Synonyms: EO
Eosinophils consist of a bilobed nucleus and three types of eosinophil granules (lipid bodies, eosinophils, small and primary). They contain protein structures with the help of which foreign cells are neutralized. Eosinophils are quite large cells: their diameter reaches 20 microns.
Eosinophils got their name due to the fact that when stained according to Romanovsky, they are easily stained with eosin (an acidic dye), while other types of dyes have no effect on them. Eosin itself was invented in 1873 by the German scientist G. Caro and, due to its bright pink color, was named after the ancient Greek goddess of the dawn Eos (in the German version the name sounds like “eosin”).
What are eosinophils?
The content of the article
Eosinophils are a type of granular leukocytes or granulocytes. Their cells include a bipartite nucleus and three types of eosinophilic granules - lipid bodies. They contain protein structures that neutralize foreign bodies and substances. Eosinophils are large cells with a diameter of up to 20 microns.
Eosinophils got their name because when stained according to Romanovsky, they are easily stained with eosin dye. This dye was invented in 1873 by the German scientist G. Caro and, because of its bright pink color, was named after the ancient Greek goddess of the dawn Eos - in the German version “eosin”.
Eosinophils are formed in the red bone marrow within 3-4 days. After this, they enter the bloodstream, accumulating in the mucous membranes of the intestines, respiratory tract and capillaries. There they live and function for 10-14 days. In peripheral blood the concentration of eosinophils is insignificant. There are about 200 times more of them in the bone marrow and other tissues.
Role and functions in the body
Eosinophils, as a type of white blood cell, are responsible for protection against foreign agents, which can be microorganisms, chemicals, and toxins. Eosinophils are often called scavenger cells, which have a special task. They are considered the most sensitive to parasitic infections and pathological bacteria. They usually begin their work after lymphocytes and neutrophils. Their option in this case is to dissolve the remains of pathogenic microorganisms.
These cells also participate in the “antigen-antibody” reaction, due to which they control the release of histamine, better known as a substance that causes allergies. Thanks to this, eosinophils help reduce the aggressiveness of the immune system's response to foreign proteins. Such blood cells can also penetrate vascular walls and move through tissues to the site of damage or inflammation.
Among the lesser known areas of responsibility of eosinophils is the prevention of thrombosis. However, they also have a downside. These blood cells can become dangerous, for example, when they are associated with pathological changes. This happens with Loeffler's disease. This is an allergic disease, when the number of eosinophils in the blood increases, and infiltrates form in the lungs, which, however, quickly disappear.
Vital interest. Six naive questions about tests Read more
Indications for analysis
A complete blood test with a count of eosinophils is prescribed for most people who visit the clinic.
The range of indications is very wide, but in modern clinical practice the initial eosinophil count is most often used:
- as a biomarker for assessing the effectiveness of drugs prescribed to patients with bronchial asthma;
- upon confirmation of a preliminary diagnosis;
- checking the effectiveness of the prescribed therapeutic course;
- assessing a person’s health status during medical examinations or medical examinations;
- in the postoperative period;
- if the development of infectious, oncological and autoimmune diseases is suspected.
Which blood test shows the level of eosinophils?
The exact number of eosinophils is indicated in the results of a blood test with a leukocyte formula. Blood is taken from a vein or finger for analysis. The study is carried out under a microscope using various reagents and dyes. During this analysis, the number of all types of leukocytes per unit volume of blood is calculated, as well as the percentage of each type of leukocyte. A leukogram (leukocyte formula) allows you to see the increase and decrease in the number of one or another type of leukocyte.
Norms of eosinophils in the blood
| Age | Normal level of eosinophils in the blood |
| Children under 5 years old | 0,5 – 7% |
| Children 5 – 14 years old | 1 – 5% |
| Adults | 0,5 – 5% |
In women, in the first days of menstruation, the level of eosinophils is slightly higher than normal, and after ovulation their number is slightly lower than normal.
An increased level of eosinophils in the blood is called eosinophilia.
