Two centuries have passed since the French physician Rene Laeneck created the first device for listening to a patient's heart - a stethoscope. A year later, cardiac auscultation began to be practiced by attending physicians. Guides for mastering the technique have appeared.
Modern doctors have a fairly serious diagnostic base, based on precise and sensitive devices. However, the novice doctor is still required to be able to independently apply basic methods and make a preliminary diagnosis, guided by his own senses.
Medical students study ways to approach a patient, learn to evaluate individual symptoms and their significance in pathology. This course is called propaedeutics. It represents a preclinical opportunity to study minimal human examination and how to interpret the results.
What methods should a doctor know?
Narrow medical specialization does not exclude the general training of a general practitioner. The standard set of knowledge and skills of a novice doctor necessarily includes:
- personal examination of the patient;
- palpation - palpation of a dense organ, edge to determine consistency and size; pulse, area of the heart - to determine the shock wave, the force of the heart impulse;
- percussion - determining the boundaries of dullness by the nature of the sound obtained by tapping a finger over organs of different densities;
- Auscultation - listening to standard points of the body located above zones that are as close as possible to the movement of fluid inside hollow organs; the occurrence of noise depends on the speed of flow and obstacles.
Let us consider the possible results of using propaedeutics methods in the diagnosis of cardiac pathology.
Shift of the apical impulse to the left and down indicates left ventricular hypertrophy
What can a doctor reveal during a routine appointment?
During the appointment, the doctor’s attention is drawn to:
- skin tone, color of the patient's lips - pallor indicates spasm of peripheral vessels, cyanosis of lips, fingers, ears - indicates circulatory failure;
- swelling - edema of cardiac origin is characterized by a dense consistency and localization on the lower part of the body;
- dilated venous vessels on the legs and arms - indicate varicose veins, congestive insufficiency;
- pulsation of the neck veins and carotid arteries - characteristic of congestion in the small circle, aortic defects;
- in a child, the part of the sternum protrudes forward (heart hump) - occurs in cases of congenital or acquired defect against the background of a significant increase in the cavity of the ventricles.
Palpation of the heart area allows:
- determine the apical impulse, a displacement in the fifth intercostal space to the left of more than 1 cm from the midclavicular line indicates an expansion of the border, an enlargement of the left ventricle;
- placing your hand on the base in the area of the clavicles and 1st intercostal space, you can feel a characteristic tremor like a “cat’s purr” when the aorta narrows, and at the apex there is a diffuse dome-shaped push.
Percussion establishes the approximate boundaries of cardiac dullness. It can be used to judge the enlargement of the ventricles and vascular bundle.
Auscultation pattern in various heart diseases
Cardiovascular pathologies in most cases are accompanied by disturbances in intracardiac hemodynamics, which is determined by auscultatory examination. The occurrence of changes is due to reorganization (restructuring) of the myocardium, replacement of the structure of the walls of blood vessels.
The most characteristic sign during auscultation of a hypertensive patient is emphasis (intensification) of the second tone over the aorta , which is due to a significant increase in tension in the left ventricle. Upon percussion in such a patient, an expansion of the boundaries of cardiac dullness is detected. In the initial stages of the disease, the doctor hears an increase in the first tone at the apex location.
Heart defects are a set of pathologies that are caused by damage to the structural apparatus of the valve. In case of organic disorders, deviations in the acoustic parameters of sound are observed. The strength of the tone changes against the background of a violent emotional shock, where a large amount of adrenaline is released. Often, when there are defects, doctors listen for specific signs:
- weakness of the bicuspid valve - disappearance of the first sound, strong systolic murmur in the area of the apex of the heart - a standard auscultation set for such a pathology;
- bicuspid valve stenosis - the first sound has a flapping character, the second bifurcates. The third tone is partially manifested in this;
- weakness of the aortic - murmur in the sixth place of listening to the heart valves, weakening of all sounds;
- Aortic valve stenosis - weakening of the tone, against the background of which a strong systolic murmur appears in the area of the second intercostal space on the right.
During a physical examination of a patient with arrhythmia, the doctor listens for erratic and chaotic tones of varying volumes that do not always correspond to the heartbeat. More often, the doctor observes systolic and diastolic murmurs, and a quail rhythm is possible. The listening points for heart valves during fibrillation are complemented by auscultation of the neck vessels to determine the return of blood (regurgitation).
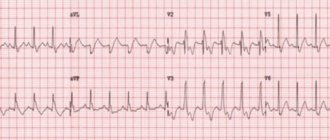
A more effective clinical tool in such a situation is an ECG with a conclusion from a functional diagnostician.
