Congenital heart defects (CHD) are developmental anomalies that lead to disruption of the morphological structure of the heart, including the valve apparatus and great vessels.
CHDs occur during the period of intrauterine development (usually at 2-8 weeks) as a result of disruption of embryogenesis processes. These anomalies can occur either alone or in combination with each other.
The overall prevalence of this group of diseases is up to 5-8 cases per 1000 births. Congenital defects can be associated with chromosomal abnormalities, however, non-chromosomal congenital heart defects are often diagnosed.
The overall incidence of non-chromosomal congenital heart disease is up to 7 cases per 1000 births, of which up to 3.5% are perinatal losses, 20% are diagnosed prenatally, 5.6% of pregnancies are terminated due to a detected fetal anomaly. Complex non-chromosomal heart defects are less common, approximately 2 cases per 1000 births. The outcome in 8% of cases is perinatal death, 40% are diagnosed in utero, and 14% cause termination of pregnancy.
general description
Congenital heart defects (heart defects) are an abnormal structure of the heart chambers, large vessels or valves (combinations are not uncommon) due to genetic predisposition, intrauterine development disorders, infectious, autoimmune, metabolic and other diseases, injuries received by the mother during pregnancy.
Valve lesions can be congenital (due to disorders of intrauterine development) or acquired, that is, occurring during life under the influence of diseases, infections or injuries. In most cases, complex congenital defects require surgical correction in both children and adults.
Methods for diagnosing congenital heart disease
Diagnosis of congenital heart disease is based on collecting medical history data (presence of developmental defects, including congenital heart defects, genetic diseases in close relatives; information about pregnancy and the presence of etiological factors in parents).
When collecting complaints, attention is paid to the child’s developmental delay, poor weight gain, poor appetite, sluggish sucking from the breast or bottle, breast refusal, cyanosis, and frequent respiratory infections.
Physical examination
During a physical examination, pay attention to the color of the skin, determine pulse and blood pressure (on the right arm and either leg), perform auscultation of the heart and lungs, pay attention to the presence of peripheral edema, perform pulse oximetry, and determine diuresis.
Instrumental diagnostics
However, the leading role in the diagnosis and confirmation, differential diagnosis of congenital heart disease is played by instrumental examination methods: x-ray examination of the chest organs, electrocardiography, echocardiography, MRI, CT, catheterization of the cardiac cavities.
Sign up for diagnostics To accurately diagnose the disease, make an appointment with specialists from the Family Doctor network.
What are the types of congenital heart defects?
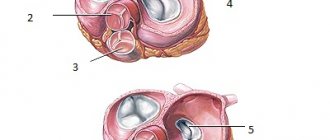
- pulmonary valve stenosis
- stenosis of the aortic valve, aortic orifice, subvalvular stenosis;
- mitral stenosis - narrowing of the bicuspid atrioventricular valve;
- Mitral valve insufficiency - incomplete closure of the bicuspid atrioventricular valve;
- Mitral valve prolapse - excessive length of one or two valve leaflets;
- aortic valve insufficiency;
- tricuspid stenosis;
- triscupidal insufficiency;
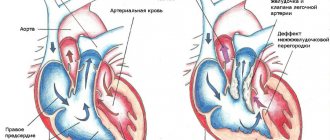
- defects of the interatrial and interventricular septum;
- anomalies in the development of heart cavities: Ebstein's anomaly, single atrium, single ventricle;
- transposition of large vessels - aorta and pulmonary artery;
- tetralogy of Fallot;
- open arterial (Botallov) duct;
- coarctation of the aorta;
- The most common congenital heart defect is an abnormal communication between the atria—atrial septal defect.
Diagnosis of congenital heart disease in newborns
Naturally, the earlier a congenital heart defect in newborns is detected and timely treatment begins, the more favorable the prognosis. However, due to the absence of clearly defined symptoms and, accordingly, no treatment at all, there are cases of death among children under 1 year of age (occasionally even older).
