The word “hemorrhoids” has become widely known thanks to commercials, but, unfortunately, they give the wrong idea about its manifestation and what needs to be done if it bothers you “there”?
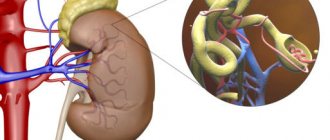
Hemorrhoids are a plexus of small veins in the submucosal layer of the rectal outlet and under the skin in the anus.
The topic is delicate, but it cannot be ignored, since with the initial manifestations the cause of concern can be eliminated quickly and inexpensively. In addition, other diseases may have symptoms similar to hemorrhoids:
- anal fissure;
- fistula;
- bleeding rectal polyp;
- benign and malignant neoplasms of the rectum and anal canal, including villous tumors;
- prolapse of the mucous membrane, rectal wall, anal sphincter insufficiency;
- parasitic infection;
- condylomas in the anal area;
- ulcerative colitis;
- Crohn's disease;
- endometriosis;
- complicated caudal teratomas;
- hemangiomas;
- acute and chronic paraproctitis (inflammation of fatty tissue around the rectum);
- allergic dermatitis;
- psoriasis;
- contact dermatitis;
- idiopathic anal itching;
- diabetes;
- pyoderma;
- diarrhea;
Often, a deceptive feeling of false “shame” prevents a person suffering from this problem from contacting a specialist, although this disease is quite common. More than 75% of adults over 45 years of age suffer from this disease to one degree or another.
Which specialist should I contact?
As you can see, the diseases are very different, and accordingly, the methods of examination and treatment of hemorrhoids are required in each case differently. In this situation, a proctologist surgeon will understand and provide assistance. The specialty “surgeon” does not at all mean that the treatment is necessarily surgical; the earlier the patient applies, the greater the chance of effectively treating hemorrhoids using a conservative method, that is, using tablets, ointments and/or rectal suppositories. And in the case of tumor diseases, it can save lives. But only a proctologist should determine this.
Proctoglivinol and Gepatrombin ® products
Suppositories sold under the name Proctoglivenol contain two active ingredients. The analgesic effect develops due to lidocaine, and the improvement in the structure of the vascular wall is due to the tribenoside included in the composition. Directions for use: 1 suppository 2 times a day during an exacerbation. As the symptoms subside, switch to a maintenance dose - 1 supp. 1 r/day.
Hepatrombin G is a remedy for complications. These suppositories have anti-edematous, antithrombotic, regenerative, anesthetic and anti-inflammatory effects. They are carried out using the following funds:
• Lauromacrogol.
• Prednisolone.
• Heparin.
Suppositories are prescribed 1-2 times a day. The course for hemorrhoids is determined individually.
When should you seek help?
- the appearance of some additional neoplasm (usually hemorrhoids) in the anus (anus), which may not hurt;
- an admixture of blood or mucus during bowel movements (defecation), which can be seen in the toilet, on toilet paper or on a towel after a hygienic shower;
- when sitting for a long time in the toilet or sitting at a table, while driving a car, nodules appear in the anus;
- burning sensation, pain or itching in the anus;
- discomfort in the anus, inside, in the rectal area, watery discharge of various types at rest or simply during the passage of gases;
- bloody discharge from the intestines even without bowel movements.
Hemorrhoids become a problem when the hemorrhoids become enlarged due to acute or chronic circulatory disorders in the venous hemorrhoidal plexuses.
They say recovery from hemorrhoid surgery is very painful?
The anus is the most sensitive and most painful area of the body. Therefore, after a radical operation, the patient is not immediately released from the clinic; first, he needs to adjust his stool and relieve pain. All this is to prevent the development of postoperative complications. Previously, when there were no modern technologies, healing was so painful that patients were kept in the hospital for three weeks, in the first days they were held back to avoid injury to the wounds during defecation, they were given antidepressants, I saw this in the 90s. And even earlier, after such radical operations, opium tincture was prescribed, which both delayed stool, because opium causes constipation, and relieved pain.
Symptoms of external hemorrhoids
External or external hemorrhoids are manifested by an increase in nodes in the anal area with pain, the appearance of blood on the napkins after using the anal area.
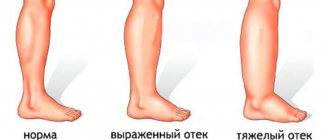
In acute cases, thrombosis of hemorrhoids with inflammation is possible, which leads to a sharp increase in hemorrhoids with swelling and an increase in pain. There are situations when the symptoms of exacerbation of hemorrhoids go away on their own in 2 - 3 days at home. If this does not happen, you need to contact a specialist. Proctologists deal with this problem. In this case, the doctor may prescribe conservative or surgical treatment for hemorrhoids.
