What are varicose veins?
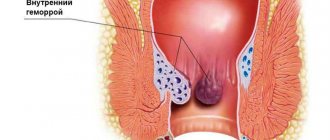
Varicose veins (in common parlance - varicose veins ) are overstretched, irregularly shaped, tortuous blood vessels that have lost their elasticity. They are increased in length and width and look like thick, convoluted blue strands that are visible under the skin. Veins become this way when the venous valves are missing or for some reason cannot perform their functions. If the valves do not work properly, blood flows through the veins in the opposite direction, downwards, accumulating in the lower sections of the veins and bursting their walls. As a result, the veins lose their natural shape, and a pathological chain of various complications begins.
Vessels: what you need to know?
22.10.2019
There are three main types of blood vessels in the human body: arteries , veins , and lymphatic vessels . They all look like a rubber pipe with many branches and different passages. pink arteries the veins are bluish and soft. Blood vessels are yellowish.
Story
Ancient anatomists connected arteries and veins with various organs. In the Middle Ages, scientists misunderstood the system of arteries ; they thought that they were not all connected to each other. This theory was refuted by the Italian physician Jacopo Berengario da Carpi at the end of the 15th century. He noticed that an artery is connected to every artery . In the 16th century, anatomists tried to answer the question of how blood gets from veins to arteries . This was clarified in the second half of the 17th century by William Harvey, who discovered blood circulation.
Under a magnifying glass
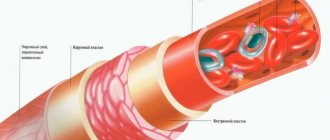
The wall of the vessel consists of three layers. Its inner part consists of a lining of flat cells (the so-called endothelium; the entire inner layer has other parts and is called intima). The middle layer consists of round and spirally oriented smooth muscle cells. The outer layer of the vessel is a compound that forms a flexible membrane (adventitia). The adventitia connects blood vessels and nerves to nourish and control vascular . Arteries have a thicker layer of muscle than veins . The capillary wall consists of a single layer of cells - the endothelium. In the veins, the endothelium forms a small pocket, a flap, in certain places, preventing blood flow. Blood vessels have a similar structure to veins .
Comparative anatomy of blood vessels
As is known, humans have a closed blood circulation. For example, mollusks, snails, arthropods and jellyfish have open blood circulation. Their “blood” or hemolymph, if present, is located directly between the organs of the body. Insects are less developed, they have only a simple tubular heart .
Anatomy
Blood vessels extend from the heart to all organs and cells. The aorta originates in the left ventricle, descends into the abdomen and flows into the pelvis, where it divides into two arteries that carry blood to the lower extremities. arteries (emanating from the aorta) also function blood to the head, upper limbs, all internal organs and skin. The arteries branch into smaller ones and eventually become capillaries. Arterial capillaries pass into venous capillaries, which converge further into veins . The superior vena cava carries blood to the heart from the lower extremities, abdomen and torso, and it also carries blood from the head and upper extremities. Blood vessels form blindly between cells flowing into stronger trunks and entering veins .
Functions
Blood vessels are used to transport blood in the body. A person has a so-called closed circulation. This means that blood flows only in blood vessels and does not accidentally “wash” certain organs. Arteries carry blood from the heart . Most of this blood is oxygenated, except for the blood that passes through the pulmonary artery from the right ventricle to the lungs . Veins carry blood to the heart . Except for the blood in the pulmonary veins , which is oxidized and flows into the left ventricle.
In the human body there are two circles of blood connected by the heart . The "small" or pulmonary circulation is where oxygenated blood is drawn through the pulmonary artery from the right ventricle into the lungs , where the pulmonary veins lead to the left ventricle. And the “large” circulation, where oxygenated blood from the left ventricle moves to the right atrium, and from there to other arteries and organs. There the blood loses oxygen and the veins return it to the heart . Blood vessels collect saliva in the intercellular spaces and transport it to the veins .
Published in Cardiology Premium Clinic
How common are varicose veins?
