Paget-Schroetter syndrome is a thrombosis of the subclavian vein, extending to the subclavian and axillary veins, as well as to the veins of the shoulder, which leads to impaired venous outflow in the arm. The syndrome is also called traumatic thrombosis or effort syndrome. Despite its relative rarity, it has become increasingly diagnosed in the last decade. The main complaints are swelling of the tissues of the upper limb and bursting pain.
The first case of the syndrome was described by James Paget in 1875, and in 1894 von Schrötter identified vascular injury as a potential cause of the disease. The term Paget-Schroetter syndrome was first used in 1948.
General information about thrombosis
Thrombosis
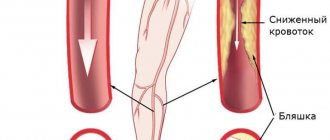
ー the process of intravital blood coagulation in the cavities of blood vessels and the heart. This process is also dangerous because part of the blood clot can break off and be carried by the bloodstream to other organs. For example, with thrombosis of the deep veins of the lower extremities, thromboembolism of the pulmonary artery or cerebral vessels often develops.
5.3. Therapeutic tactics for deep vein thrombosis
Conservative treatment
Bed rest and elevated position of the limb can reduce pain, but strict bed rest does not significantly affect the incidence of pulmonary embolism, provided that the verified thrombosis is not floating. Moreover, pain and swelling decrease much faster with early activation and adequate compression of the lower extremities using specialized grade 2-3 compression hosiery. When the edema is unstable (i.e., the volume of the limb has significant daily dynamics), the use of elastic bandages of long extensibility is permissible.
The need for adequate anticoagulant therapy as the basis for the treatment of patients with DVT (including asymptomatic ones) is undeniable. Anticoagulant therapy with UFH or LMWH in cases of reasonable suspicion of DVT can be started before instrumental verification of the diagnosis.
Treatment begins with parenteral administration of therapeutic doses of anticoagulants.
Treatment regimen with unfractionated heparin
1. Intravenously with a bolus of 80 IU/kg (or 5000 IU) and infusion at an initial rate of 18 IU/kg per 1 hour (or 1250-1300 IU/h), then selecting the IU dose based on APTT values. The goal is to maintain an aPTT of 1.5 to 2.5 times the laboratory-specific upper limit of normal.
2. Intravenously with a bolus of 5000 and then subcutaneously 450 IU/kg per day every 8 hours with dose selection to maintain APTT values 4 hours after injection 1.5-2.5 times the upper limit of normal for a specific laboratory
It is known that the frequency of rethrombosis with an aPTT that is within 1.5-2 from the norm is 4-6%, while with an aPTT that is less than 1.5 from the norm, the frequency of rethrombosis increases to 23%.
It must be remembered that the use of heparin can induce thrombocytopenia, therefore, when treating with heparin, it is necessary to monitor the level of peripheral blood platelets on days 1, 3, 5, 7 and 10. It is also necessary to monitor the hematocrit, hemoglobin level and creatinine clearance.
LMWHs have better bioavailability and more predictable pharmacokinetics and pharmacodynamics when administered subcutaneously. Due to these properties, LMWHs do not require constant laboratory monitoring other than platelet count determination. The exceptions are patients with severe underweight or excess body weight, as well as patients with renal failure. In these cases, determination of anti-Xa activity is recommended. In addition, the pharmacodynamics of LMWHs allow their use once or twice a day.
Treatment regimen with low molecular weight heparins:
Clexane (Enoxaparin)
1. Subcutaneously 100 anti-Xa IU (1 mg)/kg 2 times a day
2. Subcutaneously 150 anti-Xa IU (1.5 mg)/kg 1 time per day
Fragmin (Dalteparin) 1. Subcutaneously 100 anti-Xa IU/kg 2 times a day
2. Subcutaneously 200 anti-Xa IU/kg (maximum 18,000 IU) once a day
Fraxiparine (Nadroparine)
1. Subcutaneously 86 anti-Xa IU/kg 2 times a day
2. Subcutaneously 172 anti-Xa IU/kg (maximum 17,100 IU) once a day
Fondaparinux
Subcutaneously 5 mg 1 time per day for a body weight of 50 kg; 7.5 mg 1 time per day for body weight 50-100 kg; 10 mg once a day for body weight over 100 kg
Primary anticoagulant therapy with LMWH and UFH usually requires a switch to oral anticoagulants to maintain the anticoagulant effect for a long time. Currently, vitamin K antagonists (Warfarin) are used for this purpose. Given the delayed pharmacological effect of VKA, it is necessary to start taking warfarin in parallel with parenteral administration of therapeutic doses of anticoagulants for at least 5 days. Parenteral administration of anticoagulants can be stopped when therapeutic INR values (2.0–3.0) are reached twice, with an interval of 1 day.