Features of auscultation technique
Cardiac auscultation was first performed with a stethoscope. This is a small wooden tube with funnel-shaped extensions at the ends. Subsequently, a phonendoscope with a combined membrane-bell-shaped head was invented to amplify low- and high-frequency sounds.
Doctors insert tubes into both ears and try to detect the slightest sound abnormalities. A prerequisite for auscultation is silence, since sounds from the outside make it difficult to distinguish those coming from the heart.
The perception of the sound signal is disrupted for subjective reasons:
- when the doctor is tired;
- in old age.
This is a serious drawback of the method. The patient has to be listened to again, examined lying down, standing, after squats. Currently, stethoscopes with the function of amplifying the sound signal and filtering noise are being prepared to replace phonendoscopes. Such auscultation will become more objective and reliable.
However, this does not relieve the doctor of responsibility for gaining experience in recognizing heart sounds and murmurs.
Standard cardiac auscultation technique
The technique of listening to the heart is simple, but requires adherence to a certain sequence. Doctors learn the algorithm of actions from their student years and carry it out without thinking.
The procedure begins by asking the patient to remove outer clothing. If there is abundant vegetation on the chest, the hairs are moistened with water or cream. Listening points were selected based on the minimum distance between the area under study and the phonendoscope head. The standard provides 5 points as a mandatory set, but in case of pathology it is possible to use others.
Before listening to each point, the doctor “commands”: “Take a deep breath, exhale everything and hold your breath!” As you exhale, the air layer of the lung tissue contracts, and the heart “comes closer” to the chest. Consequently, the sound will be clearer and stronger.
The same effect is expected from listening in the left lateral position. To increase the intensity, it is sometimes suggested to strain or do several squats.
The norms for the location of the studied areas and their projection onto the chest are known, but the doctor is recommended to check himself with preliminary palpation, this way it is possible to adjust the optimal option
Auscultation sequence:
- in the area of the apical impulse - the mitral valve and the left atrioventricular orifice are examined;
- to the right of the sternum in the second intercostal space - the mouth of the aorta and the work of the aortic valve;
- to the left of the sternum in the second intercostal space - listen to the pulmonary valve;
- above the base of the xiphoid process in the lower part of the sternum - the right atrioventricular foramen and tricuspid valve;
- in the third intercostal space along the left border of the sternum is the listening site for the aortic valve.
Additional areas of auscultation are:
- over the entire sternum;
- on the left in the armpit;
- on the back in the interscapular space;
- on the neck in the area of the carotid arteries.
Norilsk Interdistrict Children's Hospital
In recent years, phonocardiography has lost its importance as a method for studying the heart. It was replaced and significantly supplemented by EchoCG. However, to train students, and a number of doctors, to assess the sounds heard during heart activity, it is necessary
- knowledge of phase analysis of cardiac activity,
- understanding the origin of tones and noises and
- understanding of PCG and polycardiography.
Unfortunately, doctors often rely on the conclusion of an echocardiography specialist, shifting responsibility for the diagnosis to him.
1. HEART SOUND
During the work of the heart, sounds called tones occur. Unlike musical tones, these sounds consist of a sum of vibrations of different frequencies and amplitudes, i.e. from a physical point of view, they are noise. The only difference between heart sounds and murmurs that can also occur during heart activity is the brevity of the sound.
During the cardiac cycle, two to four heart sounds may occur. The first tone is systolic, the second, third and fourth are diastolic. The first and second tones are always there. The third can be heard in healthy people and in various pathological conditions. An audible fourth tone, with rare exceptions, is pathological. Tones are formed due to vibrations of the structures of the heart, the initial segments of the aorta and pulmonary trunk. Phonocardiography made it possible to identify individual components in the first and second heart sounds. Not all of them are heard directly by the ear or through a stethoscope (phonendoscope). The audible components of the first tone are formed after the closure of the atrioventricular valves, and the second - after the closure of the semilunar valves of the aorta and pulmonary trunk.
Cardiohemic systems. Tones are formed not only due to the vibrations of the valve flaps, as was thought in the past. To designate complexes of structures whose vibrations cause the appearance of tones, R. Rushmer proposed the term cardiohemic systems (Fig. 1,2).
The first tone occurs due to short-term, but quite powerful vibration of the cardiohemic system of the ventricles (myocardium and atrioventricular valves). The second tone is formed due to vibrations of two cardiohemic systems, consisting of 1) the aortic valve and aortic root and 2) the pulmonary valve with its initial segment. The cardiohemic system, the oscillations of which form the third and fourth heart sounds, consists of the atria and ventricles with open atrioventricular valves. All cardiohemic systems also include blood located in these structures.
1.1. Origin of tones.
The first sound occurs at the very beginning of ventricular systole. It consists of four components (Fig. 1).
