Today, the diagnosis of vegetative-vascular dystonia (VSD) is being made less and less often to patients, but not because humanity has been able to completely defeat this disease, but because this formulation is outdated. Vegetative-vascular dystonia means dysfunction of the autonomic nervous system, which is not an independent disease, but is only a consequence of pathological changes in the body.
In the latest edition of ICD-10 there is no such disease as VSD. The disorders characteristic of it are called by the more modern and precise term “somatoform autonomic dysfunction of the nervous system.” But for simplicity of presentation and understanding, we will further use the more familiar concept of VSD.
What is VSD
The autonomic nervous system, also called the autonomic nervous system, is part of the nervous system of the human body. It is responsible for controlling the activity of internal organs, metabolic processes occurring in the body, the functioning of blood and lymphatic vessels, as well as the activity of the endocrine glands. Thus, the autonomic nervous system plays an important role in maintaining homeostasis (constancy of the internal environment) and adaptation to changing environmental conditions.
The autonomic nervous system is responsible for the innervation of the entire body, organs and tissues. Moreover, its work is in no way subordinate to the will of a person, but is controlled independently of desires by the cerebral cortex. That is, a person cannot voluntarily stop the heart or influence the speed of intestinal peristalsis.
Autonomic nerve centers are also located in the brain stem, hypothalamus and spinal cord. Therefore, any disturbances in these organs are directly reflected in the quality of functioning of the autonomic nervous system, and can lead to the development of autonomic disorders.
Thus, all vital processes of the body are under the control of the autonomic nervous system, namely:
- heart rate;
- blood pressure level;
- thermoregulation;
- activity of salivary, sweat, endocrine glands;
- frequency and depth of breathing;
- digestion of food and intestinal motility;
- the condition of the smooth muscles of internal organs and the walls of blood vessels;
- processes of growth and reproduction;
- metabolic processes;
- urination, etc.
Anatomically and functionally, the autonomic nervous system is divided into 3 sections:
- Sympathetic - responsible for metabolism, energy consumption and mobilization of forces for active activity. Its sphere of influence includes heart function and blood pressure levels. Therefore, the sympathetic department allows the human body to prepare as much as possible for fight or active work.
- Parasympathetic - regulates the functioning of organs mainly during sleep and passive rest, and is responsible for restoring spent energy reserves. It is responsible for reducing heart rate, blood pressure and increasing peristalsis, which makes it possible to replenish energy reserves from food received.
- Metasympathetic - ensures communication between internal organs and the preservation of local autonomic reflexes.
All parts of the autonomic nervous system are in a certain relationship with each other, which ensures proper regulation of the body’s functioning. At the same time, the most important organs from the point of view of life support have double innervation with the opposite effect. But when the slightest deviation from the norm occurs, under the influence of stress, the balance between the sympathetic and parasympathetic departments is disrupted, which leads to the predominance of one of them over the other. The result of this is the development of vegetative-vascular dystonia.
Vegetative-vascular dystonia is a syndrome that combines various disorders of autonomic functions that are the result of impaired neurogenic regulation. This occurs when the balance between the activity of the sympathetic and parasympathetic parts of the autonomic nervous system is disturbed, which can be due to the action of a huge variety of the most disparate causes.
Thus, VSD is a multifactorial disorder that can be regarded as one of the symptoms of an existing neurological or somatic disease and consists of changes in the functioning of internal organs. Sometimes the root cause of the development of vegetative-vascular dystonia cannot be established.
Vegetative-vascular dystonia is often also called cardioneurosis, dysvegetosis, neurasthenia and some other terms.
Neurocirculatory dystonia: what is it?
This condition is one of the most common reasons for visiting a cardiologist and neurologist.