Varicose veins are one of the most common diseases of the vascular system. According to some statistical estimates, from varicose veins . The number of people who have varicose veins increases with age, and women are affected much more often than men. According to statistics, in the age group under 25 years only 8% of women suffer from varicose veins, and in the older age group - 55 years and older - 64% of women are affected by varicose veins.
How can you recognize varicose veins in yourself?
The most common sign of varicose veins is fatigue, dull pain, a feeling of heaviness and fullness in the legs after sitting or standing for a long time. Often these symptoms appear or worsen in the evening. However, it is usually impossible to determine exactly where it hurts. And if these unpleasant symptoms - fatigue, heaviness, pain - go away after resting with your legs elevated, then they are really caused by varicose veins (unless some other cause is reliably identified).
However, do not rush to blame everything on varicose veins, especially if there are no external signs in the form of dilated veins. Some other painful conditions may also exhibit the same symptoms.
Leg cramps
With varicose veins, painful nighttime cramps in the leg muscles can actually occur (in other words, “leg cramps”). Most often, cramps appear in the calf muscles and can sometimes be so painful that the patient wakes up. Moreover, night cramps usually occur after a hard day, when the patient had to stand or sit a lot.
Publications in the media
Resuscitation or intensive care is impossible without constant transfusion therapy and taking blood samples for laboratory tests, often emergency. Under these conditions, it is necessary to have a constantly functioning venous access, providing both the infusion of any solution with optimal speed and efficiency, as well as the possibility of laboratory diagnostics and monitoring. Central venous catheterization serves this purpose. In resuscitation practice, the subclavian vein, external and internal jugular veins are most often punctured and catheterized, less often - the femoral and even less often - the ulnar vein (peripheral veins collapse and become empty during hypovolemia, and therefore are poorly contoured).
• Subclavian vein •• Indications: shock of any etiology, because Due to anatomical features, this vein does not collapse during hypovolemia. In addition, when using the subclavian vein, good comfort is provided for the patient and the possibility of careful care even with a long stay of the catheter in the vein (for several months) •• Disadvantages of catheterization of the subclavian vein - a high risk of developing pneumothorax, the possibility of injury to the subclavian artery and difficulties when necessary to stop bleeding (impossibility of compression).
• External jugular vein •• Indications ••• Access to this vein is preferable in the elderly, it is well contoured even in obese patients ••• Less danger of developing pneumothorax ••• Its rapid effective compression is possible in case of hemorrhagic complications due to coagulation system disorders •• Inconveniences - the impossibility of its long-term use due to discomfort for the patient, difficulties in care, and relatively unreliable fixation.
• Internal jugular vein •• Characterized by rare complications, especially pneumothorax, good control in case of hemorrhagic complications, high rate of successful catheterizations even during cardiopulmonary resuscitation •• Disadvantages ••• Possibility of injury to the thoracic lymphatic duct or carotid artery during catheterization on the left •• •• The impossibility of its use in intracranial hypertension and during hemodialysis and tracheostomy ••• This vein can be collapsed with deep shock or hypovolemia.
Execution technique. The patient's position is lying on his back, the head end of the table is lowered, a cushion is placed under the patient's back, the patient's head is turned in the direction opposite to the puncture site. The patient's arm on the puncture side is brought to the body, sharply supinated, the assistant pulls it in the caudal direction. The patient may be positioned according to Trendelenburg. There are two operational approaches for puncture catheterization of the subclavian vein.