Usually, during preventive examinations, the doctor must listen to the baby’s heart. If murmurs are heard there, this is a reason for a detailed examination of the heart (although not necessarily a symptom of congenital heart disease).
For this purpose, parents and children are referred to specialists with a narrower profile - a cardiologist and a cardiac surgeon.
If you suspect a heart defect, the baby’s parents do not need to immediately turn to Internet search engines with the request “congenital heart defect surgery.” Not all defects require radical surgical intervention. And the main thing is to first establish the correct diagnosis.
Changes characteristic of congenital heart disease in a newborn are revealed by the following research methods:
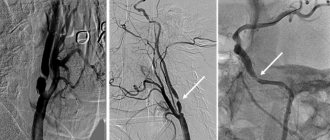
- X-ray of the chest (as well as ventriculography - x-ray with contrast injection).
- Echocardiography (using ultrasound to examine the condition of the heart muscle, valves, blood flow in the heart cavities).
- Electrocardiogram – ECG (or methods based on it: stress ECG (treadmill test, bicycle ergometry), ECG Holter monitoring).
If the above examination methods reveal the presence of a serious disease - congenital heart disease, then further diagnostics are carried out in the cardiac surgery department on an inpatient basis. Surgeons, if necessary, conduct examinations using procedures such as angiocardiography and probing of the heart chambers.
Modern high-tech medical equipment allows you to conduct a full comprehensive examination of the heart and blood vessels in order to establish the most accurate diagnosis and choose the necessary treatment tactics.
Diagnosis and treatment of heart disease
Cardiac surgeons can recognize and eliminate the defect in a timely manner. In most cases, x-ray surgeons close the defect using catheter technology without resorting to an incision.
- A defect may appear between the ventricles of the heart - a ventricular septal defect.
- Often the defects are combined with anomalies of the valvular apparatus of the heart or large vessels.
The valvular apparatus of the heart consists of four valves: mitral (bicuspid), tricuspid (three-cuspid), aortic and pulmonary valve. The functioning of the heart depends on the coordinated and correct functioning of these structures.There are two main types of valve disease: valve insufficiency and stenosis.
When there is insufficiency, the valve leaflets do not close completely, leaving a gap through which blood is thrown in the opposite direction to the normal direction. And with stenosis, the valves do not open completely, preventing normal blood flow. Isolated lesions of the heart valves are relatively rare; they are very often observed in other congenital heart defects. For example, a bicuspid acortical valve is often found in people with a patent ductus arteriosus. With this defect, part of the blood (rich in oxygen) from the aorta, which is not closed after the birth of the child, enters the pulmonary artery, causing an overload of the right side of the heart. In children and adolescents, such an abnormal message is most often eliminated without surgery, by installing a “plug” through the catheter.
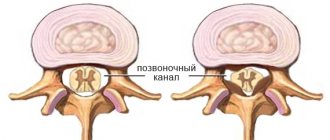
- Another congenital malformation is stenosis of the descending aorta.
In the thoracic segment, the aorta is attached to the posterior wall, closer to the spine. At this point, the aorta is sometimes significantly narrowed, and the internal organs do not receive enough arterial blood. Previously, this condition, called coarctation of the aorta, could only be corrected with surgery. But today, in most cases, narrowing during coractation of the aorta is eliminated by balloon dilation and installation of a stent frame. It should be emphasized that if valve stenosis is an isolated lesion, it is often eliminated by balloon expansion, in a minimally traumatic way.
No more sentence! Congenital heart defects in children: identify and treat
Perhaps there will always be diseases about the methods of treatment of which one could say something like “If only such diagnosis and treatment existed... years ago.”
This phrase is also true in relation to our topic today. With Candidate of Medical Sciences, pediatric cardiologist at Clinic Expert Smolensk Tatyana Mikhailovna Frolova, we are talking about congenital heart defects.
— Tatyana Mikhailovna, what is congenital heart disease? Is this a separate disease or a group of diseases?