In accordance with modern domestic and foreign recommendations, the duration of anticoagulant therapy for patients with primary DVT after surgery or long-term immobilization should be 3 months. For patients with idiopathic DVT - 6-12 months. Among cancer patients, it is preferable to use LMWH instead of VKA for 3-6 months. In patients with primary DVT and identified antiphospholipid antibodies and thrombophilia, it is recommended to continue VKA therapy for at least 12 months. In the future, the issue will be resolved individually. For recurrent DVT, lifelong use of VKA is recommended.
Surgery
Acute phlebothrombosis in the deep vein system of the lower extremities is a systemic disease that not only negatively affects the venous and lymphatic return system, but also worsens the function of the cardiovascular system as a whole. If you do not take active steps to treat this pathology, the further course of the pathological process becomes persistent and irreversible, prone to progression. The need for thrombus removal (surgery or thrombolytic therapy) is part of a strategy aimed at reducing the risk of developing post-thrombotic syndrome, especially in cases of widespread thrombosis.
Minimally invasive methods
Today, this is the most common group of methods in clinical use, designed to solve the above problems in the treatment of patients with deep phlebothrombosis. Here it is necessary to distinguish three subgroups of methods: 1. Installation of vena cava filters or partial vena cava plication. 2. Regional and systemic thrombolysis. 3. Catheter thrombus extraction and rheolytic thrombectomy.
Installation of vena cava filters and partial vena cava plication
At the beginning of the development of phlebology as a separate surgical specialty, one of the main issues requiring immediate resolution was the issue of preventing pulmonary embolism during phlebothrombosis. After the development in 1959 of the method of external plication of the vena cava with mattress sutures and external plication with clamps, it was possible to determine the further direction of solving the problem of acute deep phlebothrombosis and its complication - pulmonary embolism. Until 1967, the method, in combination with conservative therapy, remained the only clinical approach to this problem. Despite the fact that the technology of external partial clipping with clamps is associated with the need for traumatic surgical access and is practically impossible in seriously ill patients, this approach has been used and improved in limited situations to this day (for example, using endovideoscopic techniques). The Mobbin-Addin intraluminal umbrella vena cava filter, created and clinically applied in 1967, was the first experience of such endovascular intervention. Further development of this direction was carried out mainly along the path of improving the design of vena cava filters and studying their effect on hemodynamics and the clinical course of the main process. Indications for implantation of a vena cava filter are the impossibility and ineffectiveness of adequate anticoagulant therapy, a floating thrombus with a narrow base, the impossibility of its surgical removal, and recurrent pulmonary embolism in patients with high pulmonary hypertension.
In young patients with removable risk factors and causes of DVT, it is necessary to implant removable models, which are removed up to 30 days after installation when the threat of pulmonary embolism is eliminated.
It has been repeatedly noted that as a result of the installation of vena cava filters, pulmonary embolism may occur in the immediate period with a frequency of 1.5–8%, and thrombosis of the inferior vena cava occurs within a period of up to 3 years with a frequency of 12–25%.
There is no doubt that the installation of a vena cava filter is a manipulation that in itself poses a threat to the patient’s life and significantly affects the quality of life.
Justification for removing a blood clot
The basis of postthrombotic disease is the difficulty of venous outflow, which leads to pathophysiological changes characteristic of chronic venous insufficiency: edema, hyperpigmentation and lipodermatosclerosis. It is the disruption of venous outflow caused by obstruction that leads to the most severe forms of postthrombotic disease. Thus, treatment tactics aimed at removing the thrombus are pathophysiologically justified and significantly reduce the risk of severe post-thrombotic disease.
It has been shown that in patients who underwent deep vein thrombectomy, the function of the venous valves of the femoropopliteal segment is more often preserved than in patients who received only anticoagulant therapy. Positive experience is also accumulating, showing the high effectiveness of selective thrombolytic therapy, especially for ileofemoral phlebothrombosis.