Stages of eosinophilia
| Stage | Stage level | The number of eosinophils in the blood from the total number of leukocytes |
| First | Lightweight | no more than 10% |
| Second | Average | 10% – 15% |
| Third | Heavy | over 15% |
Eosinophils in allergies:
It is well known that eosinophils indicate the presence of allergies; during allergic reactions, their content in the blood can increase several times relative to the norm. However, it would be a mistake to assume that they increase the allergic reaction. On the contrary, eosinophils strive to balance the disturbed balance of the immune system, in which it gives such an explosive reaction to a stimulus. For example, these cells absorb histamine, a mediator of allergies. If there is too much of it in the body, it can cause a very serious situation: anaphylactic shock, from which you can die. Eosinophils save allergy sufferers from this, as they regulate the strength of the reaction and reduce it.
Causes of increased levels of eosinophils in the blood
An increase in eosinophils or eosinophilia is observed in the following diseases and conditions:
- diseases and conditions accompanied by allergic processes in the body - bloating, bronchial asthma, urticaria, Quincke's edema, serum sickness, drug sickness, etc.;
- parasitic diseases – ascariasis, giardiasis, toxocariasis, trichinosis, opisthorchiasis, echinococcosis, malaria, etc.;
- concomitant tissue diseases and systemic vasculitis - rheumatoid arthritis, mesothelial periarteritis, scleroderma, systemic lupus erythematosus, etc.;
- dermatological diseases - dermatitis, eczema, skin crocus, pemphigus, etc.;
- some infectious diseases - tuberculosis, scarlet fever, syphilis;
- blood diseases accompanied by the spread of one or more hematopoietic bacteria - chronic myeloid leukemia, erythremia, lymphogranulomatosis;
- taking sulfonamides, antibiotics and adrenocorticotropic hormones.
Long-term (more than six months) high eosinophilia of unknown etiology is called hypereosinophilic syndrome. The level of eosinophils in the blood exceeds 15%. This pathology is very dangerous, it causes damage to internal organs - heart, kidneys, bone marrow, lungs, etc.
If the content of monocytes and eosinophils in the blood is increased, this may indicate an infectious process in the body, a blood disease, or an early stage of cancer.
Sometimes the number of monocytes increases after recovery from various diseases.
If eosinophils are elevated
It is obvious that in children and adolescents the eosinophil count may increase to 6–7%, but this then goes away with age. If eosinophils are elevated in an adult, this indicates a pathology that requires diagnosis and treatment.
Eosinophils increase in children and adults in many diseases and conditions:
- infection with worms, especially lamblia, roundworms, strongyloides, echinococci, hookworms, schistosomes, toxocara, opisthorchiasis, pulmonary flukes and trichinella;
- asthma;
- allergy;
- hay fever;
- skin manifestations of allergies;
- malaria;
- recovery from infectious diseases;
- after taking antibiotics;
- serum sickness;
- hay fever;
- epidermolysis bullosa;
- atopic dermatitis;
- pemphigus;
- Dühring's dermatitis;
- nephroblastoma (Wilms tumor);
- carcinoma;
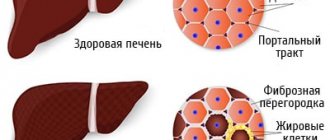
- cirrhosis of the liver;
- rheumatoid arthritis;
- pernicious (megaloblastic or B12-deficiency) anemia;
- all types of leukemia;
- lymphogranulomatosis (Hodgkin's lymphoma);
- polycythemia vera;
- fasciitis;
- Sezary syndrome;
- Wegener's granulomatosis;
- periarteritis nodosa;
- Churg-Strauss syndrome;
- sarcoidosis;
- pneumonia;
- Addison's disease;
- Loeffler's syndrome and Loeffler's endocarditis;
- condition after radiotherapy and irradiation;
- scarlet fever;
- Congenital heart defect;
- condition after removal of the spleen;
- GVHD after organ transplantation;
- tuberculosis of the lymph nodes;
- chorea;
- tumor metastases (especially to the bones and lungs);
- systemic lupus erythematosus.