Hemorrhoids in men and women
There is no difference between the clinical manifestations of hemorrhoids in men and women. Differences may lie in the causes of the disease. Pregnancy and childbirth increase the risk of developing hemorrhoids in women. During pregnancy, the uterus increases in size, puts pressure on the pelvic veins, and the tone of the vein walls decreases, leading to blood stagnation. The vessels in the rectum begin to dilate and this leads to the formation of hemorrhoids.
During the birth itself, intra-abdominal pressure increases, as a result of which the veins of the rectum become filled with blood and swell, and hemorrhoids may fall out.
Therefore, before planning a pregnancy, women are recommended to undergo a proctological examination in order to exclude or identify hemorrhoids at the initial stage and undergo a course of treatment. This will allow you to avoid unpleasant manifestations of the disease during such a wonderful period of life for any woman.
Men have their own risk factors for developing hemorrhoids. Men are more likely than women to engage in strength sports, and their work more often involves lifting weights. Loads significantly increase intra-abdominal pressure, and if the walls of the vessels of the rectal veins are weak, hemorrhoids may develop. Also, drinking strong alcoholic drinks provokes the development of hemorrhoidal disease.
If we talk about the differences between hemorrhoids in men and women, we can note that men are less likely to visit a proctologist in the initial stages and see a doctor when the disease is already advanced. This may be due to embarrassment, or because the man does not want to change his lifestyle, profession, or hobbies.
Diagnostics
Even with a visual examination, the doctor can figure out what the problem is with external hemorrhoids. The so-called hemorrhoidal cones will not allow you to doubt the correctness of the diagnosis. Treatment of internal hemorrhoids first involves digital examination in order to assess the condition of the internal nodes. Sometimes, if diseases in the upper intestine are suspected (for example, polyps) or to exclude cancer, anoscopy or sigmoidoscopy (visual examination of the lower intestine using a flexible endoscope) may be required.
Medical care for patients at Medical Plaza MC is developing along the path of minimizing surgical interventions. If 20 years ago, surgeons had one operation for hemorrhoids in their arsenal - the classic Milligan-Morgan operation (excision of hemorrhoids with suturing of the feeding vessels), today advertisements on all sites are replete with an abundance of new minimally invasive, “non-surgical” techniques, which are also popular Treatment of hemorrhoids is conservative.
How to get rid of hemorrhoids forever?
Coloproctology Tags:
Ekaterina Kryukova: Hello, this is the “Online Reception” channel, where we discuss a variety of medical issues. Today we are discussing the topic of how to get rid of hemorrhoids forever. Rustam Abdullaev, a coloproctologist and surgeon at the MedikCity clinic, will help me understand this issue. Hello, Rustam.
Rustam Abdullaev: Hello, Ekaterina.
Ekaterina Kryukova: How do you like these prospects, how possible are they in the case of hemorrhoids?
Rustam Abdullaev: Yes, all this is possible. You can get rid of hemorrhoids forever, there are several ways.
Ekaterina Kryukova: Let's first understand what it is.
Rustam Abdullaev: Let's first understand the causes of the disease, and then I will explain how it is all treated.
The cause of hemorrhoids is that in the anal canal there are hemorrhoids - these are formations that have a venous structure. But, unlike veins, they have a spongy structure; blood enters there through arteries and flows out through veins. When the outflow of blood is disrupted, the inflow is always maintained, because blood enters the hemorrhoidal nodes through an artery that pulsates and actively brings blood to the nodes. When a person sits, for some other reason, when the outflow is disrupted, the nodes begin to increase in size, the mucous membrane above them becomes thinner. The ligaments that hold this knot stretch and tear off, and the knots begin to fall out, bleed, etc. There are different methods for treating hemorrhoids.
Ekaterina Kryukova: Let's look specifically. We have a rectum, built-in hemorrhoids - the essence of veins that help blood circulation in the rectum.
Rustam Abdullaev: They don’t really help. In fact, this is a rudimentary formation, that is, only erect walkers suffer from hemorrhoids; four-legged animals do not suffer from hemorrhoids, because when a person stood up, the internal pressure on the terminal part of the rectum increased. In this case, the outflow suffers, while the inflow remains intact.
Ekaterina Kryukova: That is, we have an urge to go to the toilet, there is an influx, we do it, but later it drags on, formations appear, these nodes fall out.