This is a whole group of pathologies - congenital defects in the structure of the heart and large vessels, as well as anomalies in the location of the heart in the chest. These defects disrupt blood flow inside the heart and in large vessels and can lead to the development of heart failure, disability, and in some cases, the death of the child.
Today there are more than 35 types of congenital heart defects
Today there are more than 35 types of such defects.
— Do babies with congenital heart disease always look different from their healthy peers? Or can a heart defect in a child be asymptomatic?
The latter is true. Along with very severe defects, there are also those that are not accompanied by obvious clinical manifestations. Such children may be no different from their peers. It has become possible to identify these defects thanks to the improvement of methods for studying the cardiovascular system. They are often diagnosed accidentally.
— How is it usually discovered that a child has a heart defect?
Modern ultrasound machines make it possible to detect or suspect the presence of fetal heart defects even in the prenatal period.
After birth, a child also undergoes an ultrasound examination of the heart in the first year of life.
“An ultrasound is definitely not enough. The examination must be comprehensive." Quote from the material “Ultrasound of the heart: when is it prescribed and what will it show?”
It is possible that a defect may be accidentally discovered during examination for other reasons (medical examinations, obtaining certificates for sports activities, etc.).
And, finally, situations when a child develops some symptoms or changes are detected on the ECG, which becomes a reason to deepen the diagnostic search and conduct echocardiography.
“What are the types of heart murmurs? Where do they come from? And what to do if such noise is detected? Quote from the material “Heart murmurs in a child: looking for reasons”
— Should a cardiac examination of a baby be carried out only when indicated, or should all newborns undergo special diagnostics to exclude congenital heart defects and other cardiovascular pathologies?
According to the order of the Ministry of Health, ultrasound screening (echocardiography) is mandatory at the end of the neonatal period (the first month of extrauterine life), i.e. when the baby is one month old, during a routine medical examination. All children under one year of age must undergo such a study along with an ECG.
Of course, if a child has any manifestations of trouble, they do not wait for any special time, but consult a doctor immediately.
— How many children in Russia and the world are born with congenital heart defects?
According to statistics, congenital heart defects are considered a fairly common pathology. Their frequency in our country is 8 children per 1000, or 1 per 125 live births. The true incidence is higher if we take into account cases of early stillbirths and cases of spontaneous abortions.
In European countries this figure ranges from 3 to 8 per 1000 children. The highest frequency is in third world countries, in Asian countries.
- Why is a child’s heart so vulnerable? Are heredity and ecology to blame, or are there other reasons for the development of congenital heart defects in babies?
Approximately 90% of heart defects are multifactorial in nature. In other words, the combined influence of both hereditary and environmental factors plays a role in their occurrence.
8% of defects are caused by chromosome abnormalities and “breakdowns” of individual genes.
In our country, 8 children out of 1000 are born with congenital heart defects
2% is due solely to environmental factors that increase the risk of congenital heart defects. These may be physical, chemical factors, hazardous production, or unfavorable environmental conditions.
In addition, the formation of the defect can be facilitated by maternal diseases (in particular, endocrine; infectious pathologies during pregnancy), taking certain medications, smoking, and drinking alcohol by the mother.
— Modern diagnostics make it possible to identify congenital heart defects at the stage of intrauterine development?
Yes, but not in all cases.
— Before birth, can any heart defects in the fetus be detected with 100% accuracy, or is the development of perinatal diagnostics imperfect today?
As I said earlier, reliable diagnosis is not always possible. The success of detecting a defect is influenced by the position of the fetus, its mobility during the examination, the qualifications and experience of the doctor, the class of the apparatus for performing ultrasound, and the severity of circulatory disorders.
Some anatomical features of the heart, such as a patent ductus arteriosus, are normal in the prenatal period and become a defect only if they persist for a long time after birth. In these cases, dynamic monitoring of the child comes first.