The first component consists of very weak oscillations caused by asynchronous contraction of the ventricular muscles before the closure of the atrioventricular valves. At this moment, the blood moves towards the atria, causing the valves to close tightly, stretching them somewhat and bending towards the atria.
Second component. After the closure of the atrioventricular valves, a closed cardiohemic system is formed, consisting of the ventricular myocardium and the atrioventricular valves. Due to the elasticity of the valve leaflets, slightly protruding towards the atria, there is a recoil towards the ventricles, which causes vibrations of the valve leaflets, myocardium and blood in a closed system. These vibrations are quite intense, which makes the second component of the first tone clearly audible.
Rice. 1. The mechanism of formation of heart sounds according to R. Rushmer . I, II, III – heart sounds. 1-4 – components of the first tone. This figure is placed in the textbooks of Propaedeutics of Internal Diseases with distorted explanations.
Third component. After mitral valve closure, isometric tension of the ventricular muscle rapidly increases intraventricular pressure, which begins to exceed the pressure in the aorta. Blood rushing towards the aorta opens the valve, but encounters significant inertial resistance of the blood column in the aorta and stretches its proximal section. This causes a rebound effect and repeated oscillation of the cardiohemic system (left ventricle, mitral valve, aortic root, blood). The third component has similar characteristics to the second. The interval between the second and third components is small, and they often merge into one series of oscillations.
Isolating the muscle and valve components of the first tone is impractical, because the audible second and third components of the first tone are formed by simultaneous vibrations of both the heart muscle and the atrioventricular valves.
The fourth component is caused by vibrations of the aortic wall at the beginning of blood ejection from the left ventricle. These are very weak, inaudible vibrations.
Thus, the first tone consists of four sequential components. Only the second and third are audible, which usually merge into one sound.
According to A. Luizada, only 0.1 of the power of the first tone is provided by vibrations of the valve apparatus, 0.9 is provided by the myocardium and blood. The role of the right ventricle in the formation of a normal first sound is small, since the mass and power of its myocardium are relatively small. However, the right ventricular first sound exists and can be heard under certain conditions.
Second tone.
The initial component of the second tone is represented by several low-frequency vibrations, which are caused by inhibition of blood flow at the end of systole and its reverse flow in the aorta and pulmonary trunk at the very beginning of ventricular diastole before the closure of the semilunar valves. This inaudible component has no clinical significance and will not be mentioned further. The main components of the second sound are aortic (IIA) and pulmonary (IIP).
Aortic component of the second tone. As the left ventricle begins to relax, its pressure drops sharply. The blood located in the aortic root rushes towards the ventricle. This movement is interrupted by the rapid closure of the semilunar valve. The inertia of moving blood stretches the valves and the initial segment of the aorta, and the recoil force creates a powerful vibration of the valve, the walls of the initial part of the aorta and the blood located in it.
Pulmonary component of the second tone. It is formed in the pulmonary trunk similarly to the aortic. Components IIA and IIP merge into one sound or are heard separately - splitting the second tone (see Fig. 6).
Third tone.
Relaxation of the ventricles leads to a drop in pressure in them. When it becomes lower than the intraatrial valve, the atrioventricular valves open and blood rushes into the ventricles. The beginning of blood flow into the ventricles suddenly stops - the fast filling phase passes into the slow ventricular filling phase, which coincides with a return to the basal line of the left ventricular pressure curve. A sharp change in the speed of blood flow with relaxed walls of the ventricles gives several weak low-frequency oscillations - the third tone. The cardiohemic system (atria, ventricles - their walls and blood in the cavities) cannot give powerful oscillations, since at this moment both the atria and ventricles are relaxed, therefore, in order to listen to the third left ventricular sound, a number of conditions are important (see 1.5).
At the end of ventricular diastole, the atria contract, beginning a new cycle of cardiac activity. The walls of the ventricles are maximally stretched by the blood entering them, which is accompanied by a slight increase in intraventricular pressure. The recoil effect of the stretched ventricles causes a slight oscillation of the cardiohemic system (atria and ventricles with blood enclosed in them). The low intensity of oscillations is due to the fact that the tense atria are low-power, and the powerful ventricles are relaxed. The fourth tone occurs 0.09-0.12 s from the beginning of the p on the ECG. In healthy people, it is almost never heard and is usually not visible on FCG.
Rice. 2 . On the left – the mechanism of formation of the fourth heart sound; on the right – a rare case of good registration of the IV tone in a healthy person (observation by I.A. Kassirsky and G.I. Kassirsky);
Thus, during the work of the heart, the formation of four tones is possible.
Two of them have loud, easily audible components. In Fig. 4 and 5 show which phases of cardiac activity the heart sounds and their components correspond to.