Rustam Abdullaev: Absolutely right.
Ekaterina Kryukova: The first stage of hemorrhoids is manifested by internal nodes that have not yet fallen out and are not visible to the eye. How does this happen?
Rustam Abdullaev: There are only 4 stages. The first stage can occur without symptoms at all. They do not fall out, they can only bleed, itching and other symptoms may appear that patients do not pay attention to. Actually, they pass quickly. If the patient begins to use medications, then the first stage passes very quickly and asymptomatically. And it is very rare when a patient comes to us with the first stage of hemorrhoids. Someone is scared by blood, they come right away, and this is the right decision, because blood can not only come from nodes.
Ekaterina Kryukova: We have widespread advertising about certain candles, and men who work in the office use them as a panacea. Does this make any sense?
Rustam Abdullaev: Only in Russia there are such a number of drugs for hemorrhoids: suppositories, ointments, tablets, dietary supplements, homeopathy. Abroad, in developed countries, there are two or three types of ointments and suppositories. This is a symptomatic treatment. If a patient has complaints at the first stage, he can be prescribed treatment, but it does not eliminate the very cause of the blood outflow disorder. In this case, the disease progresses further, that is, we only relieve the symptoms. All suppositories and ointments are needed only to relieve an exacerbation. If this is thrombosis, when blood stagnates and blood clots form, then these are effective drugs, ointments or suppositories, those that dilute blood clots, with glucocorticosteroids. They help quite well in the initial stages, but this is not a radical treatment.
Only in Russia there are so many drugs for hemorrhoids. Abroad, in developed countries, there are two or three types of ointments and suppositories. This is a symptomatic treatment
Ekaterina Kryukova: Already at the first stage, we most likely won’t be able to cure it with medication? But they prescribe medications, pills for varicose veins. Can't this help and prevent hemorrhoids from progressing?
Rustam Abdullaev: There are venotonic drugs that really improve blood circulation and tones the venous walls, but this is all temporary.
Ekaterina Kryukova: Do you observe any general situations or can this happen to anyone?
Rustam Abdullaev: Who experiences it more often, women or men – it’s 50/50. In men it happens from alcohol, heavy physical exertion, poor diet, constipation, diarrhea, and so on. In women, this happens during pregnancy, the uterus enlarges, puts pressure on the lower half, which collects blood from the pelvis and veins of the lower extremities, congestion occurs, and hemorrhoids and varicose veins of the lower extremities appear.
Ekaterina Kryukova: Does a woman have hemorrhoids that arose during pregnancy and remain after?
Rustam Abdullaev: As practice shows, for some time. The fact is that during pregnancy it appears; during spontaneous childbirth, the situation can worsen; a mechanical factor is also added, that is, childbirth itself, which is quite traumatic, including for the rectum, and thrombosis of hemorrhoids can form. But after some time the symptoms go away. In the future, it still appears, for some earlier, for others later, but as a rule, this happens within 5-10 years. Patients come and undergo surgery. The easiest way is to have surgery at an early stage, but during pregnancy our hands are tied, we can only find conservative therapy, because almost all drugs that are used for treatment are transmitted through the placental barrier. Then the woman feeds, and here we can recommend expressing milk for a day, surgery, and after a day she begins to feed, that is, while we administer drugs to her, they are eliminated within 12 hours.
There is one more point, if hemorrhoids during pregnancy and after childbirth lead a woman to a fairly advanced stage. If there are small nodules, we prescribe treatment and wait until lactation ends without any problems, and then we operate. But there are cases when they come in the acute phase, when all hemorrhoids, both internal and external, are thrombosed. In this case, we recommend that the woman express milk, freeze and feed the baby so as not to stop breastfeeding. And we do the operation.
After the operation, you cannot lift weights of more than 10 kg for a month, that is, if the symptoms of hemorrhoids are relieved with medication after childbirth, the woman waits a couple of years, and the baby reaches up to 15 kg, then here we also have to refuse, because she has to lift the child, and this is the risk of postoperative bleeding.
Ekaterina Kryukova: I would like to discuss patients with constipation, this is perhaps the main risk group. Here, constipation is the root cause, or vice versa, hard feces injure the rectum. And we get hemorrhoids, plus the person is afraid to experience pain during bowel movements due to inflamed hemorrhoids, and constipation occurs.
Rustam Abdullaev: You have answered your own question.
Ekaterina Kryukova: Why does constipation occur? Is it time to go to a gastroenterologist?