Thrombolytic therapy
The first attempts at systemic thrombolytic therapy using plasminogen activators for the treatment of venous thrombosis were accompanied by a high incidence of hemorrhagic complications and an unsatisfactory thrombolytic effect. According to large randomized trials, less than half of patients treated with systemic thrombolysis experience a positive effect. The results of treatment using only anticoagulants are even less reassuring: only 4% have complete recanalization, and 14% have partial recanalization. In the remaining 82% of patients, either there are no objective signs of improvement at all, or there is deterioration.
Regional catheter thrombolysis
The main mechanism of thrombolysis is the activation of fibrin-bound plasminogen and its conversion to its active form - plasmin. Local application of plasminogen activator to thrombus is more effective and potentially safer than its systemic use. With local administration of a thrombolytic drug into thrombotic masses, its total dose and duration of administration are reduced, which reduces the risk of developing hemorrhagic complications.
Numerous studies show encouraging results in the treatment of acute deep vein thrombosis using regional catheter thrombolysis. Urokinase and recombinant tissue plasminogen activator (RT-PA) were most often used as thrombolytic drugs. Satisfactory treatment results are observed in 75-90% of cases. The incidence of hemorrhagic complications ranges from 5 to 11%. However, intracranial hemorrhages are rare. Most hemorrhagic complications develop at the site of venous access. Clinically significant PE and fatal PE are also rare. A study of the quality of life shows that after regional catheter thrombolysis, the quality of life of patients is higher than in the group of patients who received only anticoagulant therapy.
Pharmacomechanical thrombolysis
Despite the good results achieved with regional catheter thrombolysis, treatment is often lengthy, which in turn increases the risk of bleeding. The average time to perform catheter thrombolysis is 71 hours. In addition, when performing it, it is necessary to monitor the patient in the intensive care unit. These shortcomings led to the development of a combined technique of mechanical action on a thrombus with pharmacotherapy in order to quickly restore venous blood flow. Methods of mechanical action on a thrombus include endovascular mechanical thrombectomy using a catheter (AngioJet, Amplatz, etc.), ultrasound-enhanced thrombolysis, and isolated segmental pharmacomechanical thrombolysis (ISPMT). One of the important conditions for performing pharmacomechanical thrombolysis is that the period from the onset of the first symptoms is no more than 7-14 days. According to the literature, pharmacomechanical thrombolysis shows good results with a shorter duration of patient stay in the intensive care unit and a comparable number of hemorrhagic complications.
It should be noted that Russian experts do not recommend the widespread use of regional thrombolytic therapy. An exception is thrombolytic therapy for primary thrombosis of the subclavian vein (Paget-Schretter disease).
Open thrombectomy for ileocaval phlebothrombosis
Performing timely open thrombectomy for ileocaval phlebothrombosis allows one to achieve good immediate and long-term results with a relatively small number of complications. All embolic thromboses are subject to surgical treatment. A floating thrombus with a length of more than 4 cm and a narrow base is considered embologenic (embologenic). The choice of surgical treatment method is determined by the level of thrombosis, prevalence, presence of concomitant pathology of the patient, as well as the technical capabilities of the hospital.
In case of obstructive phlebothrombosis, radical thrombectomy is performed in cases of segmental lesions with a short (up to 5 days) duration of the disease.
Positive long-term results of thrombectomy are due to restoration of patency of the proximal segment of the vein and preservation of the function of the valve apparatus distal to the thrombosed area. A favorable outcome of the operation depends on the correct technical performance of the operation and the absence of recurrent thrombosis. Therefore, special attention must be paid to the details of surgical technique, the most complete removal of thrombotic masses, as well as adequate anticoagulant therapy in the postoperative period.
A number of clinical studies have shown that early thrombectomy for ileocaval thrombosis allows one to achieve good long-term results with restoration of patency of the venous segment in 75-80% of cases. Most patients experience a decrease in the frequency of edema and other symptoms of postthrombotic disease in the long-term period.
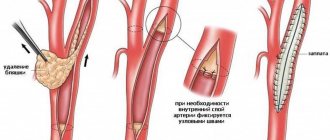
Technique for performing venous thrombectomy
A longitudinal incision in the groin area is used to access the common femoral vein, superficial femoral vein, saphenofemoral anastomosis and deep femoral vein. A venotomy of the common femoral vein is performed to provide access to the mouth of the saphenous and deep femoral veins.