• Subclavian access •• A 0.5% procaine solution is injected intradermally with a syringe with a thin needle to create a “lemon peel” at a point located 1 cm below the clavicle on the line separating the middle and inner third of the clavicle. The needle is advanced medially towards the upper edge of the sternoclavicular joint, continuously applying procaine solution. The needle is passed under the collarbone and the rest of the procaine is injected there. The needle is removed •• Using a thick sharp needle, limiting the depth of its insertion with the index finger, the skin is pierced to a depth of 1–1.5 cm at the location of the “lemon peel”. The needle is removed •• A syringe with a capacity of 20 ml is filled up to half with 0.9% sodium chloride solution, and a not very sharp (to avoid puncture of the artery) needle 7–10 cm long with a bluntly beveled end is put on. The direction of the bevel should be marked on the cannula. When inserting the needle, its bevel should be oriented in the caudal-medial direction. The needle is inserted into a puncture previously made with a sharp needle (see above), and the depth of possible needle insertion should be limited to the index finger (no more than 2 cm). The needle is advanced medially towards the upper edge of the sternoclavicular joint, periodically pulling the plunger back, checking the flow of blood into the syringe. If unsuccessful, the needle is pushed back without removing it completely, and the attempt is repeated, changing the direction of advancement by several degrees. As soon as blood appears in the syringe, part of it is injected back into the vein and again sucked into the syringe, trying to obtain a reliable reverse blood flow. If a positive result is obtained, ask the patient to hold his breath and remove the syringe from the needle, squeezing its hole with a finger. •• A conductor is inserted into the needle with light screwing movements halfway; its length is slightly more than two times the length of the catheter. The patient is again asked to hold his breath, the guide is removed, closing the catheter hole with a finger, then a rubber stopper is put on the latter. After this, the patient is allowed to breathe. If the patient is unconscious, all manipulations associated with depressurization of the lumen of the needle or catheter located in the subclavian vein are performed during exhalation •• The catheter is connected to the infusion system and fixed to the skin with a single silk suture. Apply an aseptic dressing.
• Supraclavicular approach •• Position of the patient - as with subclavian access •• The doctor pierces the skin in the area of the angle formed by the lateral leg of the sternocleidomastoid muscle and the upper edge of the clavicle, moving 0.5 cm upward from the clavicle. After puncturing the skin, the needle is directed at an angle of 45° to the sagittal and 15° to the frontal plane of the clavicle and the vein is pierced. Further actions are the same as for infraclavicular access.
• After each infusion, 0.1 ml of heparin is injected into the catheter (the so-called “heparin lock”), so that the catheter can be used for several weeks without complications.
• If thrombosis, phlebitis or catheter sepsis is suspected, the catheter must be removed, followed by appropriate treatment measures.
Is varicose veins inherited?
It is now known that varicose veins are hereditary. Scientists even believe that they were able to isolate a separate gene responsible for the development of varicose veins. It is not yet clear whether this gene causes malformations of the venous valves or malformations of the vein walls themselves. But there is no doubt that these studies will help develop a gene therapy technique - perhaps the most promising way to prevent and treat varicose veins. Unfortunately, this is still a matter of the rather distant future, and gene therapy is not yet available to patients with varicose veins.
Central venous catheterization
Just about central venous catheterization.
Puncture and catheterization of veins, in particular central ones, are widespread manipulations in practical medicine. Experience shows that this manipulation is not safe enough. Therefore, knowledge of the topographic anatomy of the subclavian vein and the technique of performing this manipulation is extremely important.
In one year, more than 15 million central venous catheters are installed worldwide. Among the venous tributaries available for puncture, the subclavian vein is most often catheterized.
Historical reference.
The first puncture of the subclavian vein was performed in 1952 by Aubaniac. He described the technique of puncture from the subclavian approach. Wilson et al. in 1962, a subclavian approach was used to catheterize the subclavian vein, and through it, the superior vena cava. Since that time, percutaneous catheterization of the subclavian vein has become widely used for diagnostic studies and treatment. Yoffa introduced the supraclavicular approach into clinical practice in 1965 to insert a catheter into the central veins through the subclavian vein. Subsequently, various modifications of the supraclavicular and subclavian approaches were proposed in order to increase the likelihood of successful catheterization and reduce the risk of complications. Thus, the subclavian vein is currently considered a convenient vessel for central venous catheterization.
