The cardiac muscle (myocardium) in the structure of the human heart is located in the middle layer between the endocardium and epicardium. It is this that ensures the uninterrupted operation of “distilling” oxygenated blood into all organs and systems of the body.
Any weakness affects blood flow and requires compensatory restructuring and coordinated functioning of the blood supply system. Insufficient ability to adapt causes a critical decrease in the performance of the heart muscle and its diseases. The endurance of the myocardium is ensured by its anatomical structure and endowed capabilities.
Features of muscle tissue are:
- striated striations formed by myofibrils of cardiomyocyte cells;
- the presence of two types of fibers: thin (actin) and thick (myosin), connected by cross bridges;
- the connection of myofibrils into bundles of different lengths and directions, which makes it possible to distinguish three layers (superficial, internal and middle).
The structure of the heart muscle is different from skeletal and smooth muscle muscles, which provide movement and protection of internal organs
The morphological features of the structure provide a complex mechanism of heart contraction.
How does the heart contract?
Contractility is one of the properties of the myocardium, which consists in creating rhythmic movements of the atria and ventricles, allowing blood to be pumped into the vessels. The chambers of the heart constantly pass through 2 phases:
- Systole - is caused by the combination of actin and myosin under the influence of ATP energy and the release of potassium ions from the cells, while thin fibers slide over thick ones and the bundles decrease in length. The possibility of wave-like movements has been proven.
- Diastole - relaxation and separation of actin and myosin occurs, restoration of expended energy due to the synthesis of enzymes, hormones, and vitamins obtained through the “bridges”.
It has been established that the force of contraction is provided by calcium entering the myocytes.
The entire cycle of heart contraction, including systole, diastole and the general pause after them, with a normal rhythm fits into 0.8 seconds. Begins with atrial systole, the ventricles are filled with blood. Then the atria “rest”, moving into the diastole phase, and the ventricles contract (systole). Calculating the time of “work” and “rest” of the heart muscle showed that per day the state of contraction accounts for 9 hours 24 minutes, and the state of relaxation accounts for 14 hours 36 minutes.
The sequence of contractions, ensuring the physiological characteristics and needs of the body during stress and anxiety depend on the connection of the myocardium with the nervous and endocrine systems, the ability to receive and “decipher” signals, and actively adapt to human living conditions.
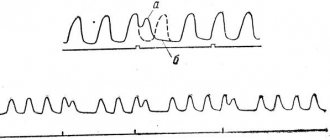
The spread of excitation from the sinus node can be traced by intervals and ECG waves
Atypical fibers.
Thanks to atypical nerve fibers, heart automation is realized.
Automaticity of the heart is the ability of the heart to contract rhythmically under the influence of impulses originating in itself.
Atypical cardiac fibers serve as the morphological substrate of automation. – pacemakers capable of periodic self-generation of membrane potential.
Atypical myocytes are larger than working ones; they contain more sarcoplasm with a high glycogen content, but few myofibrils and mitochondria. In atypical cells, enzymes that promote anaerobic glycolysis predominate.
The atypical cells themselves are located in strictly defined areas and form the sinatrial (Keith-Flerk) and atrioventricular (Aschoff-Tavara) nodes and the bundle of His, dividing into legs that branch like Purkinje fibers.
Diagram of the conduction system of the heart:
Typical myocytes maintain a stable membrane potential during contraction, while the potential of atypical myocytes of the synatrial node slowly decreases due to increased membrane permeability for sodium ions entering the fibers and potassium ions leaving them. When the sodium gate opens, Na+ ions rush into the fibers like an avalanche, causing the propagation of a new potential. (“drift” of potential). After which the process is repeated.
The ability for automaticity in different parts of the heart is not the same and in the atrioventricular node it is already lower, and in the Hiss bundle it is so small that the corresponding frequency of occurrence of the membrane potential is not compatible with life.