If there are thrombotic masses below the inguinal ligament, the lower limb is raised and a tight elastic bandage is performed. The foot bends dorsally. Once all thrombotic masses below the inguinal ligament have been removed, balloon catheter thrombectomy is performed in the ileofemoral segment. Thrombectomy from the ileofemoral segment is performed with a balloon catheter No. 8 or 10. Before inserting the catheter into the inferior vena cava, it is necessary to remove the maximum possible amount of thrombotic mass in parts. It is advisable to perform “proximal” thrombectomy under X-ray control with the introduction of contrast into the balloon, especially in cases where a vena cava filter is installed, there is occlusion of the inferior vena cava or difficulties in inserting the balloon catheter. During this stage of the operation, positive end-expiratory pressure should be created to reduce the risk of developing pulmonary embolism. If the thrombus is localized in the inferior vena cava, thrombectomy can be performed with the additional creation of balloon occlusion of the inferior vena cava proximal to the border of the thrombotic masses, which is an alternative to the installation of a vena cava filter (Fig. 5.7).
Rice. 5.7.
Creating balloon occlusion of the inferior vena cava proximal to the upper border of thrombosis to prevent the development of pulmonary embolism may be an alternative to implantation of a vena cava filter.
After completion of thrombectomy from the ileofemoral segment, phlebography/-scopy should be performed intraoperatively to assess the patency of the iliac veins. Intravascular ultrasound can be used as an additional highly informative method of intraoperative monitoring.
Venous thrombectomy is recommended to be performed under general anesthesia. Of course, such surgery can be performed by experienced, well-trained personnel.
Surgical interventions for ileofemoral and femoropopliteal phlebothrombosis
The level of thrombosis below the common iliac vein allows intervention without inserting catheters and other traumatic instruments into the lumen of the vein.
Fundamentally, the solution to the problem of surgical thrombectomy from the femoral-popliteal segment is today being considered in two directions: solving the problem by switching phlebohemodynamics to the deep femoral vein and by restoring the natural flow with the possible preservation of the valve apparatus of the femoral and/or popliteal veins themselves. If the presence of an embologenic thrombus in a segment can be considered an absolute indication for active tactics, then with occlusive thrombi the issue is resolved taking into account the duration of the process. It is known that effective thrombectomy is possible only for blood clots no more than 3-7 days old [Savelyev V.S., 2001]. There is a common opinion that one should adhere to careful tactics when surgically removing thrombus masses from the femoropopliteal segment, completing the operation by ligation or resection of the ostial segment of the femoral vein itself, assessing the immediate results as good in the absence of symptoms of chronic venous insufficiency. The calculation with this approach is to switch the main venous flow to the deep vein of the thigh, which should ensure a stable outflow. However, it is known that the latter only in 38% of cases has a direct connection with the popliteal vein.
That is why a method of thrombectomy has been proposed in the treatment of embologenic phlebothrombosis, aimed not only at removing the thrombus, but also at preserving the femoral vein as a full-fledged organ, including the valve system.
It has been shown [Kaidorin A. G., Tsyplyashchuk A. V., 2008] that circular isolation of the vein leads to a pronounced disturbance of intramural blood circulation and, as a consequence, cicatricial changes in the wall and valvular deformation.
Therefore, during access, only the anterior internal wall of the vein is isolated from the perivenous tissue for 1-2 cm, if possible damaging the adventitia only along the cut line and no more than 1/2 of the circumference.
At 1-1.5 cm above the projection of the base of the floating part of the thrombus and always above the proximal valve of the femoral vein in the transverse direction, U-shaped stay sutures are applied with a 6/0 monofilament thread, between which the lumen of the vein is opened transversely.
When the intra-abdominal pressure increases (the patient strains), the floating part of the thrombus spontaneously dislocates into the wound under the pressure of the reverse blood flow. After obtaining retrograde blood flow, the free vein above the incision site is pressed with a soft pad or finger.
With an adequate size of the phlebotomy hole, in some cases, the removed thrombus can serve as a temporary tampon to prevent blood from leaking into the wound.
Then, using intense progressive compression of the soft tissues of the leg and thigh, blood clots are removed from the distal deep veins of the lower extremity.