Puncture catheterization of the central vessels is a medical procedure. The subclavian vein, jugular and femoral veins can be punctured, both on the left and on the right. The central venous catheter can function and remain uninfected for many weeks. This is achieved through strict adherence to the rules of catheter care, including adherence to aseptic rules during its installation, precautions when performing infusions and injections.
General view of the set for central vein catheterization:
Indications and contraindications
The following indications for central venous catheterization are distinguished:
- Complex operations with possible massive blood loss
- Open heart surgery with AIK and in general on the heart
- Need for intensive care
- Parenteral (intravenous) nutrition
- Possibility of measuring CVP (central venous pressure)
- Possibility of taking multiple blood samples for control
- Insertion of a cardiac pacemaker
- X-ray and contrast examination of the heart
- Probing of the heart cavities
Contraindications
Contraindications for central venous catheterization are:
- Bleeding disorder
- Inflammatory at the puncture site
- Clavicle injury
- Bilateral pneumothorax and some others
However, you need to understand that contraindications are relative, because if a catheter needs to be inserted for health reasons, then this will be done under any circumstances, because To save a child's life in an emergency, venous access is needed.
For catheterization of central (main) veins, one of the following methods can be selected:
- Through the peripheral veins of the upper limb, usually the elbow. The advantage in this case is the ease of execution; the catheter is passed to the mouth of the superior vena cava. The disadvantage is that the catheter can remain in place for no more than two to three days.
- Through the subclavian vein on the right or left
- Through the internal jugular vein, also on the right or left
For puncture catheterization of the central veins: jugular, subclavian (and, by the way, arteries), the Seldinger method (with a guide) is used, the essence of which is as follows:
- A vein is punctured with a needle, a guidewire is passed through it to a depth of 10–12 cm
- Next, the needle is removed and the catheter is passed through the guidewire.
- After this, the guide is removed, the catheter is fixed to the skin with a plaster
If the catheter is in place for a long time, the following complications may occur:
- vein thrombosis
- catheter thrombosis
- thrombo- and air embolism
- infectious complications (5 - 40%), such as suppuration, sepsis (general inflammation), etc.
That is why central venous catheterization requires careful adherence to the rules of care and monitoring of the catheter:
- Before all manipulations, you should wash your hands, dry them and treat them with 70% alcohol, and put on sterile rubber gloves. The skin around the catheter is inspected daily and treated with 70% alcohol and 2% iodine solution or 1% brilliant green solution.
- The dressing is changed daily and when soiled.
- After completion of infusion therapy, it is necessary to place a heparin lock (special dilution of heaprin).
- It is prohibited to bend the catheter, place clamps on the catheter that are not intended for the design, or allow air to enter the catheter.
- If problems associated with the catheter are detected: pain, swelling of the arm, the bandage gets wet with blood, exudate or infusion medium, fever, catheter kinks, immediately inform your doctor.
- The catheter is removed by the attending physician or anesthesiology service staff, followed by a note in the medical history.
- It is prohibited to leave the hospital premises with a catheter! If referred to another medical institution, the patient must be accompanied by a health worker; In the discharge summary, a note is made about the presence of a subclavian catheter in the patient.
General appearance of the patient:
Varicose veins during pregnancy
Pregnancy does not cause varicose veins, but it is often a trigger for the appearance of varicose veins in those women who are predisposed to it. For example, in people with congenital insufficiency or even absence of venous valves. This fact has already been established quite definitely, because many pregnant women do not develop any varicose veins. Sometimes varicose veins appear only during the fourth, fifth or tenth pregnancy.
And in some women, they appear during pregnancy and disappear immediately after the birth of the child. Pregnancy acts as a triggering factor for varicose veins due to the fact that during pregnancy the content of sex hormones - estrogen and progesterone - in a woman’s blood increases sharply. These hormones, in high concentrations, help soften the venous walls, the veins stretch, and the valves cannot close normally because of this.