Cardiac mechanisms that provide contraction
The properties of the heart muscle have the following purposes:
- support myofibril contraction;
- ensure the correct rhythm for optimal filling of the cavities of the heart;
- maintain the ability to push blood through any extreme conditions for the body.
For this, the myocardium has the following abilities.
Excitability - the ability of myocytes to respond to any incoming pathogens. Cells protect themselves from above-threshold stimulation by a state of refractoriness (loss of the ability to excite). In a normal contraction cycle, a distinction is made between absolute and relative refractoriness.
- During the period of absolute refractoriness, for 200 to 300 msec, the myocardium does not respond even to extremely strong stimuli.
- When relative, it is able to respond only to sufficiently strong signals.
This property prevents the heart muscle from “distracting” the contraction mechanism during the systole phase
Conductivity is the property of receiving and transmitting impulses to different parts of the heart. It is provided by a special type of myocytes that have processes very similar to neurons in the brain.
Automaticity - the ability to create its own action potential inside the myocardium and cause contractions even when isolated from the body. This property allows resuscitation in emergency cases and maintains blood supply to the brain. The importance of the located network of cells and their accumulation in nodes during transplantation of a donor heart.
Pacemaker cells (pacemakers) become the main ones if the processes of repolarization and depolarization in the main nodes are weakened. They suppress “other people’s” excitability and impulses, and try to take on a leadership role. Localized in all parts of the heart. The possibilities are restrained by the sufficient strength of the sinus node.
The importance of biochemical processes in the myocardium
The viability of cardiomyocytes is ensured by the supply of nutrients, oxygen and the synthesis of energy in the form of adenosine triphosphoric acid.
All biochemical reactions occur maximally during systole. The processes are called aerobic because they are possible only with a sufficient amount of oxygen. The left ventricle consumes 2 ml of oxygen per minute per 100 g of mass.
To produce energy, the following are used in the blood:
- glucose,
- lactic acid,
- ketone bodies,
- fatty acid,
- pyruvic and amino acids,
- enzymes,
- B vitamins,
- hormones.
If the heart rate increases (physical activity, anxiety), the need for oxygen increases 40–50 times, and the consumption of biochemical components also increases significantly.
What compensatory mechanisms does the heart muscle have?
A person does not develop pathology as long as the compensation mechanisms work well. Regulation is carried out by the neuroendocrine system.
The sympathetic nerve delivers signals to the myocardium about the need for increased contractions. This is achieved by more intense metabolism and increased ATP synthesis.
A similar effect occurs with increased synthesis of catecholamines (adrenaline, norepinephrine). In such cases, increased work of the myocardium requires an increased supply of oxygen.
If atherosclerotic narrowing of the coronary vessels does not allow the heart muscle to be supplied in the required volume, then the mediator acetylcholine is released. It protects the myocardium and helps maintain contractile activity in conditions of oxygen deficiency.
The vagus nerve helps reduce the frequency of contractions during sleep, during rest periods, and preserve oxygen reserves.
It is important to consider reflex adaptation mechanisms.
Tachycardia is caused by congestive stretching of the mouths of the vena cava.
Reflex slowing of the rhythm is possible with aortic stenosis. In this case, increased pressure in the cavity of the left ventricle irritates the endings of the vagus nerve, contributing to bradycardia and hypotension.
The duration of diastole increases. Favorable conditions are created for the functioning of the heart. Therefore, aortic stenosis is considered a well-compensated defect. It allows patients to live to an old age.
Circulation circles
In the process of evolution, animals have two circles of blood circulation, which are divided into large and small circles.
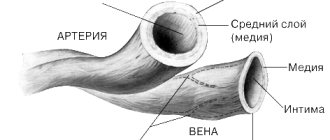
The great circle begins in the left ventricle; when it contracts, blood from the heart enters the aorta, from which the blood passes into arteries of various sizes, which subsequently break up into arterioles and capillaries in the tissues of the body. In capillaries, exchange occurs between blood and adjacent tissues. Then the blood collects in venules, from where it merges into the veins, and through the veins it enters the vena cava and the right atrium, where the path of the systemic circulation ends.