1.2. The mechanism of mitral valve closure.
The rapprochement of the mitral valve leaflets begins during atrial systole due to a drop in pressure between them caused by the rapid flow of blood. An abrupt cessation of atrial systole with continued blood flow leads to an even greater drop in pressure between the leaflets, which causes almost complete closure of the valve, which is also facilitated by the formation of vortices in the ventricle, pressing the leaflets from the outside (Fig. 3). Thus, by the beginning of ventricular systole, the mitral orifice is almost completely closed, so asynchronous contraction of the ventricles does not cause regurgitation, but quickly “seals” the atrioventricular orifice, creating conditions for powerful oscillations of the cardiohemic system (the second and third components of the first sound).
Rice. 3 . The mechanism of mitral valve closure according to R. Rushmer (writing in the text).
1.3. Phases of cardiac activity (Fig. 4, 5).
The cardiac cycle is divided into systole and diastole according to the contraction and relaxation of the ventricles. In this case, atrial systole occurs at the very end of ventricular diastole (presystole).
Ventricular systole consists of four phases. At the beginning of systole, the atrioventricular valves are open, and the semilunar valves of the aorta and pulmonary trunk are closed. The phase of isometric contraction of the ventricles begins when all four valves are closed, but at the end of it the semilunar valves open, although there is still no blood flow into the aorta and pulmonary trunk (3rd component of the first sound, see Fig. 1). Expulsion of blood occurs in two phases - fast and slow.
Rice. 4. Phases of cardiac activity . 1 – QI tone = asynchronous contraction phase, 2 – isometric contraction phase, 3 – ejection phase, 4 – protodiastolic interval, 5 – isometric relaxation phase, 6 – rapid filling phase, 7 – slow filling phase, 8 – protodiastole, 9 – mesodiastole . 10 – presystole, OMK – opening of the mitral valve.
Ventricular diastole is divided into three parts:
- protodiastole, which ends with the opening (normally silent) of the atrioventricular valves;
- mesodiastole - from the opening of the atrioventricular valves to atrial systole and
- presystole - from the beginning of atrial contraction to the Q or R wave (in the absence of a Q wave) on the ECG.
In the clinical literature, both systole and diastole continue to be divided into approximately equal parts without taking into account the physiological phases, which is difficult to agree with. If for systole this does not contradict anything and is convenient for indicating where the pathological sound is located (early systole, mesosystole, late systole), then for diastole this is unacceptable, because causes confusion: the third tone and mesodiastolic murmur of mitral stenosis are incorrectly found in protodiastole, instead of mesodiastole. Hence the incorrect names: protodiastolic gallop (I, II, pathological III tone) instead of mesodiastolic (see 1.5), protodiastolic murmur of mitral stenosis instead of mesodiastolic.
Rice. 5. Phases of cardiac activity, heart sounds. The duration of the phases is given at a heart rate of ≥75/min. Black circles show closed valves, light circles show open ones. The arrows indicate the opening or closing of the valves during a phase (horizontal arrows) or during a phase change (vertical arrows). On the right, Roman numerals indicate tones, Arabic numerals indicate components of the first tone; IIA and IIP are the aortic and pulmonary components of tone II, respectively.
1.4. Characteristics of normal heart sounds.
The first and second heart sounds are usually, even in pathological conditions, heard over the entire atrial region, but they are assessed at the site of formation. The main parameters of tones are volume (intensity), duration and pitch (frequency response). The presence or absence of tone splitting and its special features (for example, clapping, ringing, metallic, etc.) are also necessarily noted. These features are called the nature of the tones. The physician usually compares the first and second sounds at each point of auscultation, but he must, and this is a more difficult task, compare the auscultated tone with its proper characteristic at a given point in a healthy person with the same age, body weight and physique as the patient.
Volume and pitch of tones. The absolute volume of tones depends on many reasons, including those not related to the heart itself. This includes the physical and emotional state of a person, physique, the degree of development of the chest muscles and subcutaneous fat, body temperature, etc. Therefore, when assessing the volume of a tone, many points must be taken into account. For example, muffled tones in an obese person are a completely natural phenomenon, just like increased tones during fever.
It is necessary to take into account the unequal perception by the human ear of sounds of the same intensity but different heights. There is something called “subjective loudness”. The ear is significantly less sensitive to very low and very high sounds. Sounds with a frequency in the range of 1000-2000 hertz are best perceived. Heart sounds are very complex sounds made up of many vibrations of varying frequencies and intensities. In the first tone, low-frequency components predominate, in the second - high-frequency components. In addition, when strong pressure is applied to the skin with a stethoscope, it stretches and, becoming a membrane, dampens low-frequency components and enhances high-frequency components. The same thing happens when using a tool with a membrane. Therefore, the second tone is often perceived as louder than it actually is. If on FCG in a healthy person, when recording from the apex of the heart, the first tone always has a greater amplitude than the second, then when listening, one may get the impression that their volume is the same. And yet, more often the first sound at the apex is louder and lower than the second, and on the aorta and pulmonary trunk the second sound is louder and higher than the first.