If it is impossible to completely remove thrombus masses along the entire length of the vein, it is imperative to ensure and evaluate the quality of the antegrade flow through the PCBV. The latter is necessary to assess the prospects for maintaining valve function. If it is not possible to achieve antegrade blood flow, and the wall of the femoral vein in the operation area is subject to inflammatory or scar-sclerotic changes, it should be ligated below the confluence of the deep femoral vein, since the likelihood of rethrombosis is high.
With adequate antegrade blood flow, making sure that there are no moving parts of the thrombus, the U-shaped sutures are tightened, and a valve-like duplication is formed, providing temporary hemostasis. Temporary hemostasis is also easily accomplished by digital pressure above and below the phlebotomy defect (through the mass of perivasal tissue.
The above thrombectomy technique does not require circular isolation of veins and arteries, and therefore is technically simple and takes less time.
Postoperative period
In the postoperative period, parenteral administration of anticoagulants continues. In parallel, the dose of oral anticoagulants is adjusted until the target INR value is reached (2.0–3.0)
Subsequently, it is advisable to perform variable pneumocompression on both lower extremities. It is mandatory to wear compression stockings with a pressure of 30-40 mmHg. Art. at ankle level. Wearing compression hosiery helps to avoid the development of severe post-thrombotic disease.
Choice of tactics (assessment of risk factors, patient selection)
One of the significant factors limiting surgeons' enthusiasm for thrombectomy is the threat of intraoperative pulmonary embolism. This risk is especially high in patients with non-occlusive thrombus in the iliac and inferior vena cava. In this regard, it is fundamentally important to know the proximal extent of the thrombus, which will allow choosing an adequate method of preventing pulmonary embolism (implantation of a vena cava filter, balloon occlusion). The disadvantages and contraindications of thrombolytic therapy can be significantly reduced by using regional thrombolysis and reducing the thrombolytic dose.
A thorough assessment and analysis of risk factors and concomitant pathology allows us to identify a significant group of patients with ileofemoral phlebothrombosis, for whom active surgical tactics are indicated. First of all, in the light of the thrombus removal strategy, patients with an occlusive thrombus in the ileofemoral segment should be considered, since it is these patients who often develop severe, disabling post-thrombotic disease.
In the Pirogov Center, in the absence of contraindications, the priority is active surgical tactics in relation to patients with ileofemoral phlebothrombosis. Over the past 5 years, more than 1000 patients with deep vein thrombosis have been treated. Based on this experience, an algorithm for the management of such patients has been developed, presented in Fig. 5.8.
Rice. 5.8.
Algorithm for treatment tactics for patients with ileofemoral phlebothrombosis
Classification of thrombosis
Depending on the location of the pathological process:
Arterial:
- arteries of the brain;
- hearts;
- intestines (mesenteric thrombosis);
- liver;
- femoral artery and others.
Venous (phlebothrombosis):
- veins of the lower limb;
- hemorrhoidal plexus;
- femoral and iliac veins;
- cavernous sinus (intracranial collector of venous blood);
- retinal veins.
According to the severity of the disease, acute
ー a sharp blockade of blood flow, and
a chronic
ー thrombus grows gradually, the tissues have time to adapt to this and compensate for pathological changes.
Causes of thrombosis in the superior vena cava system
– basically the same as other venous thromboses. It may also develop as a complication of venous catheterization (cubital, subclavian catheter), sometimes arising as a result of prolonged compression or uncomfortable position of the upper limb (for example, during sleep).
The most common is thrombosis of the axillary or subclavian vein (Paget-Schrötter syndrome). Within 24 hours, swelling of the entire upper limb occurs with cushion-like swelling of the hand. There may be slight bursting pain. The color of the limb is unchanged or slightly cyanotic.
Mechanism of development and causes of thrombosis
There are three pathological parts in the process of intravascular thrombus formation:
- Violation of the integrity of the vascular wall. When the internal lining of blood vessels is damaged, enzyme systems are activated, which trigger the process of blood clotting.
- Slowing blood flow. This occurs when the outflow is disrupted (compression of veins, varicose veins), prolonged absence of limb movement, or heart failure.
- Blood thickening. Caused by dehydration, autoimmune diseases, chemotherapy, and oral contraceptives.
A blood clot often forms against the background of such diseases:
- atherosclerosis;
- heart failure;
- aneurysms of blood vessels and heart;
- diabetes;
- obesity;
- bone fractures;
- hormonal disorders;
- oncological diseases.
Embolism.
