The physiology of the cerebral venous system is currently still poorly understood. Therefore, only experienced phlebologists and neuropathologists know what venous discirculation is and how to treat it. Although in fact, under such a complex term lies an ordinary violation of venous blood flow. In a healthy person at rest, the average speed of venous blood movement is approximately 220 mm/min, and in those suffering from dyscirculation it decreases to 47 mm/min. Knowledge of the anatomy of the circulatory system of the brain will help you independently determine the symptoms caused by dyscirculation, as well as take preventive measures in advance.
The mechanism of occurrence of venous discirculation
Cerebral veins can be divided into 2 subtypes: superficial and deep. The veins that are located in the soft membrane (superficial) are designed to drain blood from the cerebral cortex, and those that are located in the central parts of the hemispheres (deep veins) serve to drain blood from the white matter. The above vessels carry blood to the superior and inferior longitudinal sinuses. From these collectors, blood is pumped into the internal jugular vein, and then flows from the brain through the vertebral vein system.
This rather simplified description of the complex route of blood outflow allows us to understand why for such a long time doctors cannot determine the true causes of cerebrovascular accidents.
At the moment, doctors have learned that cerebral venous discirculation occurs due to pathological processes in the cavity between the membranes of the brain or in the cervical and spinal plexus. In 75% of cases, these pathological processes are cervical osteochondrosis or atherosclerotic plaques.
Introduction
Chronic cerebrovascular disease (CVD) is a fairly heterogeneous group of conditions that differ in developmental pathogenesis, clinical manifestations and course dynamics.
Among the main etiotropic factors in the development of CVD, arterial hypertension can be put in first place as the main factor that damages the vascular wall and leads to the development of the so-called small vessel disease - the pathomorphological basis for the development of CVD [1]. However, we should not forget that causes such as atherosclerotic artery disease, hyperlipidemia, diabetes mellitus, cardiac arrhythmia (primarily atrial fibrillation), and damage to the venous bed make a significant contribution to the pathophysiology of the formation of chronic CVD. It should be noted that all of the above factors primarily lead to vascular damage and, as mentioned above, small-caliber vessels, primarily capillaries, suffer the most. Meanwhile, cerebral capillaries, unlike peripheral ones, are a structural and functional part of the blood-brain barrier, the destruction of which creates the preconditions for the penetration of immunocompetent cells, plasma proteins, and red blood cells into the brain, which, along with ischemia and microhemorrhages, has a toxic effect on the brain, triggering extra- and intracellular signaling pathways leading to neurodegeneration and demyelination, and, accordingly, to atrophy and leukoaraiosis, detected in patients with CCVD during neuroimaging [2]. Most of the above pathogenetic factors are well studied and described, although it should be noted that, for example, the problem of microhemorrhages is not sufficiently covered in domestic publications, along with such an important pathogenetic link as venous discirculation (VD). There is no consensus in the literature which term most accurately characterizes the pathology of the cerebral venous bed. Concepts such as venous encephalopathy, venous discirculation, venous insufficiency, obstruction of cerebral venous outflow, etc. are used [3–7]. In addition, it is not always clear what size lesions of venous vessels are meant in certain publications. Another important issue is the participation of the cerebral venous system in the functioning of the glymphatic system of the brain (GLS), which was discovered by a group of researchers in 2012 and described by the authors as “a drainage system connecting the perivascular spaces with the CSF pathways” [8]. The peculiarities of the functioning of this system have not been sufficiently elucidated to date, however, it has been shown that DBS plays a critical role in the elimination of cerebral metabolic products, in particular beta-amyloid and tau oligomers [8, 9]. It has also been established that this system functions in the slow-wave sleep phase, i.e., the clearance of eliminated metabolites increases precisely in this sleep phase [10]. The close functional relationship between DBS and the venous system of the brain has also been clarified. According to JJ Iliff et al. [8], DBS functions as follows: at the first stage, cerebrospinal fluid (CSF) circulates from the basal cisterns into the subarachnoid space, washing the brain, after which it enters the periarterial space, then from the periarterial space of the CSF through channels formed by aquaporin-4 on astrocytic stalks , enters the intercellular space, where it mixes with the interstitial fluid and, accordingly, the products of brain metabolism, and finally, through the perivenular spaces it is directed to larger veins and further into the venous bed (Fig. 1).
Thus, it is obvious that healthy cerebral metabolism depends on the normal functioning of the DBS and venous system; it is not without reason that a number of authors consider disorders of the drainage system to be the leading cause, for example, of Alzheimer’s disease [12].