At different ages, from a third to a half of all registered pathologies of the cardiovascular system are precisely neurocirculatory dystonia. It has been noted that most often it occurs in young and middle age, from adolescence to 45 years. There are also gender differences - in women the disease is registered much more often. Neurocirculatory dystonia in children most often develops in adolescence during puberty, when the body is rebuilt and all regulatory processes, including the functions of the cardiovascular system, undergo significant changes. Psycho-emotional stress, which often accompanies puberty, also plays an important role. Pathogenesis of neurocirculatory dystonia
The essence of neurocirculatory dystonia is a violation of control of the cardiovascular system by the nervous and endocrine systems. It is neurohumoral control that ensures homeostasis by maintaining balance in the sympathetic-adrenal, cholinergic, histamine-serotonin and other systems that regulate numerous vital processes of the human body. In case of failures in the complex regulatory system, which can be caused by a variety of influences, the interaction of the hypothalamic-pituitary system and peripheral endocrine glands is disrupted, the acid-base state of biological media, and all types of metabolism change. The myocardium is very sensitive to these changes, therefore it reacts with changes in contractile function, and vascular tone also changes. A stable response to the action of various factors is gradually formed - a symptom complex of neurocirculatory dystonia of a certain type, appearing in certain circumstances.
Types of neurocirculatory dystonia
The classification of neurocirculatory dystonia is based on the leading symptom of the disease. There are 4 main types:
- Neurocirculatory dystonia of the cardiac type (disturbance of the heart comes to the fore).
- Neurocirculatory dystonia of the hypotonic type develops when the balance shifts towards the parasympathetic nervous system (vagotonia). The main symptom is a decrease in blood pressure (BP).
- Neurocirculatory dystonia of the hypertensive type is a predominance of the sympathetic nervous system (BP increases).
- Neurocirculatory dystonia of a mixed type (changes in blood pressure in one direction or another are combined with disturbances in the functioning of the heart).
In practical medicine, a classification of neurocirculatory dystonia according to severity is used. There are: mild, moderate and severe degrees.
Causes of vegetative-vascular dystonia
VSD can develop against the backdrop of a huge number of diverse factors. Among them are especially distinguished:
- psychological – severe or constant stress, depressive states;
- physical – severe physical fatigue, exposure to vibration, high temperatures, sunstroke;
- chemical – addiction to alcohol, nicotine, narcotic substances, taking a number of medications, in particular those containing ephedrine, caffeine, bronchodilators;
- changes in hormonal levels - adolescence, pregnancy and lactation, menopause, use of hormonal contraceptives, especially with frequent periods of withdrawal;
- infectious – acute and chronic diseases of the respiratory system, kidneys, brain;
- neurological disorders - Parkinson's disease, traumatic brain injury;
- endocrine diseases – diabetes mellitus, thyrotoxicosis;
- pathologies of the cardiovascular system - arterial hypertension, coronary artery disease.
It is believed that the main cause of the development of VSD is stress.
But not all people who have even several of the listed diseases develop vegetative-vascular dystonia. Women suffer from it 2 times more often than men, and almost half of all cases of VSD diagnosis occur in young girls who have not yet turned 25 years old. And only 33% of women with vegetative-vascular dystonia are over 25 years old.
Heredity plays a significant role in assessing the risk of VSD. Very often it first appears in childhood or adolescence. As one gets older, the disorder can be compensated and the attacks disappear. But the impact of negative factors can reverse the situation and again provoke the occurrence of vegetative-vascular dystonia.
The impetus for its development can be:
- psychological characteristics of the individual, especially suspiciousness and a tendency towards hypochondria;
- unfavorable socio-economic, environmental conditions (lack of sunlight, sedentary lifestyle, lack of funds, lack of nutritional culture, consumption of cheap, low-quality products, etc.);
- intrauterine pathologies - infections, hypoxia, fetoplacental insufficiency, rhesus conflict, etc.
Sometimes VSD is a transient reaction to any strong emotional shocks or emergency situations.
Causes and mechanism of action
Hereditary predisposition is considered one of the main causes of vegetative-vascular dystonia (especially in childhood). In combination with unfavorable external factors, it affects the state of the brain (in particular the hypothalamus), increasing the manifestations of the syndrome. The development of psychoneurological disorders leads to excessive activation of some processes and inhibition of others. This state of the body has a negative impact on various systems and organs. In adolescence, this is especially evident at the neurophysiological level. The causes and symptoms of VSD in adults are particularly influenced by hormonal changes.