Other causes of varicose veins
Such a widespread prevalence of varicose veins in highly developed Western countries is probably associated with the lifestyle of the population. For example, we spend a lot of time sitting on chairs. From kindergarten until graduation, a person sits for at least 40 hours a week (counting approximately 5 hours during the day in class, 3 hours in the evening doing homework, watching TV, and so on 5 days a week). Now let's multiply these hours by 10 months a year, and so on - up to 17 years. Then - work in some institution where you have to sit even longer. When a person sits in a chair, the veins running along the back of the thighs are compressed, and the calf muscles (the rhythmic contractions of which help move venous blood to the heart) do not work.
Another important factor is nutrition. In Western countries, people prefer a low fiber diet. With such a diet, fecal matter becomes denser, and constipation often occurs. When straining to move hard stool, the abdominal muscles tense and the pressure in the abdominal cavity increases significantly. High pressure spreads to the veins running along the back of the abdominal cavity and to the veins of the legs, which dilate, causing the venous valves to leak.
VIENNS
VEINS are blood vessels that carry blood to the heart from organs and tissues, where they originate in a network of capillaries.
Also on topic:
CIRCULATORY SYSTEM
On the opposite side of the capillary bed, the vessels merge into numerous small channels, venules, which are comparable in size to arterioles. They continue to connect to form larger veins that carry blood from all parts of the body back to the heart. Constant blood flow in this direction is facilitated by a system of valves found in most veins. Venous pressure, unlike pressure in the arteries, does not directly depend on the tension of the muscles of the vascular wall, so blood flow in the desired direction is determined mainly by other factors: the pushing force created by the arterial pressure of the systemic circulation; the “suction” effect of negative pressure that occurs in the chest during inhalation; the pumping action of the muscles of the limbs, which, during normal contractions, push venous blood to the heart.
The walls of veins are similar in structure to arterial ones in that they also consist of three layers, however, much less pronounced. For the movement of blood through the veins, which occurs practically without pulsation and at relatively low pressure, it does not require such thick and elastic walls as those of the arteries. Another important difference between veins and arteries is the presence of valves in them, which maintain blood flow in one direction at low pressure. The valves are found in greatest numbers in the veins of the extremities, where muscle contractions play a particularly important role in moving blood back to the heart; large veins, such as the cava, portal and iliac veins, lack valves.
Also on topic:
ARTERY
Also on topic:
HEART
On their way to the heart, the veins collect blood flowing from the gastrointestinal tract through the portal vein, from the liver through the hepatic veins, from the kidneys through the renal veins, and from the upper extremities through the subclavian veins. Two vena cavae form near the heart, through which blood enters the right atrium. The vessels of the pulmonary circulation (pulmonary) resemble the vessels of the systemic circulation, with the only exception that they lack valves, and the walls of both arteries and veins are much thinner. In contrast to the systemic circulation, venous, non-oxygenated blood flows through the pulmonary arteries into the lungs, and arterial, i.e., flows through the pulmonary veins. saturated with oxygen. The terms “arteries” and “veins” refer to the direction of blood movement in the vessels - from the heart or to the heart, and not to the type of blood they contain.
Varicose veins in older people
Why varicose veins more common in older people, and especially common in women?
1. To answer briefly - because their vascular system wears out with age and, sooner or later, fails. However, there are still many objective reasons why older women suffer from varicose veins more often than younger men and women. Firstly, since women generally live somewhat longer than men, there are correspondingly more elderly women than elderly men, and their veins have been working harder for a longer period of time.
2. Men don't get pregnant. Even if varicose veins that appeared in a woman during pregnancy disappear soon after the birth of the child, these veins were still abnormally enlarged within a few months. And with age, all the muscles of the human body, including the smooth muscles of the vascular walls, become less elastic than in youth. And the veins, which had already expanded once, during pregnancy, in old age again become a little wider than normal.
3. Nowadays, many women over the age of 30 are resorting to hormone replacement therapy, which was originally intended to relieve the unpleasant symptoms of menopause. There is no doubt that hormone replacement therapy helps women look younger, feel better, and generally cope with the menopause years more easily. Doctors' observations also confirm that hormone replacement therapy to some extent reduces the frequency of angina attacks and prevents a decrease in bone strength due to osteoporosis.