Why are pregnant women prescribed MRI? Read here
— Tatyana Mikhailovna, if a fetus is diagnosed with a heart defect, is this an indication for termination of pregnancy or is the decision made individually in each case?
Today this is not a reason to terminate a pregnancy. In Russia, individual operations for intrauterine correction of heart defects have already begun. If there are no indications for surgical treatment during pregnancy, then after the birth of the child and consultation with a cardiac surgeon, the necessary operation is performed either immediately or later.
— Previously, the diagnosis of “congenital heart disease” almost always sounded like a death sentence. Has the situation changed now?
Over the past 10-15 years - dramatically. What has changed? The detection of defects in the prenatal period has improved significantly. Defects began to be diagnosed that do not require urgent surgical intervention and that can be eliminated on their own as the child grows older. If there is a question about surgery, then, if necessary, it can be performed even on the first day after the birth of the child.
“Holter monitoring is also used to examine children.” Quote from the material “Holter (24-hour) ECG monitoring - complete instructions for the patient”
— If a baby is diagnosed with a heart defect after birth, is this always an indication for surgery?
No. All heart defects require dynamic monitoring, since their spontaneous closure is possible, reducing the severity of circulatory disorders, as a result of which there is no need for surgical treatment. With some defects, the child can even engage in certain sports if there are no significant circulatory disorders.
— If necessary, can surgeries in Smolensk help a baby with a congenital heart defect, or are such children sent to large Russian cardiology centers?
Heart surgeries are high-tech and highly specialized medical care. They are performed only in large specialized clinics.
If necessary, the operation can be performed even on the first day after the birth of the child.
Smolensk patients can undergo surgery in Moscow or St. Petersburg, if we talk about regional proximity. In our city, unfortunately, such operations are not carried out.
— It is generally accepted that prevention can save you from many health problems. Is it possible to reduce the risk of having a child with a heart defect?
Yes. It is extremely important to remember the periods of heart development here. Its formation begins at the end of the 2nd week of pregnancy. By the 4th week, a two-chamber heart is formed, and by the 6th week the chambers separate to form a four-chambered heart.
Just thinking about these numbers is enough. Does every woman at two weeks (and even later) know about her pregnancy? No, whereas at this time the heart is laid and formed. If during this period there are unfavorable factors that we talked about earlier, the risk of developing a defect increases. Therefore, the most important prevention is planning and preparation for pregnancy. A woman must be healthy, she needs to lead an appropriate lifestyle.
Pregnant women need to undergo regular screenings, during which some abnormalities in the development of the heart in the fetus may be detected. When they are detected, the question of the method of delivery is decided.
Other materials on topics:
What should a child's blood pressure be?
Are unvaccinated children the healthiest?
Often – how much? A child who is often ill at a pediatrician's appointment
For reference:
Frolova Tatyana Mikhailovna
Graduate of the pediatric faculty of the Orenburg State Medical Academy in 1997.
From 1997 to 1998 she completed an internship in the specialty “Pediatrics”.
In 2014, she underwent professional retraining in pediatric cardiology, and in 2021 - in functional diagnostics. Candidate of Medical Sciences.
Currently, he is a pediatric cardiologist and functional diagnostics doctor at Clinic Expert, Smolensk. Receives at the address: st. 8 March, no. 20.
How do heart valve diseases manifest?
Most often, patient complaints are nonspecific: shortness of breath, rapid pulse, arrhythmia, fatigue, cyanosis, dizziness.
The severity and nature of symptoms depend on the location of the affected valve. With valve defects of the left half of the heart (mitral and aortic), the lungs are primarily affected, because Blood stagnates in their vessels, which manifests itself as shortness of breath. There are also signs of insufficient blood supply to all organs and systems, primarily the brain and the heart itself. Dizziness, fainting, and angina occur. If the functioning of the valves of the right half of the heart (tricuspid and pulmonary valves) is disrupted, blood stagnates in the vessels of the systemic circulation, i.e. all organs except the lungs are affected. Swelling of the legs and feet, ascites (fluid in the abdominal cavity), enlargement of the liver, etc. develop (LIVER INCREASES, ETC.).