An increase in these blood cells is called eosinophilia. The attending physician finds out the cause of this condition and looks for a way to eliminate it.
How to reduce the number of eosinophils in the blood?
First of all, it is important to eliminate the cause of eosinophilia, that is, the disease that caused a change in the leukocyte formula.
Possible treatment options:
- antiallergic therapy - taking antihistamines: chloropyramine, cetirizine, levocetirizine, desloratadine and loratadine, etc.;
- antibacterial therapy - taking antibiotics: amoxicillin, ceftriaxone, azithromycin, erythromycin, etc.;
- anti-inflammatory therapy - taking drugs for inflammatory processes, for example glucocorticosteroids - prednisolone;
- chemotherapy – to eliminate malignant tumors;
- hormone therapy;
- anthelmintic therapy - taking albendazole, levamisole, bephenium hydroxynaphthoate, piperazine, tetrachlorethylene, mebendazole. The choice of medication depends on the type of parasite and the stage of infestation.
Additionally, the following measures can be taken:
- Normalize your lifestyle. It is important to avoid frequent drinking of alcohol and give up cigarettes.
- Avoid chronic intoxication. In people working in hazardous industries or living in environmentally unfavorable regions, the number of eosinophils in the blood increases as a result of constant chemical intoxication.
- Stick to a healthy diet. You should not overuse spicy, smoked, canned and fatty foods. To increase the level of eosinophils, you should limit the amount of meat, poultry and fish in your diet, and consume mainly their low-fat varieties. The menu should include yogurt, cheeses, vegetables, fruits, beans, bran and whole grain bread.
Eosinophils and phagocytosis:
The entire immune system is mobilized to protect health, and each of its elements works in its own way. The eosinophil count also increases when any harmful object enters the body. Eosinophils have a clear reaction to the “enemy”: to fight it, they turn into phagocytes and devour foreign particles.
Unfortunately, they are not able to cope with all possible aggressors; These cells are powerless against especially large objects. However, they are capable of neutralizing small particles (viruses, small bacteria, molecules of toxic substances). Like full-fledged phagocytes, they approach the object of attack, capture it with their pseudopods, “swallow” and digest it. The destruction of the object occurs thanks to the enzymes contained in the lysosomes of eosinophils. Because the ability of eosinophils to phagocytose depends on the size of harmful particles, these cells are classified as so-called microphages.
Despite the fact that when describing the function of eosinophils, the ability indicated above is always mentioned, their main significance is not the absorption of microbes. What?
How to increase the number of eosinophils in the blood?
A decrease in the level of eosinophils in the blood is a sign of weakened immunity. As in the case of eosinophilia, the primary pathology should be identified and eliminated, as well as lifestyle adjustments:
- minimize bad habits;
- ensure an adequate level of physical activity;
- take care of the normal daily routine;
- consume more foods containing vitamins B12, C, D - meat, fish, cottage cheese, rose hips, currants, garlic, or use pharmacy multivitamins.
- It is advisable to exclude foods with a high allergenic potential: milk, soy, wheat, eggs, seafood, peanuts.
Changes in the level of eosinophils in the blood can be caused by both physiological reasons - physical activity, stress, overeating, and various diseases. Sometimes the same condition, for example, an allergy or an infectious process, can cause both a decrease and an increase in the number of eosinophils in the blood and other biological fluids.
Eosinophils
It is believed that eosinophils are rare white blood cells whose activities are mainly destructive and are related only to parasitic infections and asthma. However, is this rather banal conclusion correct? Inflammatory bowel disease is characterized by the invasion of white blood cells into the intestinal mucosa. However, there is a mixed inflammatory pattern that includes neutrophils, lymphocytes, monocytes and eosinophils. To this day, the role of eosinophils in health and disease remains unclear. Traditionally, research into their function has focused primarily on allergic diseases, asthma, and parasitic infections. Unlike the lungs or skin, eosinophils are found in the normal intestinal mucosa and enhance pathological conditions; therefore, a complex system must regulate their migration and numbers.