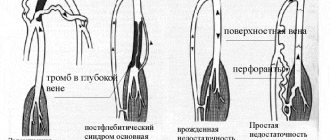
Approaches to determining VD between domestic and foreign authors differ. According to domestic researchers, chronic cerebral venous insufficiency is a pathological condition associated with impaired venous outflow from the brain, leading to decreased blood flow and intermittent return movement of blood from the intracranial jugular vein through the transverse sinus and other sinuses into the basal and deep veins [6, 13]. Currently, the following clinical forms of VD are distinguished: cephalgic, pseudotumorous, neurosis-like, microfocal (venous encephalopathy). There are 3 stages of VD: subclinical, functional disorders, encephalopathy. Domestic studies note that VD is more common in women. The nature of complaints and the clinical picture of the disease are very variable and largely depend on the severity of venous outflow disorders and the possibilities of compensation. The leading complaint of patients with VD is usually headache [3, 13]. The term “chronic cerebrospinal venous insufficiency” appears in foreign publications. However, this condition is not considered within the framework of cerebrovascular disease; the authors point to the role of venous insufficiency as a pathogenetic link in multiple sclerosis [3, 14].
Treatment of cerebral VD represents a significant medical problem, since approaches, including medications, have not yet been developed that would show their effectiveness in this group of patients from the standpoint of evidence-based medicine. Moreover, drugs with potential venotropic effects mostly have only an oral dosage form. To date, the only venotropic drug administered parenterally is an escin-containing drug obtained from the horse chestnut fruit - L-lysine escinate. It is a combination of the water-soluble saponin salt escin and the amino acid L-lysine. The drug improves the elasticity of veins, increases the tone of venous vessels, normalizes blood rheology, stimulates the antithrombotic activity of serum, improves microcirculation, dose-dependently reduces vascular-tissue permeability and the permeability of the plasma-lymphatic barrier, reduces the activity of lysosomal enzymes and prevents the occurrence of an exudative reaction to prostaglandins, has a moderate diuretic effect, has a beneficial effect on tissue trophism. In addition to the main pharmacological action, the drug has an anti-inflammatory effect and has a pronounced analgesic effect, especially for pain of traumatic origin. The drug also provides an immunocorrective effect, eliminates stress hyperglycemia in patients with brain damage and normalizes the level of blood carbohydrates, thereby preventing the development or eliminating the phenomena of acidosis of brain tissue and preventing further cerebral damage [15, 16].
Considering the above-described features of the pharmacodynamics of L-lysine aescinate, it seems advisable to use it in VD.
The purpose of the study
was to evaluate the effectiveness of L-lysine aescinate in the treatment of cephalgic, ataxic and asthenic syndromes in patients with chronic cerebral ischemia caused primarily by venous disorders.
Causes of obstruction of blood flow from the brain
It is quite difficult to determine exactly what exactly provoked the disruption of the normal outflow of blood from the brain, because more than one year may pass after the event that provoked the blockage. The main causes of venous discirculation may be:
- pulmonary and heart failure;
- compression of extracranial veins;
- jugular vein thrombosis;
- brain tumors;
- traumatic brain injury;
- cerebral edema;
- systemic diseases (lupus erythematosus, Wegener's granulomatosis, Behcet's syndrome).
Discirculation can be provoked by either one disease or a complex of several unpleasant symptoms. For example, a mutation in the prothrombin protein in combination with the use of contraceptives in the form of pills increases the risk of developing dysgemia (another name for venous discirculation).
Risk factors
In addition to the above diseases, disruption of venous blood flow can provoke an unhealthy lifestyle. If you find yourself with at least one of the risk factors listed below, you need to make an appointment with a neurologist to discuss measures to prevent dysgemia.
High blood pressure and a sedentary lifestyle are the first step to dysgemia
The following deviations should alert you:
- presence of diabetes mellitus;
- high blood pressure;
- obesity degree 2 or higher;
- high cholesterol;
- high triglyceride levels;
- passive lifestyle.
Thrombolysis
Dissolution of venous blood clots with special drugs - thrombolytics. These include streptokinase, urokinase and actilise. Only direct administration of a thrombolytic through a catheter into a thrombus with regular monitoring of the patency of the affected segment is effective. Thrombolysis options may include the use of a special Angiojet device. The thrombolytic solution is supplied through a special probe under high pressure, and then the blood clots are sucked out by a special suction. Another similar device used in our clinic is the Aspirex probe. This is a special spiral suction that gently removes thrombotic masses. The use of Aspirex in the inferior vena cava is limited due to its large diameter, so catheter thrombolysis is the most acceptable method. Thrombolysis is possible only in the first 10 days from the onset of the disease, while the blood clots have not yet healed.
