PHYSIOLOGICAL PROPERTIES OF CARDIAC MUSCLE
The cardiac muscle, like any other muscle, has a number of physiological properties: excitability, conductivity, contractility, refractoriness and automaticity.
· Excitability is the ability of cardiomyocytes and the entire cardiac muscle to be excited when exposed to mechanical, chemical, electrical and other stimuli, which is used in cases of sudden cardiac arrest. A feature of the excitability of the heart muscle is that it obeys the “all or nothing” law. This means that the cardiac muscle does not respond to a weak, sub-threshold stimulus (i.e., it is not excited and does not contract) (“nothing”), but to a stimulus of a threshold force sufficient to excite the cardiac muscle it reacts with its maximum contraction (“all ") and with a further increase in the strength of irritation, the response from the heart does not change. This is due to the structural features of the myocardium and the rapid spread of excitation along it through intercalary discs - nexuses and anastomoses of muscle fibers. Thus, the strength of heart contractions, unlike skeletal muscles, does not depend on the strength of stimulation. However, this law, discovered by Bowditch, is largely conditional, since the manifestation of this phenomenon is influenced by certain conditions - temperature, degree of fatigue, muscle extensibility and a number of other factors.
It is worth adding that it is applicable only in relation to the effect of an artificial stimulus on the heart. Bowditch, in an experiment with an excised strip of myocardium, discovered that if it is rhythmically stimulated by electrical impulses of equal strength, then the muscle will respond to each subsequent stimulation with a large contraction up to its maximum value. This phenomenon is called the “Bowditch ladder.”
· Conduction is the ability of the heart to conduct excitation. The speed of excitation in the working myocardium of different parts of the heart is not the same. Excitation propagates through the atrial myocardium at a speed of 0.8-1 m/s, and through the ventricular myocardium at a speed of 0.8-0.9 m/s. In the atrioventricular region, in an area 1 mm long and wide, the conduction of excitation slows down to 0.02-0.05 m/s, which is almost 20-50 times slower than in the atria. As a result of this delay, ventricular excitation begins 0.12-0.18 s later than the onset of atrial excitation. There are several hypotheses explaining the mechanism of atrioventricular delay, but this issue requires further study. However, this delay has great biological meaning - it ensures coordinated functioning of the atria and ventricles.
· Refractoriness is a state of inexcitability of the heart muscle. The degree of excitability of the heart muscle changes during the cardiac cycle. During excitement, she loses the ability to respond to a new impulse of irritation. This state of complete inexcitability of the heart muscle is called absolute refractoriness and takes up almost the entire systole. After the end of absolute refractoriness at the beginning of diastole, excitability gradually returns to normal - relative refractoriness. At this time (in the middle or at the end of diastole), the heart muscle is able to respond to stronger stimulation with an extraordinary contraction - an extrasystole. After the ventricular extrasystole, when an extraordinary impulse originates in the atrioventricular node, an extended (compensatory) pause occurs (Fig. 9.).
Rice. 9. Extrasystole a and extended pause b
It occurs as a result of the fact that the next impulse that comes from the sinus node arrives at the ventricles during their absolute refractoriness caused by extrasystole and this impulse or one heartbeat falls out. After a compensatory pause, the normal rhythm of heart contractions is restored. If an additional impulse occurs in the sinoatrial node, then an extraordinary cardiac cycle occurs, but without a compensatory pause. The pause in these cases will be even shorter than usual. After the period of relative refractoriness, a state of increased excitability of the heart muscle (exaltation period) occurs when the muscle is excited by a weak stimulus. The refractory period of the heart muscle lasts longer than in skeletal muscles, so the heart muscle is not capable of long-term titanic contraction.
Sometimes pathological modes of propagation of excitation are observed, in which the atria and ventricles are excited spontaneously with a high frequency and contract non-simultaneously. If these excitations are periodic, then such an arrhythmia is called flutter, if they are non-rhythmic - flicker. Both flutter and ventricular fibrillation cause the greatest danger to life.
· Contractility. The contractility of the heart muscle has its own characteristics. The strength of heart contractions depends on the initial length of muscle fibers (Frank-Starling law). The more blood flows to the heart, the more its fibers will be stretched and the greater the force of heart contractions. This has great adaptive significance, ensuring a more complete emptying of the cavities of the heart from blood, which maintains a balance in the amount of blood flowing to the heart and flowing from it. A healthy heart, even with a slight stretch, responds with an increased contraction, while a weak heart, even with a significant stretch, only slightly increases the force of its contraction, and the outflow of blood is carried out due to an increase in the rhythm of heart contractions. In addition, if for some reason there is excessive stretching of the cardiac fibers beyond physiologically permissible limits, then the force of subsequent contractions no longer increases, but weakens.