Duration of tones. This parameter cannot be assessed by ear. Although the first tone on a PCG is usually longer than the second, their audible components may be the same.
Splitting of normal heart sounds. Two loud components of the first tone usually merge into one sound, but the interval between them can reach a significant value (30-40 ms), which is already perceived by the ear as two close sounds, i.e., as a splitting of the first tone. It does not depend on breathing and is constantly heard directly by the ear or through a stethoscope with a small-diameter funnel (even better through a rigid stethoscope), if it is not pressed tightly against the patient’s body. Splitting is heard only at the apex of the heart.
The time interval between the closure of the mitral and tricuspid valves is normally small, usually 10-15 milliseconds, i.e. the cardiohemic systems of both ventricles fluctuate almost simultaneously, therefore in healthy people there is no reason for splitting the first sound, due to a slight lag of the right ventricular first sound from the left ventricular one , especially since the power of the right ventricular tone is negligible in comparison with the left ventricular tone.
The splitting of the second tone in the area of the pulmonary artery is heard quite often. The interval between the aortic and pulmonary components increases during inspiration, so the splitting is well heard at the height of inspiration or at the very beginning of expiration for two to three cardiac cycles. Sometimes it is possible to trace all the sound dynamics: an unsplit second tone, a slight split during inspiration, when the IIA-IIP interval is barely perceptible; a gradual increase in the interval to the height of inspiration and again the convergence of components IIA and IIP and a continuous tone from the second third or middle of exhalation (see Fig. 6).
| Rice. 6. Scheme of graphical recording of the main dimensions of relative dullness of the heart and the results of assessing tones at three points of auscultation : 1 – apex, 2 – aorta, 3 – pulmonary trunk, I and II – heart sounds. On the pulmonary artery, the second tone splits at the height of inspiration and merges on exhalation (third cycle). A – aortic component, P – pulmonary component of the second tone. |
The splitting of the second tone during inspiration is due to the fact that due to
negative intrathoracic pressure, the thin-walled right ventricle is filled more with blood, its systole ends later, and therefore, at the beginning of ventricular diastole, the pulmonary valve closes significantly later than the aortic valve. The splitting is not heard with very frequent and shallow breathing, because in this case, hemodynamic changes leading to splitting do not occur.
This phenomenon is especially well heard in young people with a thin chest wall during quiet deep breathing. When listening to the pulmonary trunk in healthy people, the frequency of splitting the second tone is about 100% in children, 60% in patients under 30 years old, and 35% in people over 50 years old.
1.5. Changes in tones.
Changing the volume of tones.
When auscultating the heart, an increase or decrease in both tones can be noted, which may be due to both the characteristics of the conduction of sounds from the heart to the auscultation point on the chest wall, and an actual change in the volume of the tones.
Impaired conduction of sounds and, consequently, weakening of tones is observed when the chest wall is thick (large mass of muscles or a thick layer of fat, edema) or when the heart is pushed away from the anterior chest wall (exudative pericarditis, pleurisy, emphysema). Intensification of tones, on the contrary, occurs with a thin chest wall, in addition, with fever, after physical exertion, with excitement, thyrotoxicosis, if there is no heart failure.
A weakening of both tones, associated with the pathology of the heart itself, is observed with a decrease in myocardial contractility, regardless of the cause.
A change in the volume of one of the tones is usually associated with pathology of the heart and blood vessels. Weakening of the first tone is observed when the cusps of the mitral and aortic valves are not tightly closed (the period of closed valves is absent in both mitral and aortic insufficiency), when the contraction of the left ventricle is slowed down (myocardial hypertrophy, myocarditis, heart failure, myocardial infarction, complete blockade of the left bundle branch His, hypothyroidism), as well as with bradycardia and prolongation of pQ.
It is known that the volume of the first sound depends on the degree of divergence of the mitral valve leaflets at the beginning of ventricular systole. With a large divergence, there is a greater deflection of the valves in the period of closed valves towards the atria, a greater recoil towards the ventricles and a more powerful oscillation of the cardiohemic system are observed. Therefore, the first tone becomes weaker as pQ increases and strengthens as pQ shortens.
Strengthening of the first tone is mainly due to an increase in the rate of increase in intraventricular pressure, which is observed with a decrease in its filling during diastole (mitral stenosis, extrasystole).
