Published: 05/27/2021 11:45:00 Updated: 05/28/2021
Coronary heart disease is a chronic or acutely developing disease characterized by partial or complete cessation of blood supply to the heart muscle.
The cause of this phenomenon is spasm and thrombosis of the coronary arteries, usually due to their atherosclerotic changes.
Organ ischemia is most often manifested by paroxysmal chest pain - angina pectoris; with a sharp and pronounced disturbance of blood flow in the vessels, myocardial infarction develops.
What is coronary heart disease?
Coronary heart disease is a very broad concept that includes many pathological conditions: from angina pectoris to myocardial infarction with its complications and consequences. IHD occurs when the heart muscle lacks its own blood supply and there is a discrepancy between the myocardium's need for oxygen and its delivery.
Oxygen-rich blood is delivered to the heart muscle through vessels called coronary arteries. When these vessels are damaged, coronary circulation is disrupted, and the myocardium finds itself in conditions of hypoxia (oxygen starvation), which leads to persistent disruption of the functioning of the heart.
ST segment changes
Normally, the ST segment is located on or near the isoline.
Estimates of ST tolerances vary slightly across studies. There may also be different approaches to measuring ST deviation.
The following ST segment displacements are considered pathological.
- Decrease (depression) in ST by 0.5 mm or more in V2-V3 and by 1 mm or more in other leads.
- Increase (elevation) of ST by 2 mm or more in V2-V3 and by 1 mm or more in other leads in men (in men under 40 years old, an increase in ST in V2-V3 to 2.5 mm is acceptable).
- by 1.5 mm or more in V2-V3 and by 1 mm or more in other leads in women
If in two or more than two adjacent leads the ST segment deviates from the isoline by more than the specified values, then this is a pathology.
ST deviation is usually measured at the J point (where the QRS complex enters the ST segment), as well as at ST60 (0.06 s from the J point) and ST80 (0.08 s from the J point).
When measuring the ST deviation at the J point, comparison is made with the level of the PR interval at the point of transition of the PR to the QRS complex. This is shown in diagram 1.
Diagram 1. J point and PR transition point
Schema source.
ECG 1 shows how ST segment displacement can be measured. In the example shown, an ST depression of 2 mm was recorded.
ECG 1. Fragment of a cardiogram with ST segment shift
Measuring the ST segment displacement not at point J, but at a distance of 0.08 s, i.e. 2 mm from the J point may be an alternative approach. This is especially true when there is an initial shift in the PR interval and ST segment due to the atrial repolarization wave.
The wave of atrial repolarization (indicated by Ta) is superimposed on the QRS complex and, as a rule, is not visible on the ECG. However, in some cases, the Ta wave becomes noticeable and displaces the PR interval, QRS and initial ST region.
Illustration of the phenomenon of atrial repolarization, which shifts the PR interval, QRS and initial ST segment in diagram 2. Here the Ta wave is shown in red dotted line.
Scheme 2. Atrial repolarization wave Ta
Schema source.
It is believed that the duration of the atrial repolarization wave does not exceed 0.08 s after the end of the QRS complex. In this regard, the ST displacement measurement is in some cases carried out at a distance of 0.08 s from the J point. The point at a distance of 0.08 s (2 mm) from the J point is called the I point or ST80. When displacement is assessed at ST80, comparison is made with the TP interval (between the T wave and the P wave) rather than with the PR interval.
ECG 2 shows an example when the atrial repolarization wave simulates ST segment depression. A cardiogram was taken from a 25-year-old patient with complaints of chest discomfort. The patient abuses caffeine. The recording showed tachycardia and ST depression in leads II, III, aVF and V2-V6. However, if you look closely, you can also see that the PR segment has an oblique, downward shape. This is due to the atrial repolarization Ta wave, which also shifts ST downward. If you measure the ST level at point ST80 (2 mm after the J point) and compare it with the level of the TP segment, then there will be no significant depression.
ECG 2. ST shift caused by a pronounced wave of atrial repolarization
ECG source.
However, in the case of ECG 2, even without this adjustment, there was no evidence of ischemia, because the shape of the ST segment is obliquely ascending. Ischemia is characterized by downward or horizontal ST depression. Morphological assessment of ST segment changes is more important than assessment of displacement using one or another technique.
A displacement of the ST segment above or below its normal position can occur in different types of coronary artery disease, as well as in other heart pathologies (for example, with blockade of the ventricular pathways, with ventricular hypertrophy, with tachycardia and in other cases).