A significant body of literature describes eosinophils present in the gastrointestinal microenvironment, where they can interact with other resident cells, thereby promoting intestinal remodeling, mucus formation, the epithelial barrier, cytokine production, angiogenesis, and neuropeptide release. A number of lines of evidence support both the potential beneficial and harmful roles of eosinophils in the intestine.
Eosinophils are pleiotropic multifunctional leukocytes involved in the initiation and propagation of various inflammatory responses, as well as modulators of innate and adaptive immunity. The biology of eosinophils is of interest, and the main attention here should be paid to the transcriptional regulation of eosinophil differentiation, characterization of the growing properties of eosinophil protein granules, surface proteins and pleiotropic mediators, and the molecular mechanisms of eosinophil degranulation. New insights into the role of eosinophils in homeostatic function, including developmental biology and innate and adaptive immunity (as well as their interactions with mast cells and T cells) and their putative role in disease processes including infections, asthma and gastrointestinal disorders are important.
Eosinophilic granulocytes have long been considered potent effector cells capable of releasing a range of inflammatory mediators involved in cytotoxicity, helminths, and tissue destruction in chronic inflammatory diseases such as asthma. However, it has become apparent that eosinophils are also involved in regulatory mechanisms that modulate local tissue immune responses. Eosinophils are involved in remodeling and repair mechanisms and contribute to localized innate and adaptive immune responses, as well as systemic adaptive immunity. In addition, eosinophils participate in neuroimmune interactions that modulate the functional activity of peripheral nerves. Neurotransmitters can also modulate the functional activity of eosinophils by mediating bidirectional interactions between the two cell types. Eosinophils are tissue-specific cells and have been found in close proximity to peripheral nerves.
Although the functional role of eosinophils is primarily thought to be host defense against parasitic infection, current research suggests that this complex cell is ideally suited for other roles that may include immune modulation and tissue repair. Eosinophil is an important source of essential proteins, lipid mediators, cytokines and growth factors. In disease states, eosinophil mobilization from the bone marrow and circulation can be very rapid but highly organized and cell selective, particularly in response to interleukin (IL) 5 and eotaxin. This complex recruitment pathway is regulated by a series of interactions between eosinophil receptors and endothelial and extracellular matrix ligands. Several priming mechanisms activate eosinophils during this recruitment process so that the cell reaches its tissue destination primed for immediate action and prolonged tissue survival. Degranulation is tightly controlled and allows the cell to release its contents differently in an orderly manner. This is important to prevent tissue damage during migration. Therapy remains limited for eosinophil-driven diseases, but interfering with key events that drive eosinophil recruitment and effector function may be a way forward.
Some of the roles of eosinophils are based on the acute, effector responses of this cell, its ability to generate biologically active lipid mediators and release granule contents, including characteristic cationic proteins. While effector responses of eosinophils are important for their contribution to the acute pathogenesis of allergic diseases, a more complete understanding of the eosinophil requires an appreciation of the role that this cell may play at tissue sites, particularly at submucosal sites where the cell is typically localized in the absence of disease. Moreover, for the long-lived, resident eosinophil, determining the interactions that occur between eosinophils and other immune cells is critical to understanding eosinophil function in both acute and chronic diseases. Many allergic diseases are characterized by increased accumulation of eosinophils and are chronic diseases.
The infiltration of eosinophils into tissue allergic inflammation is mediated by a combination of processes. Eosinophil L-selection and very late activation antigen (VLA-4) may selectively regulate eosinophil adhesion to the endothelium. Activating cytokines such as interleukin (IL)-5 are regulated upon activation in normal T cells (RANTES) and monocyte chemotactic peptide (MCP)-3 specifically act on eosinophils. In addition, eosinophils from allergy patients may be activated to increase adhesion and movement by chemokines released at sites of allergic inflammation. Together, these processes cause a specific infiltration of eosinophils.