Rustam Abdullaev: Constipation can cause hemorrhoids. If you have never had constipation, then the person tries to avoid pain and go to the toilet as late as possible. And this aggravates the situation, hemorrhoids begin to progress faster.
Ekaterina Kryukova: Let's go back to the stages. Bleeding may occur on the first and second.
Rustam Abdullaev: Bleeding may occur at all stages.
Ekaterina Kryukova: Bleeding is a sufficient reason to see a doctor, because we can have blood loss, anemia, and this is not much good for any person. When we see a proctologist, is a visual examination enough for us or do we need to do a rectal anoscopy? Or do they recommend some other manipulations?
Rustam Abdullaev: For the initial examination, it is recommended to conduct an anoscopy, examination of the anal canal, rectal area, terminal part of the rectum, which are not visible on colonoscopy. The anal canal is in good shape, and it is not possible to look in detail at a colonoscopy. Therefore, we perform anoscopy at the initial appointment, that is, we visualize all the processes that occur there, and prescribe rectoscopy. We prescribe it quite rarely, because we examine about 25 cm, maximum 30. We examine it with a proctoscope, which is straight and not flexible, and we can reach the splenic angle and only look at a small piece. During a colonoscopy, we get a complete picture of the entire intestine.
Ekaterina Kryukova: Why a colonoscopy, to rule out colitis?
Rustam Abdullaev: Colonoscopy is needed in order to exclude diseases that may occur with similar symptoms. A hemorrhoid or a fissure can bleed, something that we can see during the examination. Tumors and polyps can also bleed; they can produce both blood and mucus. This could be Crohn's disease, specific ulcerative colitis. If the blood comes from the upper parts of the large intestine, the blood is usually mixed. If it is released after defecation, then it is more like a disease of the terminal part of the colon.
Ekaterina Kryukova: The third and fourth stages are already a more difficult situation, when the nodes appear?
Rustam Abdullaev: The nodes begin to fall out already at the second stage, but the patient may not feel this. They fall out and immediately straighten themselves. It is unhygienic for a patient to climb and see whether something falls out or does not fall out, he does not feel it. The second stage may not lead to a proctologist. Many people may also skip the second stage.
The nodes begin to fall out already in the second stage, but the patient may not feel this. They fall out and straighten themselves right away.
Ekaterina Kryukova: Severe itching in the anal ring is already the third stage, when it hurts to sit.
Rustam Abdullaev: Itching can be caused by hemorrhoids, fissures, fistula, and there may also be problems with the upper gastrointestinal tract. These are problems with the release of bile or dysbacteriosis, errors in diet. There is such a disease as idiopathic anal itching, when it occurs without any organic pathology. We make this diagnosis extremely rarely, we practically never make it, because we still find out the cause and get rid of it. In the third stage, patients feel that the nodes have fallen out and have to be reset.
Ekaterina Kryukova: It’s hard not to notice here.
Rustam Abdullaev: Yes, they go into the bath, direct the shower and slowly tuck in these knots. It's hard not to notice here. Stage 4 is when the nodes have fallen out and can no longer be set. This is the last stage of hemorrhoids; it cannot be treated with any ointments or suppositories. We can say that this cannot be treated with minimally invasive methods either.
Ekaterina Kryukova: Will we be able to keep the disease in its early stages and it will not progress?
Rustam Abdullaev: It might be possible to hold it for some time.
Ekaterina Kryukova: What will influence? Maybe it's a hereditary venous system?
Rustam Abdullaev: Predisposition too.
Ekaterina Kryukova: Nutrition again...
Rustam Abdullaev: This is spicy, highly salted food, smoked foods, and a high meat content.
Ekaterina Kryukova: Carbonated drinks too?
Rustam Abdullaev: Carbonated drinks are not so important.
Ekaterina Kryukova: Alcohol?
Rustam Abdullaev: Alcohol first of all.
Ekaterina Kryukova: How does it directly influence this?
Rustam Abdullaev: Alcohol has a fairly strong effect on blood vessels, including the venous system. It expands, then narrows, increasing the disruption of venous outflow.
Ekaterina Kryukova: We are left with this venous nodule dangling like an earring...
Rustam Abdullaev: There is more than one venous node.
Ekaterina Kryukova: Relatively speaking.
Rustam Abdullaev: There are only 3 hemorrhoidal nodes, it is rare that there is an additional node.
Ekaterina Kryukova: Let's talk about treatment, from the lightest to heavy artillery. I read that you can use herbal medicine and physiotherapeutic methods. Are they also pointless or for follow-up treatment?
