Adolescence is a period of hormonal changes and active growth, and therefore teenagers cannot always sort out their feelings on their own. Because of this, you may miss symptoms that indicate the presence of serious diseases, including heart disease.
The best cardiologists in Rostov-on-Don do not recommend making diagnoses based solely on symptoms, but it is important to know what can signal a malfunction of the heart muscle in order to contact a specialist in time.
Heart diseases
All nosologies in pediatric cardiology are divided into several large groups:
- Congenital heart defects. These are anomalies in the development of the heart, its valves and great (main) vessels that occur in the 2-8th week of intrauterine development. These include defects of the interventricular, interatrial and/or aortopulmonary septa, open atrioventricular canal, ductus arteriosus, stenosis (narrowing) or insufficiency (incomplete closure of the leaflets) of valves, incorrect location of vessels or pathological collaterals between them (connections), absence of an atrium or ventricle, etc. .
- Valvular heart defects. These are acquired pathologies of the valve apparatus - stenosis (narrowing) or insufficiency.
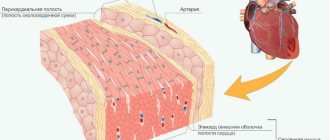
- Diseases of the endocardium - the inner lining of the heart.
- Diseases of the myocardium - the middle (muscular) layer of the heart.
- Pathologies of the pericardium - the cardiac connective tissue sac.
- Pathologies of coronary circulation. This group includes myocardial infarction, Kawasaki disease (vasculitis of medium and small arteries) and anomalies of the origin and number of coronary arteries.
- Pulmonary hypertension. This is an overload of blood in the pulmonary arteries due to increased pressure in the pulmonary arteries.
- Heart damage due to hereditary diseases. They are the result of errors in the genetic code of the parents' germ cells; these mutations are passed on to the offspring. They can appear from birth or already in adulthood.
- Heart tumors.
- Vascular damage. Most often we are talking about arterial hypertension (increased blood pressure) or hypotension (lowered blood pressure).
- Heart rhythm disturbances are disturbances in the regularity and sequence of heart contractions. If the heart muscle is damaged, its course is distorted, which leads to an abnormal rhythm of heart contraction.
- Heart failure is a syndrome caused by decompensated dysfunction of the myocardium. That is, the heart is so affected that it is no longer able to provide the necessary blood output and supply blood to all organs.
It is important to clarify that heart disease rarely occurs in isolation. One pathology progresses and leads to another. Thus, aortic stenosis will lead to pulmonary hypertension, and infective endocarditis destroys the valves, resulting in defects. After myocardial infarction or inflammation (myocarditis), the conduction of impulses through the affected area is disrupted, and as a result, the normal rhythm of contractions is disrupted.
Reasons for development
The key cause of the disease, which is called myocardial infarction, is considered to be the formation of a blood clot. Typically, a blood clot forms inside a coronary artery that is already narrowed due to atherosclerosis, a condition in which fatty deposits (or atherosclerotic plaques) accumulate along the inner walls of blood vessels.
Throughout life, fat, calcium, proteins and inflammatory cells accumulate in the arteries, forming atherosclerotic plaques. These deposits are hard on the outside but soft and crumbly on the inside. When the plaque hardens, the outer shell cracks. This is called plaque rupture. Platelets (plates in the blood that help it clot) become trapped in the area, and blood clots form around the plaque. If a blood clot blocks an artery, the heart muscle is starved of oxygen. The muscle cells soon die, causing permanent damage. This is the most common reason, but not the only one.
Slowing of blood flow in the coronary artery can occur when the heart beats very quickly or a person has low blood pressure. If oxygen demand exceeds supply, a heart attack can occur without a blood clot forming. People with atherosclerosis also often suffer from this type of heart attack. Source: Myocardial infarction. Zhmurov D.V., Parfenteva M.A., Semenova Yu.V. Colloquium-journal, 2021. p. 56-61.
In rare cases, coronary artery spasm can also cause a heart attack. During this coronary spasm, your arteries narrow or spasm, cutting off the blood supply to the heart muscle (ischemia). This can happen at rest or under stress, even if the person does not have serious coronary heart disease.
If vascular patency is not restored, there is a risk that recurrent myocardial infarction will develop over time. It will cause even more damage to the heart.
Etiology
The causes of heart problems in children are conventionally divided into large subgroups. Let's look at each one separately.
Mother's side
If during pregnancy a woman has suffered from rubella, systemic lupus erythematosus, syphilis, toxoplasmosis, if she has diabetes mellitus or other chronic diseases, then all this is reflected in the fetus.