From the right atrium, blood is transfused into the right ventricle, from which the pulmonary circulation begins. The right ventricle pushes blood into the pulmonary artery, which, dividing into smaller vessels, branches into a network of capillaries in the lungs, where the blood is saturated with oxygen and releases bound carbon dioxide. After gas exchange, the blood collects in the pulmonary veins and flows into the left atrium, where the pulmonary circulation ends.
The separation of blood circulation contributed to increased pressure in the arteries and, as a result, more intense metabolism.
How to treat hypertrophy?
Typically, prolonged increased load causes hypertrophy. The thickness of the left ventricular wall increases by more than 15 mm. An important point in the formation mechanism is the lag in the growth of capillaries deep into the muscle. In a healthy heart, the number of capillaries per mm2 of cardiac muscle tissue is about 4000, and with hypertrophy the figure decreases to 2400.
Therefore, the condition is considered compensatory up to a certain point, but with significant thickening of the wall it leads to pathology. It usually develops in the part of the heart that must work hard to push blood through a narrowed hole or overcome a vascular obstruction.
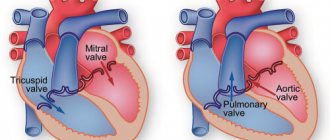
Hypertrophied muscle is able to maintain blood flow for a long time in case of heart defects.
The muscle of the right ventricle is less developed; it works against a pressure of 15–25 mm Hg. Art. Therefore, compensation for mitral stenosis and cor pulmonale does not last long. But right ventricular hypertrophy is of great importance in acute myocardial infarction, cardiac aneurysm in the left ventricular area, and relieves overload. The significant capabilities of the right sections in training during physical exercises have been proven.
Thickening of the left ventricle compensates for aortic valve defects and mitral insufficiency
The structure of the myocardium of the heart
The heart as an organ consists of three membranes: the endocardium, the deepest membrane represented by a connective tissue membrane covered with endothelium, the myocardium - the muscular membrane of the heart and the epicardium - the outer serous membrane of the heart.
The myocardium is built from cardiac striated muscle tissue and has a number of features associated with the function of the heart itself, both as a whole and its parts: - In different parts, the thickness of the heart muscle is not the same, for example, in the left ventricle the wall is thicker than in the right. - The muscles of the atrium are separate from the muscles of the ventricles. — In the ventricles and atria there are common muscle layers. — In the area of the venous mouths of the vestibules there are sphincters. — The presence of two morphofunctional types of muscle fibers in the myocardium.
Under microscopy, cardiac muscle appears similar to skeletal striated muscle. A clearly defined cross-striation and sarcomeric structure are observed.
There are two types of cardiac fibers: 1) typical fibers - the working myocardium, 2) atypical fibers of the conduction system.
Typical fibers:
The working myocardium consists of a chain of muscle cells - sarcomeres connected to each other “end to end” and enclosed in a common sarcoplasmic membrane. United sarcomeres form myofibrils. The contact of sarcomeres is carried out through intercalary disks, due to which the fibers have a characteristic cross-striation.
Structure of sarcomeres:
Sarcomeres consist of alternating dark (myosin) - A, and light (actin) - I stripes. In the center of strip A there is zone H, which has a central T-line. Sarcomeres are connected to each other using intercalary discs - nexuses, which are the true boundaries of cells.
Myosin contained in band A is capable of breaking down ATP to ADP, that is, it is an adenosine triphosphatase, and is also capable of forming a reversible actomyosin complex with myosin (in the presence of Ca++ and the formation of ADP), which is responsible for the contractility of the heart muscle.
Can the heart adapt to work in hypoxic conditions?