Symptoms of pathology
Dysgemia is almost always accompanied by periodic dull headaches, sometimes with nausea and vomiting. Less commonly, a disturbance of consciousness occurs, after which focal symptoms appear:
- numbness of the limbs;
- severe aphasia;
- isolated epileptic seizures;
- impaired vascular-platelet hemostasis.
Signs of venous discirculation may appear irregularly and last for several minutes. If the disease is not treated, then unpleasant symptoms can constantly bother the patient.
Only a doctor can help prevent the development of severe dysgemia
The most serious symptoms that occur if the disorder is ignored are:
- dizziness;
- blurred vision;
- sudden loss of consciousness;
- tingling in the neck, especially on the left;
- moderate hypoxia;
- sudden reflex movements;
- constant drowsiness.
What does ignoring the problem lead to?
Ignoring symptoms for a long time results in oxygen and glucose not reaching the brain. This can lead to neurological problems. Lack of treatment can provoke more severe conditions.
Stroke
If any tumor blocks the flow of blood in the carotid artery, a heart attack or stroke may occur. As a result, some brain tissue may die. The death of even a small amount of tissue can affect speech, coordination, and memory. The severity of the consequences of a stroke depends on how much tissue has died and how quickly the outflow of venous blood has been restored. Some patients are able to fully recover, but most of those affected suffer irreversible changes.
Brain hemorrhage
With chronic problems with cerebral venous circulation, bleeding in the cranial cavity may occur. This occurs when the walls of the arteries weaken and burst. Even minor bleeding puts pressure on the brain, which can lead to loss of consciousness.
Hypoxia
Hypoxia occurs when completely or partially blocked venous drainage prevents oxygen from reaching the brain. Individuals with hypoxia often feel lethargic and dizzy. If the vessels are not promptly unblocked, coma and death may occur.
Dyscirculatory encephalopathy (including atherosclerotic origin)
Discirculatory hypertensive encephalopathy is a painful syndrome that is caused by a violation of venous blood flow. With minor dyscirculation, encephalopathy develops very slowly and is practically asymptomatic. The syndrome quickly disappears when the original causes of dysgemia are eliminated. But with a prolonged lack of oxygen or as a result of a complete blockage of venous outflow, brain death can occur (just 6 minutes after the complete cessation of blood flow).
How does CVI manifest?
The disease often develops unnoticed. The first signs of venous insufficiency may be heaviness in the legs, swelling that appears in the evening, and cramps. Spider veins may form. The further course of the disease may be accompanied by dryness and darkening of the skin, and the formation of characteristic spots. While walking, pain and characteristic squeezing are felt in the legs; with prolonged immobility, discomfort is also felt.
Lack of timely treatment for CVI can lead to the development of thrombosis, which can be life-threatening, or a trophic ulcer.
The classification of the disease includes several stages, from a small cosmetic defect and swelling of the lower leg, to noticeable skin changes and the appearance of an ulcer. Seeing a doctor in the early stages of the disease will help restore the health of your legs, avoiding surgical intervention.
Diagnostic methods
If the patient complains of several of the above symptoms, then all the doctor’s efforts will be aimed at identifying and treating the cause of the dyscirculation. This involves a physical examination and a medical history. To confirm the violation of venous outflow, several studies are prescribed with visualization of veins in the brain and vertebrobasilar region.
Complete blood count
It is prescribed to detect antinuclear antibodies and determine the erythrocyte sedimentation rate. If the results of the analysis confirm the presence of antibodies and a reduced ESR, then an additional study is prescribed to determine complement components and the level of antibodies to anti-deoxyribonucleic acid. The results of the above tests will reveal that the cause of dysgemia is systemic lupus erythematosus or Wegener's granulomatosis.
Electroencephalogram (EEG)
An electroencephalogram with impaired outflow of venous blood may be normal. But this study is strongly recommended after unilateral thalamic infarction. A slowdown in the basic alpha rhythm indirectly indicates coordination abnormalities and problems with blood outflow.
An EEG can help a doctor identify venous dyscirculation
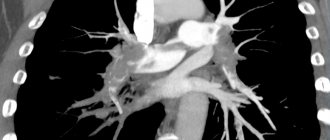
Computed tomography (CT)
CT is an important imaging modality and is often indicated for the initial diagnosis of dysgemia. In the tomograph image, you can see whether any neoplasm or thrombosis is the cause of dyshemia.
CT angiography
CT angiography is also prescribed to visualize the cerebral venous system. Only angiography can indicate the absence of flow in the venous channels.
Contrast magnetic resonance imaging
Contrast magnetic resonance imaging is an excellent method for visualizing blood flow in the great cerebral veins. It is prescribed if angiography does not reveal any disturbances in the outflow of venous blood into the VBB.