Different authors and different guidelines suggest different ways to measure ST levels, but everyone agrees that assessing the morphological pattern allows a more accurate conclusion to be made. Therefore, in order to understand what causes ST deviation in each specific case, you need to know the morphological variants of ST displacement.
Why does pathology occur?
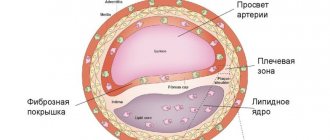
The main cause of the disease is damage to the coronary arteries by atherosclerosis, in which cholesterol plaques appear in the vessels. After some time, a blood clot may form at the site of the plaque, which partially or completely blocks the artery, blocking the supply of oxygen to the heart muscle.
As a rule, narrowing of the lumen of the vessel up to 50% occurs without any clinical manifestations. Vivid symptoms appear when the artery is blocked by 70% or more.
Very rarely (up to 5% of cases) IHD is caused by:
- congenital anomalies of the origin of the coronary arteries;
- Marfan, Ehlers-Danlos syndromes - hereditary pathologies of connective tissue;
- infective endocarditis - inflammation of the inner lining of the heart caused by pathogenic pathogens;
- Kawasaki syndrome is a systemic vasculitis affecting medium and small arteries;
- syphilitic aortitis is a complication of syphilis, in which inflammation of individual layers or the entire thickness of the aortic wall occurs;
- overdose of vasoconstrictors, narcotic drugs.
Risk factors
Risk factors for developing CHD include:
- dyslipidemia - high levels of lipids and/or lipoproteins in the blood;
- diabetes. The disease itself does not cause narrowing of the coronary arteries, but it significantly complicates the course of atherosclerosis;
- arterial hypertension;
- excess body weight;
- smoking. Smoking patients suffer from atherosclerosis more often and more severely. They develop multifocal arterial damage: atherosclerosis affects not only the arteries of the heart, but also the vessels responsible for the blood supply to the brain, head tissue, upper and lower extremities, and kidneys;
- sedentary lifestyle;
- male gender;
- heredity - the presence of atherosclerosis, ischemic heart disease, and arterial hypertension in close relatives.
It is worth noting that a hereditary factor causes IHD only in 20% of cases. Most often, the disease is a consequence of an unhealthy lifestyle.
Clinical forms of the disease
When diagnosing IHD, the clinical form of the disease must be indicated. The differential diagnosis of angina pectoris or myocardial infarction, the most common manifestations of coronary artery disease, is of key importance. Other clinical forms of IHD are much less common.
Angina pectoris is a type of coronary artery disease that manifests itself as chest pain. A dangerous condition is unstable angina, in which an exacerbation of coronary heart disease occurs and the prerequisites for the development of myocardial infarction appear.
Myocardial infarction or heart attack is a critical manifestation of coronary artery disease. During a heart attack, a coronary artery becomes obstructed, which can lead to serious damage or complete death of the myocardium.
The course of the disease, its forms and complications
Classification of IHD
differs from the classifications of other diseases: since coronary disease itself is a state of imbalance between the supply of oxygenated blood to the myocardium and the heart’s need for it, it is difficult to draw an unambiguous line between its forms and complications.
Thus, both myocardial infarction and heart failure are both clinical forms of the disease (acute and chronic
) and complications caused by a lack of myocardial oxygenation.
In this regard, the medical community talks about the clinical classification of forms of coronary artery disease
in the following order:
- Sudden coronary
death (cardiac arrest).
- Angina pectoris
: distinguish between angina pectoris (new, stable, unstable or progressive) and angina at rest (spontaneous/vasospastic/variant/Prinzmetal).
- Myocardial infarction.
- Post-infarction cardiosclerosis.
- Heart
failure (acute and chronic).
- Violations heart
rhythm.
- Silent myocardial ischemia.
- Hibernating myocardium.
- Stunned myocardium.
- Syndrome X.
The development of the disease is not linear, and clinical forms can replace each other. If you do not follow the recommendations of your doctor, chronic forms of IHD
may be complicated by an acute form (heart attack or sudden
coronary
death).
At the same time, after an acute form of IHD (the same heart attack), chronic
consequences
of ischemia
in the form of post-infarction cardiosclerosis
Both acute and chronic forms of IHD can lead to serious consequences for the body
Symptoms of coronary heart disease
The main symptom of the disease is pain behind the sternum, which can radiate under the shoulder blade, to the left arm, neck, and lower jaw. The more pronounced the ischemia, the more severe the pain becomes.