Embolism most often leads to acute arterial occlusion. Embolism refers to the entry of a foreign body into the arterial bed, leading to its blockage. Most often, emboli are pieces of an organized blood clot, accumulations of fat or gas, or other foreign bodies (plastic tubes, metal objects, bullets). Peripheral artery embolism occurs 2 times more often in women than in men, which is explained by women’s greater susceptibility to rheumatism and longer life expectancy. Emboli can occur at any age, but more often from 40 to 80 years. The main sources of peripheral arterial embolism are currently considered to be heart disease (95% of all cases). Moreover, more than half of them are due to atherosclerotic cardiopathy: atrial fibrillation, myocardial infarction, post-infarction cardiosclerosis, cardiac aneurysms. Acquired heart disease accounts for 40-43% and congenital defects 1-2%. In atherosclerotic cardiopathy, the thrombus is usually localized in the left ventricle, and in case of heart defects in the left atrium or its appendage. Following arterial embolism, acute ischemia of the limb or organ supplied by this vascular system develops. Its severity will depend on a number of factors: 1. the severity of bypass circulation, 2. continued thrombosis, 3. arterial spasm, 4. the state of central hemodynamics. A drop in intravascular pressure to a stagnation level leads to platelet aggregation and the formation of blood clots in the microcirculation system. As a result, irreversible changes in tissues occur. Later, thrombosis develops in larger arteries. Different tissues vary in their tolerance to ischemia. So in the tissues of the extremities, irreversible changes with complete ischemia occur after 6-8 hours, in the intestines after 2 hours, in the kidneys 40-50 minutes, in the brain after a few minutes.
Clinical course and symptoms of peripheral artery embolism.
The main symptom of arterial embolism is pain in the affected limb. It occurs suddenly and is very strong. Sometimes patients fall, unable to withstand this severe pain. Along with pain, patients often note a feeling of numbness in the limb. Upon examination, a change in the color of the skin of the limb is striking: from pronounced pallor to a “marble” color. In the late stage of ischemia, when thrombosis of the venous bed occurs, the color of the skin becomes cyanotic. With comparative palpation, the difference in skin temperature is noticeable, especially in the distal parts of the limb. There is also a disorder of all types of sensitivity (pain, tactile, deep). The border of sensitivity disorder does not coincide with the level of artery occlusion, but is located below, which should not mislead the diagnostician. An equally characteristic symptom is a violation of active movements in the joints of the limb, which vary in degree from limitation to complete plegia. In the late stage of severe ischemia, passive movements may also be absent due to stiffness of muscles and joints. Joint contracture is an unfavorable sign indicating the non-viability of the limb. The absence of a pulse in the arteries located distal to the level of blockage is also one of the important symptoms of embolism. With severe swelling of the limb, it is sometimes difficult to determine the pulse. Slow filling of the saphenous veins, or the “groove” symptom, also indicates poor circulation. Sometimes there is increased pulsation in the arteries located proximal to the occlusion, determined by comparative palpation. In advanced cases, severe muscle soreness on palpation, rigidity and subfascial edema are observed. Various classifications have been proposed to assess the severity of limb ischemia. The classification proposed by V.S. Savelyev and co-authors in 1978 most fully meets practical purposes. The diagnosis of great artery embolism is usually made on the basis of physical findings. Additional research methods include ultrasound, radioisotope and X-ray contrast angiography. In this case, the main purpose of their use is to establish the patency of arteries located distal to the occlusion. It should be noted that due to spasm of both main and collateral vessels, the information content of these methods is sharply reduced.
Treatment at the prehospital stage.
Pain relief is achieved by administering drugs or analgesics. An important point is the administration of anticoagulants (10 thousand units of heparin) to prevent continued thrombosis. If necessary, cardiotonic drugs are prescribed. The main method of treatment for embolism of the aorta and peripheral arteries should be surgical, aimed at restoring blood flow in all patients who do not have absolute contraindications to surgery.
Surgery.
The operation of choice is embolectomy. The best results are obtained in the early stages (6-8 hours) after the development of embolism. At later stages, irreversible tissue changes may develop. However, the timing itself does not determine the indications for surgery. Embolectomy can be successfully performed even after several days, if the limb is still viable.
Thrombosis in children
Possible causes of blood clot formation in children:
- thrombophilia - congenital deficiency of anticoagulant blood factors;
- leukemia, other oncological diseases;
- cutaneous fulminant purpura, disseminated intravascular coagulation syndrome (develops with severe intoxication, inflammatory diseases: pancreatitis, peritonitis, etc.);
- the presence of antiphospholipid antibodies, lupus anticoagulant, and other autoantibodies (antibodies to one’s own cells).