Among the risk factors for vegetative-vascular dystonia, the following are usually distinguished, having the most powerful effect:
- disruptions in the functioning of the body (endocrine disorders, pregnancy, menopause, etc.);
- consequences of past infections, injuries, as well as the presence of chronic diseases;
- bad habits (smoking, drinking alcohol, etc.);
- emotional overload, stress, etc.
Symptoms of vegetative-vascular dystonia
Thus, it is already clear that vegetative-vascular dystonia can manifest itself in radically different ways. This concept “protects” various symptoms that arise in response to disturbances in the functioning of the autonomic nervous system.
In most cases, VSD occurs latently. But under the influence of overload or other unfavorable factors, an attack develops. Often they arise suddenly and unsettle a person. They are most difficult for older people, since they usually already have a number of other diseases, which aggravates the situation.
Often there are signs of other diseases that are not directly related to the autonomic nervous system or brain. But if manifestations of disturbances in the functioning of the cardiovascular system are observed, the neurologist has good reason to assume the presence of VSD.
The most common complaints of patients who are subsequently diagnosed with vegetative-vascular dystonia are:
- headaches of varying degrees of intensity and duration, migraines;
- attacks of dizziness;
- increased sweating;
- increased heart rate;
- severe weakness, increased fatigue;
- fluctuations in body temperature;
- noise in ears;
- darkening of the eyes, sometimes followed by fainting;
- constant drowsiness;
- increased anxiety, panic attacks;
- sudden mood swings;
- obsessive syndromes, hypochondria.
A panic attack is a strong fear of imminent death that completely grips the patient. The attack begins with the onset of anxiety, which gradually increases and turns into genuine horror. This is explained by the fact that the body sends signals of danger, but does not see options for exiting the situation. The attack lasts on average 10–15 minutes, after which the patient’s well-being gradually returns to normal.
Treatment of VSD
The patient needs to consult several doctors. The first visit can be made to a therapist, who will recommend a list of tests and refer you to specialized specialists.
To rule out other diseases, the patient will need to consult the following doctors:
- cardiologist;
- endocrinologist;
- neurologist;
- psychiatrist (if necessary, after consultation with a neurologist),
- gastroenterologist;
- pulmonologist and others.
If specialized doctors do not find any serious diseases in the patient, they prescribe treatment. In most cases, it is aimed at relieving symptoms. Medicines relieve anxiety, spasms, improve blood circulation in the head, and regulate blood pressure. In addition to medications, the patient is recommended to undergo physical therapy. They eliminate pain, metabolic disorders, and restore vascular tone.
Along with taking medications, massage and acupuncture give good results. If necessary, the patient is referred for consultation to a psychologist, who helps to cope with fears, overcome internal complexes, and solve life problems that have caused a stressful state. Patients are advised to rest, light physical activity (if the patient leads a sedentary lifestyle), walks in the fresh air, and sanatorium treatment for vegetative-vascular dystonia.
Treatment of VSD in women
Women are more often susceptible to disorders of the autonomic nervous system. The cause is emotionality, an acute reaction to stressful life situations, nervous overstrain, fluctuations in hormone levels in adolescence, during pregnancy or menopause.
Treatment of vegetative-vascular dystonia in women is aimed at normalizing the functions of the adrenal glands, which produce stress hormones. Patients are prescribed sedatives, vitamin complexes with calcium and magnesium to strengthen the nervous system. If the cause of a disorder of the autonomic nervous system is severe stress, it is recommended to work with a psychologist or consult a psychiatrist.
Treatment of VSD in men
Representatives of the stronger sex suffer from vegetative-vascular dystonia due to physical or nervous stress at work, injuries, and bad habits. In addition to standard treatment with antidepressants and vitamin complexes, treatment of vegetative-vascular dystonia in men includes a review of the daily routine, limiting or increasing physical activity (depending on activity), and combating bad habits.