The list of approved drugs for pregnant women is strictly limited; most antibiotics, warfarin and other drugs (they are called teratogenic) are too toxic for the fetus. Taking them increases the risk of spontaneous abortion (miscarriage) or various abnormalities in the development of the child.
Drinking alcohol, smoking and using drugs during pregnancy also leads to congenital pathologies in children.
Genetic disorders
Most often these are chromosomal abnormalities. But genetic predisposition and mutations are not considered the only cause of cardiac pathologies. In 90% of cases, the cause of heart problems is multifactorial.
Bad habits
We have already talked about how the state of the mother’s body affects children. But the risk factors for developing heart problems in children are similar to those in adults:
- Smoking;
- Alcohol;
- Sedentary lifestyle;
- Narcotic substances;
- Stress;
- Infections;
- High cholesterol levels.
This list is more relevant for teenagers 14-17 years old than for kids. However, we must understand that nicotine and ethanol metabolism products destroy the myocardium and vascular wall in a child in the same way as in an adult. “Pampering” behind garages can result in a heart attack at age 30.
Statistics show that over the last decade the percentage of children with excess body weight has increased, which also negatively affects the heart. Myocardial infarction, due to obesity and other risk factors, has become “younger” and is already occurring in girls and boys aged 20-30 years, which was considered casuistry back in the 2000s.
Heart attack in a teenager: risk factors
Heart disease is believed to be common in older people. However, recently there have been cases where such problems become the cause of death of young people - in physical education lessons, competitions, and so on. Cardiologist, National Medical Research Center named after. ak. Meshalkina Marina Novikova told what parents need to know in order to prevent a tragedy.
Heart attack is not a diagnosis
Typically, a heart attack refers to myocardial infarction. This condition develops when the blood flow in the vessels supplying the heart muscle is disrupted - for example, due to a sharp spasm or blockage of the vessels by a blood clot or accumulation of cholesterol. From a lack of oxygen, a section of the heart muscle begins to die. This causes chest pain and cardiac dysfunction. Fortunately, myocardial infarction in children and adolescents is extremely rare.
Symptoms include chest pain that can be described as tight, heavy and squeezing.
The pain is accompanied by weakness, nausea, shortness of breath, sweating, dizziness or fainting, radiating to the shoulders, arms, neck or jaw. The attack is accompanied by a feeling of despair and doom, and the pain intensifies within 15–20 minutes.
With such symptoms, it is necessary to urgently call an ambulance. Especially if the victim has one or more risk factors for developing heart disease: a history of heart attacks in the family, smoking, obesity, a sedentary lifestyle, high blood cholesterol, diabetes.
Take action
But even if the situation is not critical, the child’s complaints of pain in the heart area cannot be ignored. The first thing to do is consult a pediatrician. There can be many reasons. The pediatrician will already determine the tactics and management strategy. It is important to stop any physical activity before seeing a doctor! The circle of required specialists can be numerous and is determined individually. It may be necessary to be examined by a cardiologist, arrhythmologist, endocrinologist, geneticist, orthopedist and other specialists. After the examination, the doctor will determine the tactics.
Non-hereditary risk factors for heart disease in adolescents
The level of C-reactive protein increases in the blood of adolescents who regularly experience stress, which increases the risk of chronic diseases of the cardiovascular system.
So, a study was conducted. Dr. Andrew Fuligni of the University of California, Los Angeles, and his colleagues from 69 high schools across the state spent two weeks identifying students who were caught in the crossfire of negative interpersonal interactions: conflicts with family, bullying from peers, reprimands from teachers.
Eight months later, the researchers measured C-reactive protein levels in the blood plasma. This substance is considered a marker of system-wide inflammation, which increases the risk of developing cardiovascular diseases in adults. As a result, doctors came to the conclusion that as the frequency of daily stressful episodes associated with other people increases, the level of C-reactive protein also increases.
In their report in the journal Psychosomatic Medicine, Andrew Fuligni and his colleagues suggest conducting more studies aimed at testing young adolescents and preschoolers. In addition, doctors say it is necessary to find out whether different coping skills can mitigate the production of inflammatory markers in young people.
In addition to stress, the risk of developing myocardial infarction is increased by heart defects - organic (persistent) lesions of the valve apparatus, both congenital and acquired.
Acquired heart defects occur due to damage to the endocardium (the inner lining of the heart). In the vast majority of cases, these defects are of rheumatic origin.
Organic lesions of the valve apparatus in children develop, most often, in the form of damage to the bicuspid valve (bicuspid valve insufficiency), which regulates blood flow in the left atrioventricular orifice.