Rustam Abdullaev: Pointless treatment in general, I don’t even consider such moments. Pathologies when the patient cannot undergo radical surgery, for example, if he flies away on a business trip or trip, his hemorrhoids have worsened, but the inflammation needs to be relieved. And when he arrives, he will come for a second examination, and we will decide on the methodology. In some cases, we can prescribe conservative treatment, which will not give as much progress, or will relieve existing inflammation.
Ekaterina Kryukova: What easy techniques exist?
Rustam Abdullaev: The easiest methods are minimally invasive, that is, minimal intervention. The easiest method is sclerotherapy. This is an injection of a drug, a sclerosant, which glues the vascular tissue together. To put it simply, the vascular tissue sticks together, a slight inflammation occurs inside the vessel, and due to this inflammation, the nodes collapse, stick together, and turn into a small scar. Few doctors know this technique, and often have to be repeated several times. This may not depend on the doctor’s experience. The point is that you need to get into the vascular sac quite accurately and inject the drug there.
Ekaterina Kryukova: How many such injections are required?
Rustam Abdullaev: As a rule, one, 3 knots.
Ekaterina Kryukova: And does the treatment of hemorrhoids end?
Rustam Abdullaev: For a while. The second disadvantage is that there is a risk of relapse.
Ekaterina Kryukova: Approximately after how long should a person repeat this procedure?
Rustam Abdullaev: Enough for several years. It depends on the stage.
Ekaterina Kryukova: We are now taking the first and second stages.
Rustam Abdullaev: At the first stage, I usually do sclerotherapy. The result is quite good.
Ekaterina Kryukova: Are there any side effects? Is it painful or expensive?
Rustam Abdullaev: This is if you do it with your left foot.
Ekaterina Kryukova: Is anesthesia required?
Rustam Abdullaev: We now use intravenous sedation everywhere, this is not anesthesia, but drug-induced sleep. The most convenient for the patient, because local anesthesia is very painful. This is an area in which there are a lot of pain receptors, let's call it shockogenic. Even a minor wound or intervention causes severe pain. Therefore, we use intravenous sedation and local anesthesia. This is a five-minute procedure, then the patient lies for half an hour, we give him tea or coffee, and he goes home.
Ekaterina Kryukova: Do the protruding nodes that are present at the second stage go away and fold up?
Rustam Abdullaev: I won’t say that they disappear completely, they subside and a small scar forms. The most important thing is that the blood that enters the nodes has nowhere to go, nothing to fill.
Ekaterina Kryukova: Accordingly, there is nothing to inflame.
Rustam Abdullaev: Absolutely right. The method is not the most reliable, but if I do sclerotherapy, I don’t worry about the patient in terms of postoperative complications.
Ekaterina Kryukova: It’s quite predictable here.
Rustam Abdullaev: Yes, if you use the right concentration of the drug and the right dose. It’s very important here, because I’ve come across many cases where, let’s say, they shot a sparrow from a cannon. They injected a large amount of sclerosant, and necrosis occurred. There is a task, a protocol, a standard according to which more can be entered; this does not need to be exceeded. There is extensive experience in the use of sclerosants, and it is necessary to use those protocols that were drawn up and invented long before their use by inexperienced specialists.
Ekaterina Kryukova: In your opinion, is this the best choice for the first and second stages?
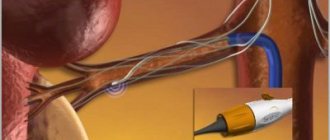
Rustam Abdullaev: Yes, this is for the first stage. The method of disarterization of hemorrhoids is used, an operation without a single incision. We have special equipment, we find the hemorrhoidal artery, which supplies the hemorrhoids. The device is an anoscope with a window and a sensor; when we begin to operate, it shows the artery itself, its depth, the diameter of the arteries, and the blood flow. We find this artery, which fills the node with blood, stitch it and bandage it. But no cuts are made.
Ekaterina Kryukova: Are we getting rid of the knot?
Rustam Abdullaev: In this case, the node does not die, it also subsides and ceases to be supplied with blood. This is a more reliable method than sclerotherapy. There are combined methods when we use both disarterization and sclerotherapy. We stitch and ligate the artery and inject a sclerosant into the base of the node. There are cases when the hemorrhoidal node is supplied not only by the large arteries that we see with the help of this device. There are small vessels that after some time, this can be several months, years, take on the function of large vessels. They expand to the same extent as large vessels. This process is called revascularization. There are indirect signs that the node is supplied with blood not by one artery, but by several, in this case we also introduce sclerosants.