If the disorder is caused by the consequences of injury or hereditary diseases, the man will have to undergo examination and treatment aimed at eliminating the underlying pathology.
Types of VSD
The nature of the manifestation of signs of VSD directly depends on the condition of the blood vessels. Based on this, the following types of vegetative-vascular dystonia are distinguished:
- hypertensive;
- hypotonic;
- mixed;
- cardiac;
- vagotonic.
But symptoms are extremely rarely present all the time. Most often they are in the nature of attacks. Not all of the signs characteristic of a particular type of vegetative-vascular dystonia always appear. Moreover, this is rare. Typically, patients complain of 2-3 disorders, the presence of which, in combination with the results of the examinations, makes it possible to determine the specific type of vegetative-vascular dystonia.
Based on how VSD occurs, there are 3 degrees of severity of the disorder:
- mild – patients fully retain their ability to work, symptoms of VSD do not cause them significant discomfort, and there are no vegetative crises;
- moderately severe – periods periodically occur during which a person loses ability to work due to exacerbation of vegetative-vascular dystonia and the development of a vegetative crisis;
- severe - a long, persistent course of VSD with frequent periods of exacerbation and crises, which leads to a significant decrease in performance.
Hypertensive type
Patients experience pronounced vascular tone, as well as a persistent increase in blood pressure. Their main complaints focus on the occurrence of:
- rapid heartbeat;
- hot flashes;
- headaches;
- constant fatigue;
- nausea, vomiting, attacks of which are not associated with eating;
- decrease in appetite up to its complete loss;
- sweating (during an attack there is severe sweating of the palms);
- causeless but strong fear;
- flickering “flies” before the eyes.
Hypotonic type
Characterized by low blood vessel tone and low blood pressure. Therefore, patients are often annoyed by:
- episodes of darkening of the eyes;
- a sharp decrease in blood pressure;
- severe weakness;
- loss of consciousness;
- pale skin;
- nausea, heartburn;
- changes in bowel habits (diarrhea or constipation);
- inability to take a full breath.
It can be noted that in patients with VSD of the hypotonic type, the palms and feet are constantly cold.
Mixed type
With this variant of VSD, variability in vascular tone is observed, so blood pressure can fluctuate within a fairly wide range. It can rise sharply to high levels and then suddenly drop to extreme levels.
In such cases, there is a change in the symptoms of VSD, which occurs according to the hypertensive type, with manifestations of VSD of the hypotonic type. This significantly affects the lives of patients, as attacks of weakness, profuse sweating and fainting states are replaced by hot flashes, tachycardia and headaches.
During an attack, there is often a fear of imminent death and the inability to take a full breath, which further aggravates the situation. Pain in the heart area may be present.
Cardiac type
This type of VSD is diagnosed when aching, throbbing pain occurs in the heart area, which does not have a significant effect on a person’s general well-being. They may be accompanied by arrhythmia and profuse sweating, but the examinations carried out do not reveal heart pathologies.
Vagotonic type
For this type of vegetative-vascular dystonia, the occurrence of breathing disorders is typical. Patients often complain of the inability to take a full breath and a feeling of tightness in the chest. In this case, there may be a tendency to lower blood pressure and slow heartbeat. But with the vagotonic type of VSD, there is an increase in salivation and changes in the functioning of the organs of the digestive system.
Symptoms
The symptoms of neurocirculatory dystonia are very diverse and form the basis for the classification of pathology. However, it is possible to identify a number of common features that are characteristic of most types of NDC:
- frequent mood changes;
- constant fatigue and drowsiness;
- lack of strength, weakness;
- feeling of a lump in the throat;
- increased sweating;
- weather sensitivity;
- anxiety;
- feeling of lack of air, etc.
An exacerbation of the disease can be triggered by any stressful situation: an excess of positive or negative emotions, lack of sleep, or even a simple change in time zones.
How does an attack go?