However, hormonal supplements at the same time soften the vein walls in the same way as increased levels of estrogen and progesterone during pregnancy. This side effect of hormonal pills is all the more dangerous because the walls of the veins are already becoming weaker - due to natural age-related changes in the muscle layer. So, additional clinical studies are needed to definitively clarify this issue.
Veins of the lower extremities
Vienna
- these are vessels that ensure the outflow of blood from organs and tissues to the heart. The wall of the veins consists of three layers: internal (endothelium), middle (muscular) and external (adventitia). Unlike arteries, the walls of veins are thinner and contain few elastic fibers. Therefore, the veins are less elastic and collapse easily. In this case, the diameter of the veins is larger than that of the arteries. The peculiarity of the veins is that their diameter depends on many factors: body position, blood pressure, blood flow speed, condition of the valves and breathing phase.
The peculiarity of the veins in the legs is that they have valves. Venous valves are folds of the inner lining; they allow blood to flow towards the heart and prevent it from flowing back.
The flow of blood is carried out due to respiratory movements, the existence of constant muscle tone of the venous wall, constant support of blood from the arterial end of the capillary bed, and the suction action of the right parts of the heart. The main role in moving blood is played by the so-called “muscular-venous pump”. The deep veins that run in the legs are surrounded on all sides by muscles. When walking and physical activity on the legs, the muscles contract and squeeze blood upward.
If the valves are malfunctioning, during the operation of the muscle pump, there is no drop in pressure in the deep veins during muscle contraction. Venous blood is retained in the sinuses and venules, which leads to changes in capillary exchange parameters and the development of edema, pigmentation, itching and other symptoms of venous insufficiency.
The outflow of blood from the lower extremities is provided by three interconnected and clearly interacting systems: superficial veins, deep veins and communicating veins (perforators) connecting them.
Superficial veins
and their tributaries form venous networks under the skin. They can be felt and are quite visible. This network is especially clearly visible on the dorsum of the foot. From the superficial veins of the leg, it is customary to distinguish the large and small saphenous veins of the leg. Both saphenous veins receive other superficial veins along their path. Varicose veins on the legs concern the superficial veins.
Deep veins
. These veins are located between the muscles and connective tissue. The main outflow of blood (85-90%) is through the deep veins. These veins have valves that prevent blood from flowing back.
Superficial and deep veins are connected to each other by communicating veins
. The reason for the existence of these veins is to equalize the pressure between them. Damage to the valves of the communicating (perforating) veins leads to blood flowing from the deep veins to the superficial ones. Normally, the valves of these veins allow blood to flow in only one direction - from superficial to deep.
Types of varicose veins
Varicose veins are divided into two main groups:
- The first group includes primary varicose veins, caused by a hereditary predisposition to varicose veins.
- The second group includes varicose veins that appear after damage to the venous walls as a result of injury with the formation of blood clots in the veins or thrombosis.
When a clot or thrombus passes through a vein, the integrity of the venous valves is disrupted and secondary varicose veins are formed.
Varicose veins
Varicose veins are bundles of thin, purple or red veins that appear around the knees or ankles. (Sometimes such vascular “webs” can appear on the face, near the nose.) These vessels cannot be called varicose veins, since, by definition, varicose veins are veins that are increased in length and in diameter. In fact, these are slightly dilated venules (vessels connecting capillaries to the veins themselves), which are located close to the surface of the skin.
Such dilated venules appear due to increased levels of female sex hormones in the blood and are often found in women taking oral contraceptives. But venules can expand even in the presence of varicose veins of larger veins that do not appear externally. However, women with varicose veins often experience symptoms very similar to those of varicose veins.
Intensive care nurse: venous catheterization
One of the main responsibilities of an intensive care nurse is organizing venous access for a patient, or, more simply, catheterizing a vein. A catheter is placed in different cases: to take blood for analysis (sometimes tests are taken several times a day, and pricking again each time is painful and traumatic for the patient) or to administer drugs and nutritional solutions to the patient. Placing a catheter is almost no different from a regular injection - you just need the vein to be straight in a certain area.