The main reasons for the weakening of the second sound in the aorta are: violation of the tightness of the closure of the semilunar valve (aortic valve insufficiency), with a decrease in blood pressure, as well as with a decrease in the mobility of the valves (valvular aortic stenosis).
Accent II tone. It is assessed by comparing the volume of the second tone in the second intercostal space at the edge of the sternum, respectively, on the right or left. The emphasis is noted where the second tone is louder, and can be on the aorta or on the pulmonary trunk. The accent of tone II can be physiological or pathological.
The physiological emphasis is age-related. It is heard on the pulmonary trunk in children and adolescents. It is usually explained by the closer location of the pulmonary trunk to the site of auscultation. The emphasis on the aorta appears by the age of 25-30 and somewhat intensifies with age due to the gradual thickening of the aortic wall.
We can talk about a pathological accent in two situations:
- when the accent does not correspond to the proper point of auscultation according to age (for example, a loud II sound on the aorta in a young man) or
- when the volume of the second tone is greater at a point, although corresponding to age, but it is too high in comparison with the volume of the second tone in a healthy person of the same age and build, or the second tone has a special character (ringing, metallic).
The reason for the pathological emphasis of the second tone on the aorta is an increase in blood pressure and (or) compaction of the valve leaflets and the aortic wall. An emphasis on the second tone on the pulmonary trunk is usually observed in pulmonary arterial hypertension (mitral stenosis, cor pulmonale, left ventricular failure, Aerza disease).
Pathological splitting of heart sounds.
A distinct splitting of the first heart sound can be heard during right bundle branch block, when excitation is carried out significantly earlier to the left ventricle than to the right, so the right ventricular first sound is noticeably behind the left ventricular one. In this case, the splitting of the first tone is better heard in cases of right ventricular hypertrophy, including in patients with cardiomyopathy. This sound pattern resembles the systolic rhythm of a gallop (see below).
With pathological splitting of the second tone, the interval IIA - IIP is 0.04 s, sometimes reaching 0.1 s. The splitting may be of the normal type, i.e. increase on inspiration, fixed (independent of breathing) and paradoxical when IIA appears after IIP. Paradoxical clefting can be diagnosed only with the help of a polycardiogram, including an ECG, PCG and a carotid sphygmogram, the incisura of which coincides with IIA.
Three-part (three-beat) rhythms.
Rhythms in which, in addition to the main tones I and II, additional tones (III or IV, the tone of the opening of the mitral valve, etc.) are heard, are called three-term, or three-beat.
A three-part rhythm with a normal third tone is often heard in young healthy people, especially after physical activity in a position on the left side. The third tone has a normal characteristic (quiet and low - dull) and should not raise suspicion of pathology. Often the third sound is heard in patients with a healthy heart who have anemia.
Gallop rhythms . A pathological third tone is observed when the contractility of the left ventricular myocardium is impaired (heart failure, myocardial infarction, myocarditis); with an increase in volume and hypertrophy of the atria (mitral defects); with any increase in the diastolic tone of the ventricles or their diastolic rigidity (severe hypertrophy or cicatricial changes in the myocardium, as well as with peptic ulcer disease).
The three-part rhythm with a weakened 1st tone and a pathological 3rd tone is called the protodiastolic gallop rhythm, because with tachycardia, it resembles the clatter of the hooves of a galloping horse. However, it should be noted that the third tone is in the mesodiastole, i.e. we are talking about the mesodiastolic gallop rhythm (see Fig. 4.5).
The presystolic gallop rhythm is caused by the appearance of the IV tone, when the IV, I and II tones are successively heard. It is observed in patients with a significant decrease in ventricular myocardial contractility (heart failure, myocarditis, myocardial infarction), or with severe hypertrophy (aortic stenosis, hypertension, cardiomyopathy, Fig. 7).
Fig.7. Loud IV tone in a patient with hypertrophic cardiomyopathy. The upper curve of the FCG, on the low-frequency channel (middle curve), oscillations of the IV and I tones practically merge, at medium frequencies they are clearly separated. During auscultation, a presystolic gallop rhythm was heard, and the IV tone was determined by palpation.
A summation gallop is observed in the presence of III and IV tones, which merge into one additional tone.
A systolic gallop is heard when an additional tone appears after the first sound. It can be caused by a) the impact of a stream of blood on the aortic wall at the very beginning of the ejection period (aortic stenosis, see Fig. 16; hypertension, atherosclerosis) - this is an early systolic click or b) prolapse of the mitral valve leaflet into the atrium cavity (late systolic click, it appears in the middle or at the end of the expulsion phase).