Hereditary risk factors
Hereditary factors include congenital heart and vascular defects, which can manifest as heart attacks, and the older the child, the greater the likelihood of such “typical” complaints. Also these are heart rhythm disorders - disturbances in the conduction and blockage of the heart and hereditary hypercholesterolemia (FH) - a genetic disease that leads to the early onset of heart disease.
If hereditary hypercholesterolemia is left untreated, the risk of developing cardiovascular diseases at an early age increases 100 times. In the largest study to date, more than 10,000 one-year-olds were tested for high cholesterol and genetic mutations. One child in every 270 children tested positive for FH. During examination, their parents also had a positive FH test. Therefore, it is important to know your heredity, notes Marina Albertovna.
A recent study found that checking young children for high cholesterol while receiving mandatory vaccinations could prevent hundreds of heart attacks in teenagers.
After selecting children with a high likelihood of developing heart disease, the possibility of using measures to lower cholesterol levels, sets of exercises to strengthen the heart, quitting smoking, maintaining a diet, and at an older age - taking medications to stabilize them follows. For example, screening for cholesterol in some countries is recommended along with preventive vaccinations.
When should you be vigilant?
To reduce the risk of developing chronic cardiovascular disease in a child, it is important for parents to know the family tree in terms of the presence of hereditary diseases, undergo routine examinations with a pediatrician and follow his recommendations.
After consulting a pediatrician, if indicated, the circle of specialists whose consultations are necessary is determined, and an examination plan is formed.
At risk are patients with a hereditary factor, overweight, and leading a sedentary lifestyle. In addition, the modern rhythm of life is often itself a risk factor.
Thus, excess body weight and physical inactivity significantly increases the risk of developing cardiovascular diseases in adolescents. The vast majority of adolescents diagnosed with obesity cannot get rid of this disease at a later age. Therefore, it is necessary to change their eating behavior as early as possible.
Scientists have previously suggested that obese teenagers are at greater risk of early death from heart attack or stroke, just as adults. A new study has given a more precise answer to the question of how fat a teenager should be when faced with a similar problem.
According to the electronic journal “Health Bulletin”, during a scientific investigation by Israeli specialists it was found that the following correlation operates: the higher the BMI of a teenager, the greater the risk of early death.
Note that scientists calculated the BMI of 2.3 million young people aged 17 years. While the project lasted, several tens of thousands (32,127) deaths were recorded among those observed, including those due to cardiovascular disorders, coronary heart disease, and strokes. Several hundred cases were of so-called sudden death.
It is also important that parents of children involved in sports should be vigilant and keep in mind that only a sports medicine doctor can give a medical certificate on admission.
Symptoms
A child who has heart problems may complain of:
- Chest pain (in the area of the heart, possibly radiating to the arm, hypochondrium, or armpit);
- Shortness of breath;
- Rapid heartbeat or noticeable pauses;
- Interruptions in heart function;
- Dizziness;
- Darkening of the eyes and fainting;
- Paleness or cyanosis (bluish coloration of the skin and mucous membranes);
- Acceleration of the pulse or its difference in the hands;
- Poor appetite and short stature;
- Frequent respiratory infections;
- Swelling and pulsation of neck vessels;
- High or low blood pressure;
- Chest deformation, etc.
Symptoms usually begin or worsen after exercise. At first, the child usually does not attach any importance to this, then his endurance begins to suffer, and his condition worsens, which becomes the reason for contacting a cardiologist.
How to understand what exactly hurts in a child’s chest
First of all, this is not just a whim, but crying, screaming and even hysteria. At this time, the child can clench his fists and pull them to the chest, or he can simply hit himself in this area. Additional symptoms include:
- shortness of breath;
- cardiopalmus;
- difficulty breathing or swallowing;
- less often elevated temperature.
Since there is strong pain in this area, the baby rarely turns over on his stomach, but will lie on his back or side, although he previously loved this position.
The key symptom of compressive pain is a sudden change in mood, and in addition, the child shrinks, taking the fetal position, thus helping himself to cope with such severe pain at the level of instincts. Sometimes sharp redness of the whites of the eyes, red spots on the body in the chest area and face are noticeable.
Pressing pain can make itself felt progressively. One moment everything is fine, the next it’s hard to breathe. In order to exclude all possible causes, and in case of diagnosis and treatment, return to its former healthy state, it is necessary to regularly visit a pediatric cardiologist in Saratov. The first dose is appropriate at the age of 1–2 months, and then every six months, if there are no visible pain syndromes.