During an attack of VSD, a sympathoadrenal crisis is observed, as a large amount of adrenaline is suddenly released into the blood. Then it starts suddenly. At the same time, you begin to feel your heartbeat, your blood pressure and body temperature rise. In this case, the skin may turn pale and chills may occur. This is accompanied by the appearance of strong fear for one’s own life. This condition lasts on average 20–30 minutes, but can last 2–3 hours, after which the condition gradually improves.
Attacks may occur several times a week or several times a day.
After the attack ends, the patient feels a strong urge to urinate, during which a large volume of light-colored urine is released. Fear is replaced by severe weakness, as there is often a sharp decrease in blood pressure. In some cases, this is accompanied by tremors in the legs, up to the inability to walk normally.
After an attack, people tend to become anxious and fear new episodes. Therefore, depression often occurs, which makes the situation even worse. Also, patients with VSD may tend to refuse to communicate with other people because they are ashamed of their illness and its manifestations. But at the same time, they are also afraid of not receiving much-needed medical care at the right time, which also does not help improve the situation.
Also, an attack of VSD can occur with a vagoinsular crisis. In this case, the attack begins with the appearance of pre-syncope symptoms:
- noise in ears;
- darkening of the eyes;
- sudden weakness;
- a feeling of unreality of what is happening.
These phenomena are observed for a very short period of time, and are replaced by loss of consciousness.
During a vagoinsular crisis, severe abdominal pain and a powerful, urgent desire to empty the intestines may occur. During an attack, accelerated intestinal motility, decreased blood pressure, slowed heart rate and severe sweating are observed. Patients usually complain of cold sweat with a pronounced feeling of heat. They are often overcome by indescribable melancholy and strong fear appears.
Very rarely, an attack of VSD occurs of a mixed type, in which symptoms typical of a vagoinsular and sympathoadrenal crisis are observed. Most often in such cases it is observed:
- shortness of breath, up to a feeling of suffocation;
- chest pain;
- increased heart rate;
- severe dizziness;
- unsteady gait;
- very strong fear of death;
- a feeling of unreality of what is happening.
Diagnostics
To diagnose and prescribe treatment for VSD, you must consult a neurologist. Before the consultation, it is best to make a detailed list of complaints. This will help the specialist not only detect VSD, but also suggest what caused its development. The doctor will definitely conduct a thorough survey, during which he will also find out the presence and nature of the prerequisites for the development of vegetative-vascular dystonia.
Then the neurologist proceeds to the examination. The doctor assesses the condition of the skin, measures the pulse, blood pressure, sometimes using an orthostatic test (2 measurements are taken: one in a lying position, the second after taking up a vertical position), listens to the lungs and heart. To assess the activity of the sympathetic and parasympathetic autonomic nervous system, he may pass the end of the hammer handle over the skin.
After completing the examination and assuming the presence of VSD, the neurologist must prescribe a set of studies that will help detect or confirm existing assumptions about the causes of the development of the disorder. For this purpose, patients are prescribed:
- UAC and OAM;
- blood sugar test;
- blood test for TSH, T3 and T4 (thyroid hormones);
- biochemical blood test to determine the concentration of potassium, cholesterol, creatinine, urea and other compounds;
- ECG;
- fluorography of the chest organs;
- rheoencephalography;
- MRI;
- Ultrasound scanning of neck vessels;
- EEG.
In our clinic, you can also learn in more detail about the composition of your body and the state of the vascular system, which is involved in the blood supply to internal organs, skeletal muscles, and the brain. Our experienced doctors will explain the data obtained to you in detail. Bioimpendansometry calculates the ratio of fat, muscle, bone and skeletal mass, total fluid in the body, and basal metabolic rate. The intensity of recommended physical activity depends on the state of muscle mass. Metabolic processes, in turn, affect the body's ability to recover. Based on the indicators of active cell mass, one can judge the level of physical activity and nutritional balance. This simple and quick test helps us identify disturbances in the endocrine system and take the necessary measures. In addition, it is also very important for us to know the condition of blood vessels for the prevention of diseases such as heart attacks, hypertension, heart failure, diabetes and much more. Angioscan allows you to determine such important indicators as the biological age of blood vessels, their stiffness, stress index (which indicates heart rate), and blood oxygen saturation. Such screening will be useful for men and women over 30, athletes, those undergoing long-term and severe treatment, as well as everyone who monitors their health.