Quail rhythm . With mitral stenosis, the opening tone of the mitral valve is often heard, which resembles a click. It often occurs 0.7-0.11 s from the onset of the second sound (the earlier, the higher the pressure in the left atrium). Presystolic murmur, clapping sound I, tone II and an additional sound of the mitral valve opening - all this resembles the singing of a quail: “sssssssssssssssssssssssssssssssssss.”
Pericardial tone in adhesive pericarditis is explained by the sudden cessation of ventricular filling due to the pericardial adhesion, an armor that limits further expansion of volume. It is very similar to the mitral valve opening click or third sound. Diagnosis is carried out based on a set of symptoms, both clinical and obtained using instrumental methods.
In conclusion of the first part of “Auscultation of the Heart”, dedicated to heart sounds, it should be noted:
We listen and evaluate short sounds - the sounds that arise from the heart, not the valves. Three auscultation points are sufficient to evaluate tones.
Diastole is divided into protodiastole, mesodiastole and presystole, taking into account
physiological mechanisms of the heart, and not by dividing it into 3 equal parts.
What does sound analysis provide?
Diagnostics requires identifying sounds that do not correspond to the norm. Therefore, an experienced doctor must be able to distinguish the “music” of regular heart contractions from pathological ones.
The muscular and valvular apparatus of the heart are in constant hard work. By driving a mass of blood from the chambers into the vessels, they cause vibration of nearby tissues and transmit sound vibrations to the chest from 5 to 800 Hz per second. The human ear can perceive sound in the range from 16 to 20,000 Hz, with the best sensitivity between 1000 and 4000 Hz. This means that a person does not have enough capabilities for an accurate diagnosis. It takes practice and attention. Heard sounds must be perceived as information. Having received it, the doctor must:
- evaluate the origin in comparison with the norm;
- suggest the causes of violations;
- characterize.
How tones are formed, interpretation of deviations from the norm
Be sure to listen to two interconnected beats at each point. These are heart sounds. All healthy individuals have them. It is less common to hear the third and even fourth tone.
The first sound is called systolic; it consists of several components:
- atrial function;
- muscular - caused by vibrations of the tense muscles of the ventricles;
- valvular - considered the main component, formed by the oscillating leaflets of the atrioventricular valves;
- vascular - includes the walls of the aorta and pulmonary artery and their valve apparatus.
Based on the nature of its sound, it can be classified as:
- deaf - with left ventricular hypertrophy, myocarditis, cardiosclerosis, dystrophic changes;
- quiet, “velvet” - with myocardial infarction;
- weak, as if coming from afar - with exudative pleurisy, emphysema, significant thickness of the chest wall;
- loud, clapping - with neurosis, thyrotoxicosis, stenosis of the left atrioventricular orifice, anemia, high fever, extrasystole;
- bifurcated - with bundle branch block, thyrotoxicosis, aneurysm in the apex of the heart, myocardial dystrophy.
The second sound is formed at the beginning of diastole, caused by the slamming of the semilunar valves of the pulmonary artery and aorta. In a healthy person it is concentrated on the aorta. In cases of “pulmonary heart” with hypertension in the pulmonary circle - on the pulmonary artery.
With atherosclerotic lesions of the aorta, vasodilation, the second tone rings and resonates. Bifurcation is observed with aortic aneurysm and mitral stenosis.
You can visually register noises and tones using a phonocardiogram (bottom line), it must be written along with the ECG
The appearance of the third tone creates an auditory picture of a “gallop rhythm”. It is believed that it is formed due to the rapid decrease in the tone of the flabby walls of the ventricles in the diastole phase. In children and adolescents it is heard more often than in adults and indicates functional inferiority of the myocardium, since pathology is not detected.
For persons 30 years of age and older, it is a characteristic sign of hypertension, cor pulmonale, myocarditis, cardiosclerosis, myocardial infarction and aortic aneurysm.
Why do they listen to the heart?
The study of circulatory sounds (hemodynamics) is a quick and technically simple procedure that helps to obtain a huge amount of information about the functioning of cardiac structures.
Listening to tones is the main, but not the only purpose of auscultation. During contact with the patient, the doctor assesses heart rate, rhythm, timbre, and pathological noises.
The listening technique is used to study such changes:
- ventricular hypertrophy;
- myocarditis;
- ischemic disease (IHD);
- heart defects;
- myocarditis;
- arrhythmia;
- pericarditis.
The auscultation technique is used both for adults and in pediatric practice. An accessible and absolutely safe method helps to suspect abnormalities during the initial examination and promptly refer the child for a detailed examination.
In addition, auscultation is used to assess the condition of the fetus, which is important in the early stages of pregnancy without risk to the child and mother. In the future, the cardiovascular system of a newborn is a new object for “listening” to the heart and lungs.