Complications
If you have cardiac problems, medical supervision is always necessary. In the youngest patients, the pathology may disappear on its own, but this is a rare occurrence. Teenagers during puberty are often worried about arrhythmia or tachycardia (increased heart rate) - this is the price to pay for hormonal changes; in most cases, everything returns to normal on its own.
Despite the presence of happy outcomes, if a child has heart complaints, you should urgently consult a cardiologist.
Otherwise, complications may arise:
- Secondary arterial hypertension (in the systemic and/or pulmonary circulation);
- Destruction of valves and adaptive changes of the heart (dilatation or hypertrophy;
- Poor circulation (other organs suffer, ischemia occurs - insufficient oxygen supply to the tissues);
- Heart attack;
- Pneumonia;
- Heart failure.
Death is a common result of heart pathologies, especially with congenital defects.
Online consultation with a pediatrician
consultation cost: 500 rubles
Online consultation
During the consultation, you will be able to voice your problem, the doctor will clarify the situation, interpret the tests, answer your questions and give the necessary recommendations.
Diagnostics
At each appointment, the pediatrician conducts auscultation (listening with a phonendoscope) and examination of the chest to check the functioning of the child’s heart, even if the patient came in for ARVI. Pathological murmur is easily auscultated by a cardiologist. It indicates heart problems, even if the patient is not worried about anything or does not attach importance to some symptoms (in addition, children are sometimes afraid to report their problems and worries).
Basic diagnostic methods in cardiology:
- ECG (assessment of the conduction of electrical impulses through the heart muscle);
- Daily ECG monitoring;
- Ultrasound of the heart;
- Echo-CG (study of the morphology and functional state of the heart);
- Doppler echo-CG (study of blood flow in the chambers of the heart and great vessels);
- Plain radiography of the chest (determining the size and location of the cardiac shadow);
- Coronary angiography (study of coronary vessels);
- CT;
- MRI.
It is important to identify the disease in time: the earlier treatment is started, the better the effect. However, most violations can only be detected using special equipment. In addition, the baby is not able to voice complaints, so instrumental diagnostics in pediatrics cannot be avoided.
What may indicate childhood heart disease?
First of all, it is painful sensations in the sternum, as well as in the back in the area between the shoulder blades. Sometimes the pain is so severe that it may be symptoms of coronary artery disease. As a rule, pain appears after active activities or sports, and can sometimes become more active at night when the body is in an uncomfortable position. Among the additional symptoms that indicate that you urgently need to visit a pediatric cardiologist in Saratov are:
- persistent cough;
- frequent fever;
- dyspnea;
- the child complains of headaches;
- severe motion sickness in transport;
- increased fatigue.
During your appointment, an experienced cardiologist will carefully listen to the heart’s function to determine whether the child has a heart rhythm disorder. Heredity is taken into account, as well as:
- how the pregnancy progressed;
- were there any complications during childbirth;
- whether there have been previous infections.
Self-diagnosis
To independently diagnose the state of the cardiovascular system, functional tests are carried out: Martinet-Kushelevsky, Kotov-Deshin, Rufier, with a 15-second run at the fastest pace, and others. You can familiarize yourself with the sampling methodology in the relevant articles on the Internet.
These are simple tests to roughly assess the adaptation of the heart and blood vessels to stress. In schools and universities, they are carried out in special medical physical education groups to monitor the well-being and fitness of students.
Treatment
Therapy depends entirely on the specific nosology. Infectious endocarditis and pericarditis are treated with drugs, but tumors or defects require surgical intervention, otherwise the child will grow, and with it pathological holes (or neoplasms) in the organ, which will lead to death.
Conservative treatment
Non-drug methods are recommended for all patients with a predisposition to or presence of cardiac problems. They include:
- normalization of work and rest regimes;
- 8 hours sleep;
- regular moderate physical activity;
- control of salt intake;
- weight loss (if you are overweight);
- avoiding alcohol and smoking;
- changing your diet towards proper nutrition.
Specific drug therapy depends on the cause of cardiac dysfunction. Main groups of drugs:
- Antibiotics (for bacterial etiology);
- Antihypertensives (Beta blockers, diuretics, ACE inhibitors and angiotensin II receptor blockers dilate blood vessels to lower blood pressure);
- Cardiac glycosides (to restore cardiac conduction and contractility);
- Nonsteroidal anti-inflammatory drugs (suppress inflammation);
- Immunosuppressors (for autoimmune processes), etc.
Surgery
The surgeon restores the heart rhythm by implanting a pacemaker. The batteries for it are changed every 5-7 years during repeated surgery.
All affected valves are replaced with artificial ones. In severe cases, a heart transplant is required.