Ekaterina Kryukova: In these small vessels? Tell me, are we actually blocking the movement of blood in the area of the hemorrhoid?
Rustam Abdullaev: Yes.
Ekaterina Kryukova: How is traffic blocked on the road?
Rustam Abdullaev: Absolutely right.
Ekaterina Kryukova: Isn’t it harmful? Are we artificially creating a dead end?
Rustam Abdullaev: No, this is a very physiological operation. At the very beginning of the conversation we said that these are rudimentary formations. Therefore, the fact that we block the blood flow, small vessels, capillaries remain, they do not allow the tissues to die, they remain in place. The nodes collapse, but no necrosis occurs.
Ekaterina Kryukova: Complication after?
Rustam Abdullaev: There is only one complication, in the early postoperative period for 3 weeks, if the patient does not follow our recommendations. For a month you cannot lift weights, you cannot visit baths, saunas, you cannot drink alcohol and observe sexual rest. It is very important. If the patient violates one of the four restrictions, then those ligatures, those sutures that we put on the arteries, can fly off, and then bleeding opens. I operated on about 2,500 patients, and I had about 20 such cases.
For a month after the operation, you should not lift weights, visit baths, saunas, drink alcohol, or maintain sexual rest.
Ekaterina Kryukova: Do you have difficulty going to the toilet?
Rustam Abdullaev: After this technique there are no difficulties.
Ekaterina Kryukova: Can’t we remove these stitches?
Rustam Abdullaev: No, everything is safe there. If you follow all these recommendations, then there will be no bleeding. The technique has been used for a long time and has been tested. The mucous membrane stretches, it is elastic, and in this regard there is no risk of bleeding.
Ekaterina Kryukova: As for the more advanced stages of the disease, do we resort to general surgery?
Rustam Abdullaev: At the 3rd stage, we do not use, at least in my practice, such a technique. I know all the techniques for hemorrhoid surgery...
Ekaterina Kryukova: What is called major surgery.
Rustam Abdullaev: We can combine. If there is an external component, that is, external hemorrhoids that are large enough, they may be supplied by separate arteries that we cannot ligate with ultrasound. In this case, we perform disarterization and excise the external nodes. This still applies to surgery: either with a scalpel, or radio wave, or electrocoagulation.
Ekaterina Kryukova: There is a classic Milligan-Morgan operation, there is also a Whitehead one...
Rustam Abdullaev: The second operation has long been forgotten. We do Milligan-Morgan at stage 4, and we do it quite often. It consists in the fact that the nodes are completely cut off. A clamp is applied to the vascular pedicle of the artery, about which we talked a lot today, and a second clamp is applied opposite it, and the nodes are completely cut off along the clamps and sutured. This is a reliable way to get rid of it, but the downside is the pain that occurs after surgery.
Ekaterina Kryukova: That is, during defecation.
Rustam Abdullaev: The first days it hurts even at rest.
Ekaterina Kryukova: And constant bleeding, the risk of infection...
Rustam Abdullaev: There are no risks of infection, because the intestine is a fairly resistant bacterium. There, the body has calculated everything, it happens extremely rarely when an infection gets somewhere between the seams, a small paraproctitis may occur, but this happens extremely rarely.
Ekaterina Kryukova: Is the recovery period painful and unpleasant?
Rustam Abdullaev: It usually hurts for 7-8 days, but it heals completely in a month.
Ekaterina Kryukova: And hemorrhoids do not return after such an operation?
Rustam Abdullaev: If you do sclerotherapy, then there is a risk of relapse, no more than 10%. If you do disarterization of hemorrhoids under Doppler control, then the risk of relapse is about 1.5%. After Milligan-Morgan, even less.
If you do sclerotherapy, the risk of relapse is no more than 10%
Ekaterina Kryukova: In principle, we have no problems with the treatment of hemorrhoids. Why do people suffer so much, why do they search so much for the right doctor, the right medicine?
Rustam Abdullaev: Firstly, people are embarrassed, and secondly, they are very afraid, there are a lot of reviews and all sorts of scarecrows written on the Internet. I specifically sat down and read what my patients were afraid of. They are afraid of a very strong pain syndrome that takes six months to heal, in fact, there is no such thing. I haven't seen anything that takes six months to heal.
Ekaterina Kryukova: Could there be long-term consequences of the operation?
Rustam Abdullaev: It happens that under Milligan-Morgan a problem can be solved.
Ekaterina Kryukova: Proficiency in the anal canal does not decrease?