Why is there a murmur in the heart?
Heart murmurs can be compared to the sounds of fluid flowing through a pipe. The turbulence depends on the roughness of the walls, flow speed, and encountered obstacles (constriction areas). The heart murmur will be louder if the obstruction is dense enough and located close to the outlet.
Vortex noises have different shades:
- gentle,
- weak,
- rude,
- whistling,
- hissing,
- howling,
- "mosquito squeak"
The lower the viscosity of the blood, the greater the speed of its movement and the noise caused. The structure of the valves (tensioned tendon threads, vibrations of the valves) can cause additional vortex flows.
Murmurs in the systole and diastole phases significantly depend on the narrowing of the atrioventricular, aortic and pulmonary openings. In aortic stenosis, blood passing through the narrowed canal during systole causes a systolic murmur. Insufficiency of the aortic or mitral valve causes backflow into incompletely closed gaps.
Types of noises and their significance in diagnosis
All noises, depending on the phase of cardiac contraction, are divided into:
- systolic - heard in case of tricuspid and bicuspid valve insufficiency, stenosis of the pulmonary artery and aorta;
- diastolic - formed due to insufficiency of the valves of the main vessels, stenosis of the atrioventricular orifices.
The nature of the noise has diagnostic significance. Noises of organic origin associated with heart defects have more “musical” properties. Thus, listening to a patient with septic endocarditis reveals a diastolic murmur on the aorta with a howling or whistling tone. This indicates a perforation with separation of the valve leaflet.
For the congenital defect of patent ductus arteriosus, a noise similar to “the rumble of a train in a tunnel” is typical.
To identify the place of greatest sound, palpation is carried out at the same time, the patient is listened to in the interscapular area, above the carotid arteries.
Cardiopulmonary murmurs are rare due to emptying during systole and decreased ventricular size. At the same time, the adjacent section of lung tissue expands and sucks air from the bronchus. The noise is heard at the height of inspiration.
Murmurs of pericardial origin are not audible in a healthy person. A creaking sound accompanies both systole and diastole. Indicates overirritation of the enlarged heart and friction of the pericardial layers.
Decoding the results
The results of cardiac auscultation in a healthy and sick person are significantly different. If the activity of the valves is not impaired, the doctor hears a “melody”, which consists of alternating abrupt sounds. The strict sequence of tension and relaxation of the myocardium is called the cardiac cycle.
The physiology of the concept consists of three stages:
- Atrial systole. The first stage lasts no more than 0.1 seconds, during which the muscle tissue of the heart chamber is tensed.
- Ventricular systole. Duration – 0.33 seconds. At the peak of myocardial contraction, the chamber takes the shape of a ball and hits the chest wall. At this moment, the apex beat is recorded. Blood is expelled from the cavities into the vessels, after which diastole begins and the fibers of the ventricular myocardium relax.
- The last phase is muscle tissue relaxation for subsequent blood intake.
The sounds described above are called tones. There are two of them: the first and the second. Each has acoustic parameters that are determined by the characteristics of hemodynamics (blood circulation). The occurrence of a heart sound is determined by the speed of the myocardium, the degree of filling of the ventricles with blood and the functional state of the valves. The first tone characterizes the systolic phase (expulsion of fluid from the cavities), the second - diastole (relaxation of the myocardium and blood flow). The heart rhythm is characterized by a high degree of synchronization: the right and left halves interact harmoniously with each other. Therefore, the doctor hears only the first two tones - this is the norm. In addition to the first two, there are additional sound elements - the third and fourth tones, the audibility of which indicates pathology in an adult, depending on the points of listening to the heart where the disorder is determined. The third is formed towards the end of ventricular filling, almost immediately after the end of the second. There are several reasons for its formation:
- deterioration of muscle contractility;
- acute myocardial infarction;
- angina pectoris;
- atrial hypertrophy;
- neuroses of the heart;
- cicatricial organic tissue changes.
The fourth pathological tone is formed immediately before the first, and in healthy people it is extremely difficult to hear. It is described as quiet and low frequency (20 Hz). Observe when:
- decreased contractile function of the myocardium;
- heart attack;
- hypertrophy;
- hypertension.
The sounds produced when blood moves through the narrowed lumen of blood vessels are called heart murmurs. Normally, noise does not occur and is heard only in cases of valve pathology or various septal defects. There are organic and functional noises. The former are associated with structural valve defects and vasoconstriction, and the latter with age-related changes in anatomy, which must be taken into account when auscultating the heart in children. A child with such murmurs is considered clinically healthy.
Typical results of auscultation of the heart are normal (in an adult): the tones are clear, sonorous, rhythmic, there are no pathological noises.