Prevention
To prevent circulatory problems in the brain:
- Get rid of bad habits.
- Avoid stress, overexertion, and overtime.
- Eat right.
- Do not subject your body to excessive physical activity, but also do not lead a sedentary lifestyle.
- Treat chronic diseases in a timely manner, especially for cervical osteochondrosis, which people often do not give due importance. If your neck hurts, immediately go to a neurologist.
- Monitor your blood pressure, especially if you are over 40. Buy an automatic electronic blood pressure monitor and measure your blood pressure 2 times a day. This will take at most 5 minutes a day, but in this way you will eliminate hypertension and hypotension. If you notice that your blood pressure changes, immediately go to a therapist, and then to a cardiologist.
- Once every six months to a year, undergo a preventive examination with a therapist, cardiologist, or neurologist.
How to treat venous discirculation?
The doctor may recommend several different treatment methods, depending on the identified causes of the disease. But most patients will be advised to make changes to their daily lifestyle, namely:
- stop smoking and drinking alcohol;
- perform simple physical exercises daily;
- follow a diet to lower cholesterol levels;
- Monitor your blood sugar and blood pressure daily.
As for the drug treatment of patients with venous discirculation, specific therapy is prescribed, which includes taking anticoagulants or thrombolytics (depending on the medical history). But the use of systemic anticoagulation as primary treatment is recommended for all patients without exception (even for a child and in the presence of intracranial hemorrhage).
Drug therapy is the most effective method of treating dysgemia
Most often, drugs containing heparin are prescribed. When administered intravenously, its action begins immediately, which is very important for patients with acute dyshemia.
Enoxaparin sodium is a low molecular weight heparin and is prescribed if it is necessary to restore venous outflow to patients suffering from allergic reactions, or for prophylaxis. The main advantage of enoxaparin is the possibility of intermittent administration of the drug, which allows the patient not to go to the hospital, but to take advantage of outpatient treatment.
Warfarin is prescribed to patients with bleeding disorders for whom heparin and enoxaparin are strictly contraindicated. The drug has a slight effect on coagulation activity, but the therapeutic effect can only be seen after a few days. Therefore, such treatment is not prescribed in the acute stages of dyscirculation. The dose of the administered drug must be carefully monitored by a doctor, so use at home is excluded. Higher doses are administered at the beginning of treatment in order to speed up the time to restore normal outflow, but at the same time, this tactic leads to an increased risk of bleeding. Treatment with warfarin should be continued for 3-6 months to obtain lasting results.
Surgical intervention to get rid of dyscirculation is prescribed in extreme cases
If the disturbances in the venous system are too severe, the doctor may recommend surgery to quickly improve the flow of blood from the brain. But surgery is prescribed only if medical methods do not work.
Types of surgical operations recommended for dysgemia:
- endarterectomy (removal of the inner lining of the affected artery);
- bypass surgery: a new blood vessel is placed near the narrowing of the vein to create a new route for blood flow;
- angioplasty: a balloon catheter is inserted into a narrow section of the artery to widen the walls and improve blood flow.
What contributes to the disease
CVI is caused by the characteristics of the circulatory system. To rise through blood vessels, blood must resist gravity. Its rise is caused by a diaphragm, the main function of which is to create a pressure difference. Help in overcoming gravitational forces is also provided by muscles, by contracting which the vein is compressed and, thus, blood is pushed through. Valves located on the walls prevent it from flowing back.
Failure in the activity of any component of this complex system impairs the outflow of blood, the vessels become overcrowded, and the pressure in them increases. Thus, venous insufficiency of the lower extremities develops.
The development of such a disease can be facilitated by:
- low mobility;
- genetic predisposition;
- obesity;
- increased intra-abdominal pressure, which can be caused by lifting heavy things, tight clothing, severe coughing and even constipation;
- overheating of the legs;
- pregnancy;
- taking hormonal contraceptives;
- heavy loads when playing sports;
- varicose veins, vascular injuries and other pathological changes in the functioning of the circulatory system of the lower extremities, previously suffered.
Forecasts for venous discirculation
The prognosis and speed of recovery will depend on several factors.
Success in treating the underlying disease that caused dysgemia
For example, the survival prognosis for dysgemia may be quite negative if the patient has had a stroke or thrombosis. But if the cause of the disease is hypertension or diabetes, the prognosis will be much better.
Presence of hypoxia
The prognosis will be poor if venous discirculation previously led to hypoxia. Even after eliminating dysgemia, sudden loss of consciousness or problems with the musculoskeletal system are possible.