Rustam Abdullaev: Insufficiency does not happen after hemorrhoid surgery, because we don’t touch the muscles at all, we don’t touch them.
Ekaterina Kryukova: Does the functional side never suffer?
Rustam Abdullaev: Absolutely. Insufficiency occurs only after certain diseases, acute paraproctitis. There are fistulas, paraproctitis, in some cases we even warn patients that they may have to be patient for six months. But this is not for hemorrhoids. This is after excision of extrasphincteric fistulas.
Ekaterina Kryukova: When receiving a patient at the initial appointment, we do a colonoscopy, anoscopy and try to look at the entire clinical picture. If we find accompanying polyps, do you operate on two problems in one?
Rustam Abdullaev: Yes, if it is a visually benign polyp, then it is immediately trimmed and sent for histology. If there is a suspicion that it is malignant, then a biopsy is taken, in this case we do not operate on hemorrhoids, we wait for histology. Colonoscopy is performed by endoscopists, that is, we do not perform colonoscopy. These are different specialists, but we work very closely. When my patients undergo a colonoscopy, I always go in before the operation to see how everything is happening there, whether there are any problems, so that I can immediately solve them on the spot. If the polyps are benign, we can immediately excise them and send them for histology, and we will take them straight away for surgery.
Ekaterina Kryukova: You correctly noted that the topic of diseases of the rectum, hemorrhoids, all this proctology is taboo in our country. I think a person who came to an appointment one day would be glad to get rid of everything at once. I would like to discuss such possibilities.
Rustam Abdullaev: We try to get rid of everything right away. By the way, you are talking about the taboo topic of proctology. Indeed, this is so, patients for the first time, especially the older generation, are very embarrassed by this problem and walk until they feel the urge, and they already come to give up: do what you want, operate, save me from this. Then they start sharing with relatives or colleagues, and it turns out that everyone they know has this problem. And they are operated on by me through word of mouth, 30 percent are patients who came through word of mouth.
Ekaterina Kryukova: Do you have an idea of how this happens in general, perhaps at the level of state medicine? What are they prescribed for us, do they operate on hemorrhoids? Or do ordinary, district proctologists tend to prescribe medications?
Rustam Abdullaev: You touched on a very relevant topic. The Russian school of colorectal surgery is very strong. At one time there was an academician named Ryzhikh who organized and built a coloproctology center. Coloproctology separated from general surgery and began to deal only with the colon. But, unfortunately, patients come to me from district clinics. They do not perform such operations on an outpatient basis.
Ekaterina Kryukova: Sclerotherapy, disarterization..
Rustam Abdullaev: As a rule, they don’t do anything at all. Maybe they do it somewhere, but they don’t get to me.
Ekaterina Kryukova: I thank you, this was the opinion of Rustam Abdullaev, coloproctologist, surgeon at the MedicCity clinic. We talked about hemorrhoids and how they can be successfully treated. Once and for all. I'm Ekaterina Kryukova, this was an “Online reception”. Thank you, stay healthy.
Effective treatment for hemorrhoids
If symptoms are not expressed or an exacerbation occurs for the first time, a competent doctor-proctologist will advise conservative measures, which will include:
- treatment of hemorrhoids with medication. Using a local set of ointments, suppositories, baths;
- it is necessary to normalize the “stool” - sufficient fiber consumption (vegetables, fruits, cereals), sufficient water consumption up to 1.5 -2.0 liters, activation of the motor mode (walking, playing sports);
- refusal of dry toilet paper in the anal area and use of warm water or a shower after defecation;
- They recommend wheat bran, seaweed and flaxseed in their natural form, or in the form of pharmaceuticals, seeds and psyllium husks, which have a high water-holding capacity, and this allows you to avoid straining during bowel movements.
In case of chronic recurrent course of the disease with 1 - 2 degrees of internal hemorrhoids, it is possible to apply latex rings to hemorrhoids:
The procedure is performed quickly and almost painlessly: a latex ring is applied to the hemorrhoidal nodes, which leads to disruption of the blood supply and “drying out” of the node, and in 4-5 days it “disappears” on its own. During one procedure, you can apply 1 - 2 rings. Sometimes 3 to 5 procedures may be required. Possible complications: bruising and pain (usually do not require additional interventions).
Minimally invasive procedures include:
- infrared coagulation (laser treatment of hemorrhoids);
- radiofrequency coagulation;
- cryo-treatment of hemorrhoidal venous plexuses.