Episodes of blood clots in a child should prompt a serious examination to determine the cause.
Risk factors for thrombosis
The following factors increase the likelihood of developing the disease:
- age over 50 years;
- obesity;
- smoking, alcoholism, drug addiction;
- poor nutrition;
- sedentary lifestyle;
- injuries;
- the need for frequent intravenous injections and procedures associated with violation of the integrity of blood vessels (blood sampling, hemodialysis, installation of a venous catheter) increases the risk of developing phlebitis and inflammation of the venous wall.
Prevention measures
Thromboembolism prevention is based on timely detection and treatment of heart and vascular diseases, so we recommend undergoing a comprehensive examination at least once a year.
It is also necessary to lead a healthy and active lifestyle, exercising moderately and adhering to the principles of a healthy diet. The diet should be dominated by foods of plant origin, but it is advisable to exclude foods containing cholesterol.
In the summer, you should avoid dehydration by following a drinking regime. Bad habits, such as smoking, increase the risk of blood clots - give them up.
Symptoms of thrombosis
The clinical manifestations of this pathology vary depending on the location.
Symptoms of venous thrombosis
When a vein is blocked, the outflow of blood is hampered, so the tissues beyond the blockage swell and turn blue. The waste products of cells accumulate, therefore tissue intoxication develops, this is accompanied by pain, impaired sensitivity (the sensation of “crawling goosebumps”). If you do not intervene in time, the tissues begin to die.
Symptoms of venous thrombosis of the lower extremities:
- swelling of the leg, a sharp increase in size, cyanosis;
- cramps of the calf muscles;
- constant pain in the leg, which intensifies when walking;
- increased venous pattern on the thigh.
Cavernous sinus thrombosis:
The dura mater contains channels into which venous blood from the brain drains. Blockage of one of these sinuses, the cavernous sinus, is dangerous because several cranial nerves and the internal carotid artery pass through it. The most common causes of cavernous sinus thrombus formation are inflammatory diseases of the nose, sinuses, facial skin and scalp. Signs:
- headache;
- decreased visual acuity, double vision;
- confusion;
- heat, fever;
- swelling of the eyelids and periocular area;
- pain in the neck when turning or tilting the head;
- impaired facial skin sensitivity.
Among the consequences of such thrombosis: stroke, loss of vision, coma.
Hemorrhoidal thrombosis
Develops against the background of hemorrhoids. Chronic constipation, physical stress, pregnancy and childbirth, and alcohol abuse contribute to it. Signs:
- pain, burning and itching in the anal sphincter area;
- discharge of blood with feces and regardless of the act of defecation;
- prolapse of hemorrhoids.
Retinal vascular thrombosis
The pathology is a typical complication of diabetes mellitus and hypertension, but can also develop for other reasons. Symptoms:
- deterioration of vision, up to complete loss (usually one-sided);
- the appearance of spots, mesh, veils before the eyes.
Symptoms of arterial thrombosis
Blockage of the artery leads to oxygen and energy starvation of tissues, which quickly leads to their death. Arterial forms of the disease are often acute.
Thrombosis of the cerebral arteries
This process leads to necrosis of the area of the brain that the affected artery supplies blood to - ischemic stroke. Signs:
- hemiparesis ー lack of movement in the right or left half of the body (opposite affected area);
- asymmetry of the smile - one corner of the mouth is lowered, does not take part in conversation and smile;
- unclear speech;
- when the patient sticks out his tongue, it deviates to the side.
Thrombosis of the coronary arteries of the heart
Partial blockage of these vessels leads to attacks of angina pain, complete blockage leads to myocardial infarction. Symptoms:
- pressing, burning pain behind the sternum, radiating to the left shoulder blade, arm, shoulder, half of the face and neck;
- dyspnea;
- with angina pectoris, rest and nitroglycerin help, with a heart attack there is no improvement, urgent medical attention is needed.
Pulmonary artery thrombosis
It is a complication of thrombosis of the veins of the lower extremities, endocarditis, myocardial infarction. It develops rapidly and has a high mortality rate. Signs:
- sharp stabbing pain in the chest;
- swelling of the veins of the neck;
- shortness of breath, feeling of lack of air;
- hemoptysis;
- increased heart rate.