Diagnosis of VSD
Due to the fact that the symptoms of the disease are very diverse, it is difficult to make an accurate diagnosis. It is important to take into account all the patient’s complaints, his medical history, as well as objective research data and the results of additional research methods.
Additionally, studies such as:
- Electroencephalography (EEG)
- Studies of blood vessels of the head and neck;
- ECG;
- Magnetic resonance imaging, etc.
In addition to the neurologist, the examination may involve such specialists as an ophthalmologist, otolaryngologist, cardiologist, endocrinologist, psychotherapist or psychiatrist and others.
Treatment of vegetative-vascular dystonia
Treatment of VSD is always selected strictly individually. In this case, the neurologist must take into account a lot of factors and formulate the optimal tactics. Not only the type of vegetative-vascular dystonia, the severity and frequency of attacks, the patient’s age, but also the presence of concomitant diseases and their characteristics are taken into account.
When prescribing treatment for patients with VSD, neurologists pursue two goals: eliminating the symptoms of vegetative-vascular dystonia and influencing the cause of the development of dysfunction of the autonomic nervous system. The second task is of particular importance, since sometimes it is not possible to find the true cause of VSD. But the patient’s quality of life in the future primarily depends on this, since by eliminating the cause of VSD, the cause itself will also be eliminated. Therefore, treatment of vegetative-vascular dystonia is often carried out not only by a neurologist, but also by other specialized specialists, in particular, a cardiologist.
Also, treatment of vegetative-vascular dystonia involves influencing the psycho-emotional state of patients, since stress and prolonged nervous tension definitely do not improve their condition.
Thus, the treatment of vegetative-vascular dystonia is always complex. It includes:
- drug therapy;
- lifestyle correction;
- psychotherapy;
- Spa treatment.
To combat the causes of VSD, manual therapy is often used. This is due to the fact that a competent effect on the spine can improve the performance of almost every organ of the human body. After all, it is in the spinal cord that the autonomic centers are located, which suffer greatly in the presence of spinal pathologies.
Therefore, the elimination of scoliosis, protrusions, herniated intervertebral discs, spondylosis and other disorders necessarily leads to a significant improvement in the condition of patients, and when treated in the early stages, a complete elimination of the causes of the development of VSD.
One of the most effective methods of manual therapy is the original Gritsenko method. With its help, you can restore the normal position of each vertebra and thereby completely normalize the functioning of the spinal cord. As a result, blood circulation also improves, back and chest pain, breathing problems, and a host of other disorders go away. An additional “bonus” is an increase in the body’s adaptive capabilities and a slowdown in the natural aging process.
When manual therapy is performed correctly, improvements are observed after the first sessions. But to consolidate the results and eliminate the causes of vegetative-vascular dystonia, you need to undergo a course of manual therapy. Moreover, sessions can be combined with work, study, business trips and other activities.
Drug therapy
Treatment of VSD involves the use of a whole range of medications, the list of which, as well as the dosage, is determined by the neurologist on an individual basis. Thus, drug therapy for vegetative-vascular dystonia may include:
- Antidepressants help eliminate excessive anxiety, increased irritability and help overcome depression, psycho-emotional stress, and apathy. Often, while taking antidepressants, there is a decrease in heart pain and muscle pain, even in cases where they previously could not be relieved by other means.
- Tranquilizers - used to reduce the risk of panic attacks, eliminate causeless fears and relieve increased anxiety.
- Sedatives - initially preference is given to herbal remedies, but if they do not have the desired effect, they are replaced with “heavy artillery”. Herbal remedies act gently; in the absence of allergies, they do not have a negative effect on the body, but have a beneficial effect on the nervous system.
- Nootropics are designed to activate blood circulation in the vessels of the brain, remove the negative effects of hypoxia (oxygen deficiency) and increase the body’s ability to resist stress.