As the pathology develops, the level of physical activity at which pain occurs becomes less and less significant. For example, if at the beginning of the disease a person felt pain in the heart area when climbing the stairs to the fifth floor, then with severe narrowing of the arteries, pain can occur even during normal everyday activities (cleaning the apartment, preparing food, brushing teeth).
With myocardial infarction, the pain behind the sternum becomes very severe and is not relieved even by nitroglycerin. Also during a heart attack a person may experience:
- nausea, vomiting;
- tachycardia;
- dyspnea;
- dizziness;
- cold sweat;
- panic attack;
- fainting.
Symptoms and forms of IHD
With different forms of coronary heart disease, symptoms may differ. There are several forms of the disease.
Angina pectoris
The condition is characterized by attacks of squeezing or burning pain behind the sternum, which usually appears during physical and emotional stress.
It can radiate to the left arm, neck, shoulder, lower jaw, subscapular region, upper abdomen. For this reason, angina pectoris is also called “angina pectoris.” The duration of pain is usually several minutes. Depending on the stability of the course of the disease, stable and unstable forms of angina are distinguished. The first occurs only after physical or psycho-emotional stress, with increased blood pressure, tachycardia. As the disease progresses, the amount of activity available to a person decreases, and in the fourth class of pathology, he can no longer make any movement without developing attacks of chest pain.
Unstable angina can be new - a month or less after the onset of symptoms, progressive and early post-infarction. Progressive angina is characterized by a decrease in the load tolerated, for example, a decrease in the distance that a person can walk without the appearance of symptoms.
Unstable angina requires examination and treatment in a hospital; the risk of myocardial infarction is high.
Myocardial infarction
Develops acutely.
Due to a prolonged decrease in blood flow or its complete cessation to certain areas of the heart muscle, necrosis of the area of the heart muscle occurs - necrosis. The affected area can be of different sizes depending on the diameter of the affected vessel, which is why the disease is often called large-focal or small-focal myocardial infarction. The pain in this condition is intense, pressing and squeezing in nature, and attacks of burning “dagger” pain are also common. In many patients, it has a typical localization in the retrosternal region, but it can also involve the area to the left of the sternum or spread to the entire surface of the chest. In this case, the patient experiences “fear of death”, melancholy, a feeling of doom arises, and may be restless and very excited.
The localization of pain during myocardial infarction can be almost any; for example, sometimes pain occurs even in the abdomen. There is also a painless form.
With small focal lesions, the symptoms may be blurred, and diagnosis by ECG can be difficult.
Spontaneous Prinzmetal ischemia
Substernal pain occurs against the background of spasm of the coronary vessels and is not associated with exercise. Most often, the condition develops at night, between midnight and eight o'clock in the morning. Spastic angina is characterized by regularity and cyclicity, often repeating several attacks in a row with a short interval.
Post-infarction cardiosclerosis
After a heart attack, dead muscle cells are replaced with connective tissue. In this case, conductivity in the myocardium is disrupted, which may be accompanied by sensations of interruptions in the work or prolonged cardiac arrest, periodic fainting and dizziness. There may also be attacks of rapid heartbeat, chest pain, shortness of breath, pale or blue discoloration of the skin.
Heart failure
A disease in which the heart cannot fully perform its function of providing the tissues of various organs with a sufficient amount of blood. The condition is manifested by shortness of breath, swelling, fatigue, and poor tolerance to physical activity.
Heart rhythm disturbances
Arrhythmias are of various types. Accompanied by a feeling of palpitations or a decrease in heart rate. The patient may experience severe weakness, dizziness, nausea, and possible loss of consciousness. There are also asymptomatic forms of pathology, which become an accidental finding on the ECG.
Silent myocardial ischemia
It occurs without characteristic attacks of angina pectoris. It is usually detected accidentally on an ECG and after special diagnostic exercise tests.
Sudden cardiac death
More often it occurs due to ventricular fibrillation or flutter - erratic contraction of the heart muscle at high frequency. The condition develops unexpectedly and is manifested by the following symptoms:
- weakness;
- dizziness;
- loss of consciousness;
- noisy and rapid breathing;
- dilated pupils;
- decrease in respiratory rate;
- absence of heart contractions.
Sometimes the heart can be returned to the correct rhythm, but if this was not done in the first minutes, then the brain cells die from hypoxia, and an irreversible coma develops.
How is diagnosis carried out?
If coronary heart disease is suspected, a thorough examination of the patient is carried out, which may consist of various diagnostic tests:
- Blood chemistry.