The strength and frequency of heart contractions also changes under the influence of various neurohumoral factors without changing the length of muscle fibers.
The peculiarity of the contractile activity of the myocardium is that calcium is required to maintain this ability. In a calcium-free environment, the heart does not contract. Energy suppliers for heart contractions are high-energy compounds (ATP and CP). In cardiac muscle, energy (unlike skeletal muscles) is released mainly in the aerobic phase, therefore the mechanical activity of the myocardium is linearly related to the rate of oxygen absorption. With a lack of oxygen (hypoxemia), anaerobic energy processes are activated, but they only partially compensate for the missing energy. Lack of oxygen also negatively affects the content of ATP and CP in the myocardium.
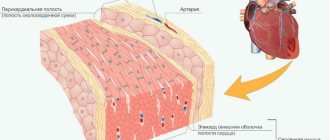
In the cardiac muscle, there is so-called atypical tissue, which forms the conduction system of the heart (Fig. 10.).
This tissue has thinner myofibrils with less cross-striation. Atypical myocytes are richer in sarcoplasm. The tissue of the conduction system of the heart is more excitable and has a pronounced ability to conduct excitation. In some places, the myocytes of this tissue form clusters or nodes. The first node is located under the epicardium in the wall of the right atrium, near the confluence of the vena cava - the sinoatrial node.
Rice. 10. Conducting system of the heart:
a - sinoatrial node; b — atrioventricular node; c — bundle of His; d - Purkinje fibers.
The second node is located under the epicardium of the wall of the right atrium in the area of the atrioventricular septum, separating the right atrium from the ventricle, and is called the atrioventricular (atrioventricular) node. The bundle of His departs from it, dividing into the right and left branches, which separately go to the corresponding ventricles, where they break up into Purkinje fibers. The conduction system of the heart is directly related to the automaticity of the heart.
Automaticity of the heart is the ability to contract rhythmically under the influence of impulses originating in the heart itself without any irritation. The automaticity of the heart can be observed on the heart of a frog removed and placed in Ringer's solution. The phenomenon of cardiac automaticity has been known for a very long time. It was observed by Aristotle, Harvey, Leonardo Da Vinci.
For a long time, there were two theories to explain the nature of automation - neurogenic and myogenic. Representatives of the first theory believed that automation was based on the nervous structures of the heart, and representatives of the second theory associated automation with the ability of muscle elements to perform it.
Views on automaticity received new directions in connection with the discovery of the conduction system of the heart. Currently, the ability to automatically generate impulses is currently associated with special β-cells that are part of the sinoatrial node. Numerous and varied experiments (Stannius - by the method of applying ligatures, Gaskell - by limited cooling and heating of different parts of the heart), then by studies with the registration of electrical potentials, it was proved that the main center of first-order automaticity, sensor, driver (pacemaker) of the heart rate is the sinoatrial node , since in the P-cells of this node the highest rate of diastolic depolarization and generation of action potential associated with a change in the ionic permeability of cell membranes is noted.
As one moves away from this node, the ability of the cardiac conduction system to operate automatically decreases (the law of the gradient of decreasing automaticity, discovered by Gaskell). Based on this law, the atrioventricular node has less ability for automation (second-order center of automation), and the rest of the conduction system is a third-order center of automation.
Under normal conditions, only the automaticity of the sinoatrial node functions, and the automaticity of other departments is suppressed by the higher frequency of its excitations. This was proven by Stannius by applying ligatures to different parts of the frog's heart. So, if the first ligature is applied to a frog, separating the venous sinus from the atria, then the heart contractions will temporarily stop. Then, after some time or immediately after applying the second ligature to the atrioventricular node, contractions of the atria or ventricle will begin (depending on how the ligature is placed and where the node goes), but in all cases these contractions will have a rarer rhythm due to the lower ability to automation of the atrioventricular node.
Thus, the impulses that cause contractions of the heart initially originate in the sinoatrial node. Excitation from it spreads through the atria and reaches the atrioventricular node, then through it along the His bundle to the ventricles. In this case, excitation from the sinoatrial node to the atrioventricular node is transmitted through the atria not radially, as was previously thought, but along the most favorable, preferred path, i.e. cells very similar to Purkinje cells.
The fibers of the conduction system of the heart, with their numerous branches, are connected to the fibers of the working myocardium. In the area of their contact, there is a delay in the transfer of excitation of 30 ms, which has a certain functional significance. A single impulse, arriving earlier than others along a separate fiber of the conduction system, may not pass to the working myocardium at all, and when several impulses arrive simultaneously, they are summed up, which facilitates their transition to the myocardium.