Heart valve defects are dangerous due to their complications and impact on the body, so the main prevention of pathological conditions is regular examinations and treatment of diseases leading to the formation of valve defects.
Treatment for the diagnosis of congenital heart disease in newborns
Treatment methods depend on the type of heart defect:
- Minimally invasive procedures
- Radical surgery
- Heart transplant
- Drug therapy
- Long-term therapy
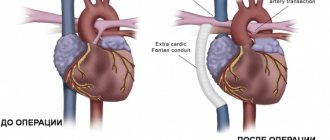
If the heart defects are not very serious, minimally invasive procedures can be used. Their essence is that a thin catheter is inserted into the heart through the femoral vein, and the necessary instruments are delivered to the defect inside the catheter.
The most radical but effective method of treating congenital heart disease is surgery. This is a traditional open intervention with opening of the chest and the heart itself. Most of these operations are performed using a heart-lung machine. After heart surgery, a child faces a long and difficult recovery period, but sometimes it is the only possible way to cure.
Heart transplantation is used in the most severe cases, in which traditional surgery is helpless in case of severe congenital heart disease.
Drug therapy is used mainly for auxiliary purposes, improving the functioning of the heart and blood flow.
Long-term therapy involves several consecutive operations on congenital heart disease.
Is a conscript accepted into the army if he has an open foramen ovale?
The likelihood of such a serious pathology as a patent oval window increases under the influence of the following factors:
- unfavorable environmental conditions;
- taking drugs belonging to the group of non-steroidal anti-inflammatory drugs during pregnancy;
- smoking;
- frequent consumption of alcoholic beverages during pregnancy;
- premature birth.
The clinical picture observed in the presence of an open oval window depends on the following individual characteristics:
- hole sizes;
- presence of blood flow disturbance.
If the hole size does not exceed 5 mm, characteristic clinical symptoms are usually absent. In the absence of blood flow disturbance, the young man is assigned category “B-4”.
A deferment from military service in the presence of an open oval window is not granted.
Diagnostics
At each appointment, the pediatrician conducts auscultation (listening with a phonendoscope) and examination of the chest to check the functioning of the child’s heart, even if the patient came in for ARVI. Pathological murmur is easily auscultated by a cardiologist. It indicates heart problems, even if the patient is not worried about anything or does not attach importance to some symptoms (in addition, children are sometimes afraid to report their problems and worries).
Basic diagnostic methods in cardiology:
- ECG (assessment of the conduction of electrical impulses through the heart muscle);
- Daily ECG monitoring;
- Ultrasound of the heart;
- Echo-CG (study of the morphology and functional state of the heart);
- Doppler echo-CG (study of blood flow in the chambers of the heart and great vessels);
- Plain radiography of the chest (determining the size and location of the cardiac shadow);
- Coronary angiography (study of coronary vessels);
- CT;
- MRI.
It is important to identify the disease in time: the earlier treatment is started, the better the effect. However, most violations can only be detected using special equipment. In addition, the baby is not able to voice complaints, so instrumental diagnostics in pediatrics cannot be avoided.
Military service and arrhythmia
A young man is taken into the army with arrhythmia if it takes the following varieties:
- tachycardia, accompanied by rapid heartbeat;
- bradycardia. With this type of arrhythmia, the heart rate slows down;
- extrasystole. With this pathology, single arrhythmic beats occur. With extrasystole, there is no change in heart rate.
If certain types of arrhythmia are present, the conscript receives the right to be assigned category “D”. These include:
- paroxysmal tachycardia. With this pathology, heart contractions increase sharply. Adverse symptoms such as weakness, fear of death, shortness of breath, and a feeling of pressure in the chest area may appear;
- presence of Adams-Stokes-Morgagni attacks. With this pathology, complications such as loss of consciousness or respiratory arrest may occur;
- weak sinus node syndrome;
- ventricular extrasystole.