An important property of adaptation to work without sufficient oxygen supply is the anaerobic (oxygen-free) process of energy synthesis. A very rare occurrence for human organs. Turns on only in emergency situations. Allows the heart muscle to continue contracting. Negative consequences are the accumulation of breakdown products and overwork of muscle fibrils. One cardiac cycle is not enough for energy resynthesis.
However, another mechanism is involved: tissue hypoxia reflexively causes the adrenal glands to produce more aldosterone. This hormone:
- increases the amount of circulating blood;
- stimulates an increase in the content of red blood cells and hemoglobin;
- increases venous flow to the right atrium.
This means that it allows the body and myocardium to adapt to the lack of oxygen.
Cardiac cycle.
The work of the heart can be divided into several phases (periods):
Tension - systole,
expulsions of blood,
Relaxation - diastole.
The cardiac cycle is the coordinated alternation of systole and diastole of the heart.
The beginning of the cardiac cycle is considered to be atrial systole (and the left one contracts slightly earlier than the right one); when the atria contract, the pressure in them increases, and blood flows into the ventricles of the heart. Blood does not flow into the veins, since at the moment of atrial systole the lumen of the veins is narrowed, and blood flows freely into the ventricles, since the ventricles are relaxed and the atrioventricular valves are free. Cycle time 0.1 s.
The next stage of the cycle is ventricular systole. When they contract, the pressure increases and the blood, trying to flow out, slams the atrioventricular valves and rushes into the lumen of the arteries, opening the semilunar valves. Cycle time 0.4 s.
After the opening of the semilunar valves, the pressure in the ventricles drops, and in the arteries it increases sharply, the semilunar valves slam shut, and ventricular diastole occurs.
How myocardial pathology occurs, mechanisms of clinical manifestations
Myocardial diseases develop under the influence of various causes, but appear only when adaptation mechanisms fail.
Long-term loss of muscle energy, the impossibility of independent synthesis in the absence of components (especially oxygen, vitamins, glucose, amino acids) lead to a thinning of the actomyosin layer, breaking the connections between myofibrils, replacing them with fibrous tissue.
This disease is called dystrophy. It accompanies:
- anemia,
- avitaminosis,
- endocrine disorders,
- intoxications.
Arises as a consequence:
- hypertension,
- coronary atherosclerosis,
- myocarditis.
Patients experience the following symptoms:
- weakness,
- arrhythmia,
- shortness of breath during physical exertion,
- heartbeat.
At a young age, the most common cause may be thyrotoxicosis and diabetes mellitus. In this case, there are no obvious symptoms of an enlarged thyroid gland.
The inflammation of the heart muscle is called myocarditis. It accompanies both infectious diseases of children and adults, as well as those unrelated to infection (allergic, idiopathic).
It develops in focal and diffuse forms. Proliferation of inflammatory elements affects myofibrils, interrupts pathways, and changes the activity of nodes and individual cells.
We advise you to learn more about inflammatory diseases of the myocardium from this article
As a result, the patient develops heart failure (usually right ventricular failure). Clinical manifestations consist of:
- pain in the heart area;
- rhythm interruptions;
- shortness of breath;
- dilation and pulsation of the neck veins.
Atrioventricular blocks of varying degrees are recorded on the ECG.
The most well-known disease caused by impaired blood flow to the heart muscle is myocardial ischemia. It proceeds in the form:
- angina attacks,
- acute heart attack,
- chronic coronary insufficiency,
- sudden death.
The main morphological substrate for this pathology are areas of the heart muscle depleted of nutrients and oxygen. Depending on the degree of damage, cardiomyocytes change and undergo necrosis.
All forms of ischemia are accompanied by paroxysmal pain. They are figuratively called “the cry of the starving myocardium.” The course and outcome of the disease depends on:
- speed of assistance;
- restoration of blood circulation due to collaterals;
- the ability of muscle cells to adapt to hypoxia;
- formation of a strong scar.
A controversial drug included in the doping list for providing additional energy to the heart muscle