All of them are aimed at eliminating the blood supply to the hemorrhoidal plexuses and reducing hemorrhoids.
How long does healing take? When can you lead your normal life?
Healing after radical removal of hemorrhoids lasts, on average, 35 days. If more than 60 days have passed and the wound has not healed, you need to figure out what the reason is. For several months after surgery, scar tissue continues to form. At this time, the patient may be bothered by various unpleasant sensations: numbness, tingling, twitching. If the stool is too dense, the patient may feel discomfort, burning, and notice traces of blood in the stool.
Can the nodes appear again after surgery, for example, after a year or after 5 years? Statistics say that after radical surgery, relapses occur in 4% of cases. Repeated hemorrhoids are caused by the same factors that caused them the first time. It is necessary to give up a sedentary lifestyle, avoid constipation, increased intra-abdominal pressure, and avoid excessive physical exertion.
If you still have questions, you can ask your coloproctologist online in the Doctis app.
Treatment of hemorrhoids at the Medical Plaza MC clinic
Treatment of hemorrhoids at the Medical Plaza medical center is carried out mainly using the radiofrequency method, which has proven its effectiveness. This method can also be used to treat bleeding hemorrhoids. The procedure is performed under local or spinal anesthesia, lasts up to 20 – 30 minutes and is painless. Observation for up to 2 hours after surgery is sufficient and the patient returns to his usual lifestyle.
For stages 3-4 of internal hemorrhoids, hemorrhoidectomy is performed under spinal anesthesia, which requires the patient to stay in the clinic for one day. During the recovery period, analgesics and suppositories may be required. The standard surgical technique has proven its effectiveness over many years of use.
And finally, for advanced forms of hemorrhoids with prolapse of nodes and rectal mucosa, there is an innovative hardware treatment method (Longo's operation), when a special stapler restores the anatomy of the anal canal while suturing the vessels supplying the hemorrhoidal plexuses. Pain after surgery is minimal, the recovery period is shorter than with standard surgery, and most importantly, the risk of complications is minimized.
It should be noted that only after an examination can a doctor recommend a method that is suitable for your situation.
What complications can arise after radical surgery?
During healing, early complications often arise such as:
- Urinary dysfunction. The operation does not injure the urinary tract; the disturbances are reflexive in nature and are associated with pain. Such complications are more common in men with prostate diseases.
- Bleeding. If the postoperative regimen is not followed, dense stools and constipation may cause injury to the wounds in the anal canal.
- Purulent-inflammatory processes. They occur when defecation is impaired, wounds become infected with pathogenic microorganisms, or local immunity decreases. Abscesses may appear - cavities with purulent contents or rectal fistulas.
Late postoperative complications can develop if the operation is performed incorrectly, or if the coloproctologist surgeon does not conduct regular examinations during the postoperative period, if the patient does not follow the doctor’s recommendations. Among these complications:
- Narrowing (stricture) of the anus. The complication occurs in 2% of cases. To correct a narrowing of the anus, plastic surgery may be required, often much more complex than surgery to remove hemorrhoids.
- Insufficiency of the anal sphincter. This dangerous complication can develop both due to damage to the obturator apparatus of the rectum during surgery, and scar deformation of the anus (the sphincter is intact, but postoperative scars do not allow it to ensure a tight closure of the anus).
- Long-term non-healing wounds are a very common complication, observed in 20−30% of cases, most often associated with infection of wounds by pathogenic and opportunistic flora (chlamydia, trichomonas). A long-term non-healing wound sometimes brings more suffering to the patient than the hemorrhoids themselves.
Ointments Bezornil, Aurobin and Levomekol ®
An equally effective method to help treat pathology is the use of ointments or creams, for example Bezornil. The product for local therapy contains musk of artificial origin (muscone), bezoar, calamine, pearls and amber. The components provide antimicrobial, astringent and drying effects. You need to use ointment for hemorrhoids at least 2 times a day, and preferably after each bowel movement.
Aurobin for hemorrhoids. The product contains lidocaine, D-panthenol (regenerating), triclosan (antiseptic), prednisolone (potent anti-inflammatory effect). Used for hemorrhoids 2 times a day for a course of no more than 5-6 days.
Levomekol for hemorrhoids. One of the safest means for external drug therapy, approved for use even in pregnant and lactating women. The main active components of Levomekol are methyluracil, which has regenerative and moderate immunostimulating effects (due to activation of interferon synthesis), and chloramphenicol, an antimicrobial substance. On average, you need to be treated with Levomekol for 9-10 days, applying the ointment 2-3 times a day.