, methylprednisolone, dexamethasone) are often used as the first line of therapy. But their long-term use is associated with unwanted side effects. Intravenous administration of immunoglobulins (Pentaglobin, Octagam, etc.) can also be used, which prevent increased destruction of blood platelets.
If the disease constantly recurs and does not respond to therapy, then patients may be advised to remove the spleen (splenectomy). This procedure is successful in most cases, but is associated with certain risks and leads to disruption of the body's immune defense. Therefore, they often try to avoid it, especially in children.
"Enplate" (romiplostim) is a drug that in the last 10-15 years has revolutionized the treatment of many patients with chronic and recurrent forms of ITP. “Enplate” stimulates increased platelet production, is highly effective, quickly achieves results, and is well tolerated. Another drug effective for the chronic form of the disease is Revolade (eltrombopag). Both drugs remain effective even with long-term use and can be used on an outpatient basis (“Enplate” is administered subcutaneously, “Revolade” is used in tablet form), but the high cost still limits their use.
Sometimes other medications are used, such as immunosuppressants (MabThera, Azathioprine, etc.). Angioprotective drugs can be used to improve the condition of blood vessels. There are other treatment options that can be individualized. Transfusions of donor platelets are not recommended, except in situations of life-threatening bleeding, since such transfusions enhance the formation of antibodies to platelets.
Patients with ITP must observe certain restrictions, especially during periods of exacerbation. They need to avoid any injuries (which severely limits their ability to play sports); taking aspirin and other drugs that reduce blood clotting; contact with allergens, excessive sun exposure, vaccinations, etc.
Results
Platelets are anucleated flat blood cells produced in the bone marrow. Their main functions are maintaining normal blood clotting and protecting blood vessels from rupture. If the platelet count rises, the blood becomes thicker, which can lead to blocked blood vessels, heart attack and stroke.
A reduced content of flat cells (thrombocytopenia) indicates anemia, oncohematological diseases, and chronic intoxication of the body.
You can raise platelets in a moderate stage of decline with the help of folk remedies and proper nutrition. In more serious cases, the doctor prescribes therapy with immunostimulating and hemostatic medications, hormone-containing medications and vitamins. It is prohibited to use medications without a doctor's permission.
Thrombocytopenia: diet and treatment
Thrombocytopenia is a disease accompanied by a decrease in the number of platelets in the blood - blood cells responsible for its clotting. These diseases can be caused by various reasons, be congenital or acquired. Common to all thrombocytopenia is the leading syndrome - bleeding. Bleeding with thrombocytopenia occurs spontaneously or after minimal damage and can last up to several days. Thrombocytopenia is also characterized by the appearance of small hemorrhages on the skin and mucous membranes - petechiae, and larger ones - ecchymosis (colloquially bruises).
The most common cause of thrombocytopenia is immune disorders. Children usually experience pathological immune reactions when the body comes into contact with external factors - viruses, bacteria, drugs. In adults, autoimmune variants predominate, when immune mechanisms are directed against the body's own cells. The most common form of thrombocytopenia is idiopathic thrombocytopenic purpura.