- Adrenergic blockers are prescribed when problems with the heart are detected.
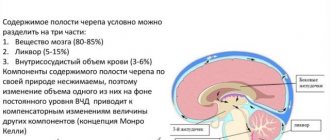
- Diuretics - used in the presence of headaches, attacks of dizziness that occur against the background of increased intracranial pressure or arterial hypertension. They help remove excess fluid from the body, but lead to a decrease in sodium levels, and some potassium levels. This can negatively affect the functioning of the heart, so diuretics are often combined with drugs that replenish the deficiency of these ions.
- Vitamin preparations containing B vitamins improve the conductivity of nerve impulses and generally have a positive effect on the state of the nervous system as a whole.
- Metabolic drugs - designed to increase control over glucose levels, have microcircular, antihypoxic properties.
Lifestyle correction
In order to improve the functioning of the autonomic nervous system, patients with VSD are recommended to reconsider their lifestyle and habits. Thus, neurologists recommend to all patients:
- Organize the correct work and rest schedule. During the workday, it is important to take breaks, leave your chair and go for a walk to improve blood flow in the body and give your head a chance to rest.
- Get enough sleep. It is recommended to sleep at least 8 hours every day.
- Walk outdoors every day. It's worth walking for about an hour. This is enough to improve the functioning of the entire body.
- Make moderate physical activity an integral part of your life. Fanatical exercise with VSD will be detrimental, but half an hour of jogging, aerobics, and swimming will be very helpful.
- Eat properly. Patients are advised to avoid foods with a high content of trans fats, which contribute to the formation of atherosclerotic plaques and also increase nervous excitability. But a strict diet for VSD is not indicated, since strict restrictions can negatively affect the psycho-emotional state of the patient, which will aggravate the course of vegetative-vascular dystonia.
Since the topic of nutrition in VSD raises many questions, it requires a more detailed consideration. With such a diagnosis, the diet should be built in accordance with the following principles:
- enriching the diet with foods that are sources of potassium and magnesium and have a positive effect on the functioning of the cardiovascular system, in particular blood pressure levels;
- normalization of water-salt balance by drinking 1.5 liters of water per day, in addition to tea, juices and other drinks;
- enjoying food;
- bringing the diet as close as possible to the requirements of a healthy diet.
The nature of the diet may vary depending on the type of vegetative-vascular dystonia. So, in case of hypertensive form, it is important to exclude foods containing large amounts of “hidden” salt. For this purpose, it is recommended to refrain from eating fast food, canned food, marinades, semi-finished products, etc. Instead, patients are asked to include soups with vegetable or weak meat or fish broth in their daily menu. It is also recommended to replace traditional wheat or rye bread with products made from whole grain flour or with bran.
With hypotonic VSD, when creating a menu, you should pay special attention to vegetables and fruits that contain increased amounts of well-absorbed vitamin C and β-carotene, as well as foods that increase blood pressure. Thus, with this form of dysfunction of the autonomic nervous system, it is worth introducing into the daily diet:
- citrus fruits, bananas, bell peppers, pineapples, pomegranate;
- any nuts, buckwheat, liver, brains;
- cheeses;
- herring;
- dark chocolate, cocoa, coffee.
With hypotonic VSD, it is not prohibited to eat white bread, potatoes and even sweets.
If a patient is diagnosed with a cardiac form of the disease, he is recommended to bring foods that are a source of magnesium and potassium to his table. This will have a positive effect on the functioning of the heart muscle and reduce the risk of developing dangerous complications. Therefore, they should pay attention to:
- oatmeal, buckwheat;
- legumes;
- onions, eggplants;
- apricots, peaches, grapes, including in the form of dried fruits;
- natural juices, compotes, jelly;
- dairy products;
- chicken eggs;
- lean varieties of fish and meat.
Psychotherapy
With vegetative-vascular dystonia, it is important not to close yourself off from the problem, but to solve it. Therefore, competent psychotherapy plays a significant role in the treatment of VSD. Psychotherapy helps you understand yourself better, become calmer and more confident.