Hepatic artery thrombosis
Death (infarction) of liver tissue is a complication of endocarditis, myocardial infarction or liver transplantation and manifests itself as follows:
- severe pain under the right rib;
- nausea, vomiting, bitterness in the mouth;
- yellowness of the skin and whites of the eyes.
Femoral artery thrombosis
This form of pathology is manifested by pain when walking, coldness, and paleness of the limb. The pulse in the popliteal fossa and on the foot is palpable weakly or not detected at all.
Therapeutic tactics
When lesions of the brachiocephalic vessels are detected, specialists traditionally choose conservative treatment tactics. It involves taking certain medications (anticoagulants or antiplatelet agents), vitamin therapy, and diet therapy. The patient is given detailed recommendations regarding lifestyle and nutrition correction. He is obliged to control the level of cholesterol in the blood, as well as monitor the condition and stability of blood pressure.
Surgical intervention as a therapeutic tactic is chosen in conditions of a direct threat of stroke. If there is no immediate risk, the patient is registered and observed.
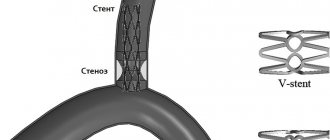
Surgical intervention happens:
- Open (resection of the affected arterial section with its immediate prosthetics or suturing);
- Endovascular (introduction of a stent into a vessel).
The category of open interventions includes endarterectomy (carotid eversion).
Stenting is a more modern, atraumatic and effective method, but it is acceptable and not indicated in every case. The later you seek professional medical help, the less likely you are to be cured using these methods.
Diseases of the brachiocephalic arteries are a serious disorder leading to unpredictable consequences. We urge you to promptly contact vascular surgeons with alarming symptoms in order to avoid the need for aggressive treatment and save your life.
Diagnosis and treatment of thrombosis in Medical
Specialists from the Paracelsus Medical Center will help in diagnosing and eliminating this pathology, provide support during the rehabilitation period, and give recommendations for further prevention.
Our center uses expert-class equipment from leading global manufacturers for diagnosis and treatment. The consultation is conducted by practicing phlebologist surgeons.
On the basis of "Operating Room No. 1" phlebological operations are performed for venous disease. The key advantage of the Paracelsus Medical Center network is highly qualified professional surgeons with extensive practical experience.
Drug treatment
The basis of drug therapy is anticoagulants (thin the blood, prevent the growth of a blood clot), fibrinolytics and thrombolytics (dissolve existing clots), antiatherosclerotic drugs (lower cholesterol levels). If necessary, analgesics, anti-inflammatory drugs, cardiotonic drugs, vitamins, minerals, etc. may be needed as symptomatic therapy.
Surgery
There are such methods of surgical treatment of the disease:
- thrombectomy ー removal of a blood clot;
- stenting (expansion using a frame) and shunting (creating a bypass path for blood flow) for atherosclerotic artery disease;
- arteriovenous shunting.
If the thrombus cannot be removed, a vena cava filter can be installed - the device is placed in the vein above the level of blockage to prevent it from moving and closing the lumen of the vessels of vital organs.
Typical signs and symptoms
The symptoms of diseases of the brachiocephalic arteries are specific. If you feel alarming symptoms, but your doctor, after listening to the complaints, limited himself to pointless diagnoses (CFS, VSD, etc.), be sure to insist on an expanded diagnosis.
Symptoms of diseases of the brachiocephalic arteries include:
- General fatigue, weakness, decreased performance and concentration;
- Sharp headaches that occur when moving the head;
- Dizziness and syncope (short-term loss of consciousness);
- Fainting with low blood pressure;
- Noise or ringing in the ears;
- Transient paresis of the head and limbs;
- Visual disturbances (appearance of spots and flies in the field of vision, decrease in visual acuity with sudden recovery);
- Angina pectoris;
- Ischemia (sometimes asymptomatic);
- Itching, numbness, tingling in the left extremities;
- Swaying when walking;
- Nausea;
- Rare or frequent disorders of motor or speech functions (numbness, inability to communicate clearly).
The insidiousness of atherosclerosis of the brachiocephalic arteries lies in its “blurred” early course. The listed signs sometimes do not make themselves felt at all, or are expressed so weakly that the patient does not attach due importance to them. Ignoring diagnosis and treatment leads to death or a vegetative state.