Reduced blood glutathione levels and blood eosinophil levels were studied over many weeks in patients given placebo. The laboratory changes that accompany placebo improvement develop slowly and differ from the rapid changes produced by some drugs.
Eosinophils can regulate local immune and inflammatory responses, and their accumulation in the blood and tissues is associated with several inflammatory and infectious diseases. Thus, eosinophil-targeted therapies may help control a variety of diseases, including atopic disorders such as asthma and allergies, as well as diseases that are not primarily associated with eosinophils, such as autoimmune diseases and malignancies. Eosinophil-targeting drugs that target specific steps associated with eosinophil development, migration, and activation have recently entered clinical trials and have provided encouraging results and insight into the role of eosinophils
Activation of eosinophils results in the release of preformed and newly synthesized products, including cytokines, chemokines, lipid mediators, and cytotoxic granule proteins, which can initiate, enhance, and maintain local inflammatory and remodeling responses. Eosinophil secondary granules are composed of highly charged basic proteins, including basic eosinophil granule proteins, eosinophil cationic protein, eosinophil-derived neurotoxin, and eosinophil peroxidase. In addition, eosinophil granules contain a variety of preformed cytokines, chemokines, enzymes, and growth factors, leading to diverse biological activities of eosinophils during infection and inflammation. Although glucocorticoids are very effective in reducing the number of eosinophils in the blood and tissues, patients often have dangerous side effects and develop resistance to these drugs. A therapy targeting the eosinophil growth factor interleukin-5 (IL-5) has been tested in clinical trials for effectiveness in several eosinophilia-related disorders and appears promising. However, the reduction in tissue eosinophilia and improvement in symptoms was variable and depended on patient phenotypes (subgroups). Thus, additional approaches to patient selection and new drug selection based on understanding the mechanism of eosinophilia and the effector functions of eosinophils are needed.
Preclinical studies suggest that inhibition of eosinophil migration from the bloodstream into tissues has therapeutic potential, but clinical success to date has been limited. The lack of efficacy may be due to complex regulation of eosinophil recruitment to inflammatory tissues. Preclinical studies targeting the promotion of eosinophil apoptosis support the relevance of studies of sialic acid-binding immunoglobulin-like lectin 8 (SIGLEC-8)-targeted therapy, as recruitment of SIGLEC-8 leads to selective eosinophil apoptosis.
Treatment of patients with allergic asthma with omalizumab, a recombinant monoclonal antibody that binds to immunoglobulin E, reduces eosinophilia in the blood and tissues through a yet unknown mechanism.
Clozapine
There have been reports in the literature of fever and diarrhea associated with the use of clozapine. However, the etiology of these symptoms is not clear. Eosinophilic colitis was suspected in these cases, although there was never any pathological confirmation of this hypothesis of findings. The researchers noted the presence of an increased erythrocyte sedimentation rate in this case, as is often observed in eosinophilic colitis. Histological examination of eosinophilic colitis usually shows the presence of patchy clusters or sheets of eosinophils in the lamina propria and crypt epithelium. The histopathology observed in patients is typically consistent with eosinophilic colitis.
Eosinophilic myocarditis is a rare form of myocarditis characterized by myocardial infusion consisting primarily of eosinophils. It is known that it can develop at a rate of 0.2-3% with long-term therapy, especially with clozapine. Standard treatment cannot be established due to the rarity of the disease and difficulties in determining the etiology. When examining areas of the myocardium using a light microscope, general conclusions were drawn: myocyte damage was accompanied by a patchy distribution of perivascular and interstitial inflammatory infiltrate rich in eosinophils. These entities may have developed as a result of a hypersensitivity reaction due to long-term use of antipsychotic drugs. Eosinophilic myocarditis occurs as a rare clinical entity and is probably a subtype of myocarditis that is not always recognized. Failure in clinical diagnosis and delay in treatment can lead to irreversible myocardial damage. Endomicrobial biopsy is still the gold standard in the diagnosis of eosinophilic myocarditis.