Where you can inject and where you can’t
To select a vein, you need to roughly estimate why the catheter is being placed in the first place. For emergency patients with severe injuries, bleeding, or those who are being prepared for abdominal surgery, a large-diameter catheter is placed, and a large vein is selected accordingly. For a grandmother of a very elegant age, whose diagnosis is not so serious, a smaller catheter is selected - the veins at this age are most often no longer the same.
How to choose the injection site? Nurses start with the distal veins, i.e. those that are “on the periphery”: the veins of the hand, forearm. The principle of ascending from the hand above also works (bad veins on the hand - move to the forearm).
The veins on the elbow are clearly visible, but this place is not very suitable for catheterization. The person bends and straightens the arm, sometimes unintentionally, and the catheter can become kinked or broken. Although, if you don’t need to insert a catheter, but only one or two injections are expected, the elbow bend is what you need. The vein on it is thick enough and will withstand all this.
Elsewhere, the vein may not be visible, but with a tourniquet applied, it can be easily felt with the fingers (palpated). In this case, an experienced nurse will be able to give an injection without even seeing the vein. In some patients, the median ulnar vein is not visible, but you can feel another one, which is a little closer to the outside of the arm, the lateral saphenous vein (it is also not visible with the eyes). I have had cases when I fell into such veins almost blindly - my veins also have this feature, so I am well aware of it.
Treatment of varicose veins
Treatment depends on the severity of the disease. If the disease does not manifest itself too strongly, then conservative treatment is best:
- regular rest with your feet up,
- elastic bandaging (or special elastic stockings),
- physical exercises for leg muscles.
If these measures are not enough, the veins affected by varicose veins must be surgically removed at the Phlebology Center. Or using new, experimental methods - elastic strengthening of the venous walls is carried out surgically. That is, a special elastic plastic cover is placed on the outer surface of the affected veins in places of varicose veins, where incompetent venous valves are located. And finally, to treat dilated venules or varicose veins of small veins remaining after surgery, sclerotherapy - that is, the introduction of sclerosing substances into the areas of dilation, which causes clogging of the pathological vein. Blood returns to the heart through normal venous vessels.
Introduction:
The circulatory system is responsible for moving blood throughout the body. The main components of this system are the heart and blood vessels. The heart is the central organ of the circulatory system. With each heartbeat, blood is pumped through the arteries and delivers oxygen and nutrients to various organs and tissues, after which the blood returns back to the heart through other blood vessels - veins.
There are three types of blood vessels that play different roles. The two main types are arteries and veins. Arteries carry oxygenated and nutrient-rich blood away from the heart, and veins return waste blood back to the heart. Lymphatic vessels are the third component; they filter and “purify” the liquid part of the blood - plasma, before returning it to the general bloodstream.
Complications during treatment
The main danger with conservative treatment (elastic stockings, exercise and resting with legs elevated) is its possible ineffectiveness.
Surgical treatment of varicose veins of the lower extremities should currently be performed by experienced vascular surgeons and phlebologists . Often complications and relapses after surgical treatment are caused by the fact that the operation was not performed by a specialist from the phlebology center.
With sclerotherapy, the main nuisance is small dark spots that can remain at the injection sites for several months, or in some cases forever.
Dilated veins after surgical treatment
If varicose veins have been removed, varicose veins will no longer appear in their place. However, sometimes varicose veins are found after surgery - in veins that were not previously affected, or in small veins that were not identified during the preoperative examination. Varicose veins after surgery appear because the blood is forced to find new outflow paths. At the same time, a larger volume of blood is redistributed to the remaining veins than before, and if there were any defects in the valves or walls, then new problems arise. New varicose veins, as a rule, bring cosmetic inconvenience and can be easily eliminated by a phlebologist using modern sclerotherapy techniques.