Spa treatment
An annual holiday in a sanatorium outside the period of exacerbation of vegetative-vascular dystonia has a positive effect on the physical and psycho-emotional state of people, which helps to prolong remission. But with VSD, long trips abroad will not be the best idea. It would be more correct to choose a balneological resort in the climatic zone in which he permanently lives, since a sharp change in climate can negatively affect a person’s condition and provoke a new exacerbation of VSD.
Treatment methods for VSD
Treatment of VSD in Moscow is carried out using medication and physiotherapeutic methods. The choice depends on the characteristics of the patient’s condition and symptoms of disorders.
Drug therapy
Treatment of vegetative-vascular dystonia in adults should be comprehensive. The following groups of drugs are used for this:
- Sedatives. Medicines relax, calm, normalize sleep, and relieve anxiety. Good results are obtained with preparations based on medicinal herbs or containing synthetic relaxants (barbiturates).
- Cardiovascular. The drugs relieve arrhythmia, normalize blood pressure, and improve cerebral circulation. To increase their effectiveness, patients need to sleep at least 8 hours a day.
- Medicines to normalize the functioning of the nervous system. There are several groups of drugs. For VSD, the following are used: tranquilizers (drugs relieve anxiety), sleeping pills (normalize sleep), antidepressants (treat the symptom complex of depression, including increasing mood), neuroleptics (reduce the sensitivity of nerve endings, are used to treat severe emotional and mental arousal), nootropics ( to improve cerebral circulation).
- Vitamin complexes. The drugs normalize the balance of vitamins and minerals and strengthen the nervous system.
- Antispasmodics. Necessary for muscle weakness, stomach cramps, headaches.
- Hormonal drugs. The drugs are used if VSD has developed against the background of hormonal imbalance.
- Diuretic medications. These drugs remove excess fluid, prevent stagnation and swelling, and ensure good blood and lymph circulation.
When choosing medications, the patient’s age and existing diseases are also taken into account.
Physiotherapy
In addition to medications, the symptoms of the disorder are relieved by physiotherapeutic procedures. Treatment of vegetative-vascular dystonia in Moscow includes:
- bioresonance therapy;
- reflexology;
- Exercise therapy according to a special course of exercises;
- massage;
- acupuncture;
- laser and magnetic therapy;
- electrophoresis with sedatives;
- electrosleep;
- darsonvalization;
- aeroionotherapy.
Massage, exercise therapy, acupuncture should be carried out by specialists. Procedures are selected individually.
Prevention
After a course of VSD therapy, as well as to prevent nervous breakdown, doctors recommend the following measures to patients:
- various exercises, sports;
- walk as often as possible;
- start doing yoga, meditation, and other techniques aimed at relaxation;
- vitamin therapy courses;
- contrast shower (if there are no contraindications).
Patients are advised to avoid overexertion, find time to rest, and get enough sleep. At the first attacks or intensification of symptoms of the disorder, it is better to consult a doctor. In case of severe manifestations of dysfunction of the autonomic system, the patient is hospitalized.
Consequences of VSD
Despite the fact that vegetative-vascular dystonia manifests itself quite severely, it has a positive prognosis. Of course, the risk of developing negative consequences is directly influenced by strict adherence to medical recommendations, especially regarding adherence to a daily routine, giving up bad habits and taking prescribed medications.
With a careful approach to the treatment of VSD, the risk of developing undesirable consequences is minimal. But if the problem is ignored, patients have a high chance of later encountering:
- tachycardia;
- hypertension that cannot be treated with traditional drugs to lower blood pressure;
- cardiomyopathy;
- diabetes mellitus type 2;
- urolithiasis and cholelithiasis;
- stroke, myocardial infarction.
VSD negatively affects the immune system. Therefore, patients with this diagnosis are much more likely than others to suffer from respiratory infections. In this case, a vicious circle is formed, since in acute respiratory infections attacks are observed more often.
5 2 votes
Article rating