When conducting a biochemical blood test, a lipid profile is necessarily performed, aimed at determining the level of lipids (fats) of various blood fractions. Lipid profile indicators include:
- total cholesterol;
- low and high density lipoproteins;
- triglycerides;
- atherogenic coefficient.
Also, during a biochemical study, the level of glucose, C-reactive protein, and creatinine is determined.
- Electrocardiography (ECG).
Electrocardiography is a method of recording and studying the electric fields that arise during the work of the myocardium. If a patient has coronary artery disease, characteristic changes in the ST segment and T wave appear on the ECG.
In addition to the classic ECG, which is performed at rest, ECG tests with physical activity can be used. For example, such tests include bicycle ergometry - a technique for conducting an ECG under conditions of dosed exercise on an exercise bike. This functional test allows you to identify hidden (asymptomatic) IHD and determine blood flow reserves during physical activity.
Another ECG method that can be used to diagnose coronary artery disease is Holter monitoring, which monitors the work of the heart throughout the day. Electric fields are recorded using a portable device - a Holter monitor.
- Echocardiography (ultrasound of the heart).
Echocardiography reveals a wide range of changes in myocardial function that are not always detected during an ECG. During the examination, the doctor can see on the monitor the condition of the heart valves and changes in the size of the myocardial cavities. Echocardiography with Doppler can detect vascular damage and impaired blood flow.
Ultrasound of the heart can be performed both at rest and under conditions of dosed physical activity.
- Scintigraphy.
Study of the heart muscle by introducing radioactive isotopes into the body and subsequently recording their radiation. The uptake of isotopes by heart cells occurs in proportion to the blood flow in it. Therefore, in the presence of affected vessels, the scintigram (image of the myocardium) reveals areas of reduced accumulation of the pharmaceutical.
- Coronary angiography.
This technique is the gold standard in diagnosing coronary artery disease and assessing the degree of arterial damage. During the procedure, a contrast agent is injected into the right and left coronary arteries through catheters. After this, using an X-ray machine, images of the vessels are taken in different projections, which makes it possible to assess their patency. Based on the results of the study, further treatment tactics are selected.
Measures to prevent cardiovascular pathology
To avoid developing heart disease, you need to stop smoking and reduce your alcohol consumption.
Severe stress is also one of the predisposing factors to the occurrence of IHD. It is impossible to remove stress from life, but you can react to it correctly: humans are evolutionarily designed in such a way that muscle work is necessary after any stress. If you are worried or upset, then you need to squat, jog, or walk – the muscles should get tired. In case of severe anxiety, you may need to use sedatives, for the selection of which you need to consult a doctor.
Regular exercise with moderate physical activity is useful for the prevention of ischemia. You also need to monitor your weight and blood pressure. All persons over 40 years of age must be examined annually - take a biochemical blood test to check the level of cholesterol in the blood, and do an ECG.
Treatment of coronary heart disease
There are three main methods of treating IHD.
- Drug treatment, which may include taking antihypertensive drugs, antiplatelet agents, statins, beta blockers, ACE inhibitors, nitrates and other drugs.
- Stenting is the dilation of blood vessels by installing stents (thin metal tubes) into them. The procedure is carried out under the control of coronary angiography.
- Coronary bypass surgery is a surgical operation that is performed in case of severe damage to the coronary arteries and a large number of atherosclerotic plaques. During the operation, new pathways are formed for blood movement to bypass the narrowing sites. Shunts are created from the patient's own arteries. Coronary bypass surgery not only restores blood supply to the heart, but also eliminates the risk of re-development of coronary artery disease.
Also, a mandatory element of treatment is lifestyle changes (giving up bad habits, following a diet, dosed physical activity).
What medications are used to treat ischemic heart disease?
Medicines that lower blood pressure
High blood pressure negatively affects the blood vessels of the heart and other organs, causing them to become even more constricted and receive less oxygen. Reducing and constantly maintaining normal blood pressure is a key factor in the treatment of coronary artery disease. The target blood pressure level for coronary artery disease is 140/90 mmHg. or less for most patients, or 130/90 for patients with diabetes or kidney disease. For severely ill patients, even lower numbers are recommended. In the vast majority of cases, achieving this level of blood pressure requires constant use of antihypertensive drugs.
ACE inhibitors
This is a class of drugs that block the enzyme angiotensin-2, which causes high blood pressure and other negative effects on the heart, kidneys and blood vessels. Recently, many positive effects of ACE inhibitors on the prognosis of patients with coronary artery disease have been proven, so they are prescribed as widely as possible, in the absence of contraindications. These include, for example, enalapril, lisinopril, perindopril and others. Long-term use may cause coughing and is not suitable for all patients. Used as prescribed by a doctor.