Read more about whether people with tachycardia are accepted into the army.
Acquired heart defect
Up to 90% of acquired defects develop against the background of rheumatic diseases. Based on the state of general hemodynamics, compensated, subcompensated and decompensated defects are distinguished.
Valve defects cause increased load on the corresponding parts of the heart, myocardial hypertrophy and ultimately heart failure. The suitability of a conscript with an acquired heart defect is determined according to the functional class based on the document Schedule of Diseases.
The clinical picture of the disease depends on the affected valve or combination of affected valves. The patient complains of tachycardia, shortness of breath, edema and other signs characteristic of heart failure.
The main type of treatment for acquired defects is surgery.
Postpartum period in women with heart defects
The risk of thrombosis, bleeding and heart failure persists up to 5 days after birth, so during this period the woman is prescribed bed rest. From the 7-11th day, if the defect is of a rheumatic nature, the woman is prescribed a study to determine the activity of rheumatism; The activity of rheumatism is monitored during the year after childbirth.
Postpartum women with heart disease can be discharged from the maternity hospital no earlier than 2 weeks after birth in satisfactory condition under the supervision of a cardiologist at the place of residence.
If decompensation does not occur after childbirth and medications are not required, breastfeeding is preferable.
After the birth of a child, specialists must examine him for the presence of heart defects, since in children whose mothers had such problems, the risk of having them increases many times over.
Thus, timely diagnosis and proper treatment allow many women who were previously unable to have a child to experience this joy. And experts are always ready to help them with this.
How to identify a heart defect
The specialist begins determining the presence of a heart defect with a conversation with the patient, the purpose of which is to clarify the existing symptoms. The main signs of the disease include:
- decreased ability to work and rapid fatigue;
- chronic fatigue, fainting, which have been observed since childhood;
- pallor, cyanosis of the skin;
- swelling;
- unstable blood pressure (high or low);
- shortness of breath with little physical activity;
- decreased immunity, provoking the development of various immune pathologies.
With congenital heart disease, the clinical picture is observed from childhood. When compiling an anamnesis, previous diseases and diagnoses, as well as surgical interventions, are taken into account.
To identify heart pathology, it is mandatory to measure blood pressure, study the condition of the skin, and listen to the heart. If necessary, to confirm the preliminary diagnosis, the patient is prescribed instrumental examinations:
- Electrocardiography. The method is effective for identifying various cardiac pathologies. The method makes it possible to record electric fields that arise during myocardial oscillations, which makes it possible to record deviations in the functioning of the heart.
- X-ray. The method allows you to determine anomalous phenomena visually.
- Ultrasound of the heart. Used when necessary to monitor the patient's condition.
The results of the examination are entered into the medical history, which the patient, along with various certificates and a doctor’s opinion, provides to the military medical commission to obtain a deferment or exemption from service due to health reasons.
Mitral valve prolapse
In the presence of mitral valve disease (MVD) of the 1st degree, the characteristic symptoms of the disease are often absent. The patient's health remains satisfactory. The answer to the question of whether people with congenital mitral valve disease of the 1st degree are recruited into the army is positive. PMH of the first degree is not one of the diseases that exempts you from the army. At the same time, the accompanying documents indicate the relevant information about the presence of mitral valve disease in the young man.
Note! In the presence of grade 2 or 3 MVP, valve function noticeably deteriorates. Regurgitation may occur, which changes the direction of blood flow. This pathological condition can lead to serious health problems.
In the presence of mitral valve disease of 2 or 3 degrees, oxygen starvation may occur. It may be accompanied by the following adverse symptoms:
- feeling of fatigue;
- dizziness;
- cardiopalmus.
A young man who has been diagnosed with stage 2 or 3 mitral valve disease is in most cases assigned category “B”. This means that the young man is exempt from military service in peacetime. A young man is subject to conscription only in the event of general mobilization (during military operations).
Read more about whether people with mitral valve prolapse can be drafted into the army on our website.