Angiotensin receptor blockers
These drugs make it possible to block not angiotensin-2 itself, but its receptors located in various organs, including the heart. In some cases this is much more effective. ARBs are less effective at lowering blood pressure than ACEIs, but they have several additional beneficial effects on the heart and blood vessels. In particular, some of them are able to stop the growth of the heart muscle (hypertrophy) and even reduce it by several percent. They are used in all groups of patients, and especially in those who cannot tolerate ACE inhibitors.
Long-term, lifelong use, as prescribed by a doctor. Examples of drugs: losartan (Cozaar, Lozap, Lorista), valsartan (Valz, Diovan, Valsacor), candesartan (Atacand), telmisartan (Mikardis) and others.
The choice of a specific drug, regimen of its use and dose is within the competence of the doctor, since it is necessary to take into account the individual characteristics of the course of the disease and concomitant diseases.
Drugs that improve heart function
Beta blockers
Block receptors for adrenaline and other stress hormones in the heart. Reduces heart rate and blood pressure. They have a beneficial effect on the heart during arrhythmia and can eliminate it.
Recommended for continuous use in all patients after myocardial infarction and pre-infarction conditions, as well as with left ventricular dysfunction, regardless of the presence of heart failure, in the absence of contraindications. Use can be long-term or short-term, only as prescribed by a doctor. Most of them are contraindicated for bronchial asthma, many increase blood sugar and are not used for diabetes.
Examples of drugs: anaprilin, metoprolol (Egilok), bisoprolol (Concor), etc.
Nitrates
Basic medications for stopping (eliminating) an attack. These include drugs such as nitroglycerin (“Nitromint”), isosorbide dinitrate (“Isoket”) and mononitrate (“Monocinque”), etc. They act directly on the coronary vessels and lead to their rapid expansion, and also reduce blood flow to the heart due to the expansion of deep veins, which can store blood. All this facilitates the work of the heart and reduces its need for oxygen, which means it reduces oxygen starvation and pain.
Currently, nitrates are used mainly to relieve attacks of angina pectoris, and for continuous use in severe patients with chronic heart failure. All nitrates develop addiction, and their effect decreases over time, but after short-term withdrawal it is restored again.
Cardiac glycosides
Digoxin, corglycone, etc. Strengthen contractions of the heart muscle and slow down their frequency. Currently, they are used in the treatment of coronary artery disease infrequently, mainly for atrial fibrillation and severe edema. They have many side effects, especially in combination with diuretics, and therefore should be prescribed by a doctor only after a thorough examination.
Cholesterol-lowering drugs
For most patients, the following figures are recommended:
- total cholesterol level should be no more than 5 mmol/l,
- low-density lipoprotein (“bad”) cholesterol level – no more than 3 mmol/l,
- high-density lipoprotein (“good”) cholesterol level is at least 1.0 mmol/l.
The atherogenic index and triglyceride levels also play a role. In severely ill patients (for example, with concomitant diabetes mellitus), these indicators are recommended to be monitored even more strictly.
Target cholesterol levels are achieved through a special diet and medications. In most cases, diet alone is not enough, but without it, taking medications will not be as effective. Modern medications can significantly lower cholesterol levels, but they must be taken constantly. Basically, drugs from the statin group (atorvastatin, simvastatin and others) are used for this purpose. The specific drug is prescribed by the doctor.
Drugs that reduce blood viscosity
The more viscous the blood, the greater the likelihood of blood clots forming in the coronary arteries and the worse the blood supply to the heart muscle. To reduce blood viscosity, two groups of drugs are used: antiplatelet agents and anticoagulants.
The most common antiplatelet agent is aspirin. It is recommended to be taken daily by all patients with coronary artery disease throughout their lives at a dose of 70–150 mg per day (in the absence of contraindications, such as a stomach ulcer). For patients after heart and vascular surgery, the dose can be increased as prescribed by the doctor, and clopidogrel can be added at a dose of 75 mg per day.
In patients with a permanent form of atrial fibrillation, the doctor may prescribe a stronger medication - the anticoagulant warfarin, in a dosage that ensures that the INR (blood clotting indicator) is maintained at a level of 2.0 - 3.0. Warfarin dissolves blood clots more effectively than aspirin, but may cause bleeding. Use only as prescribed by a doctor after a thorough examination and under the supervision of blood tests.
Medicines that control blood sugar (glucose) levels
A modern criterion for controlling diabetes mellitus is the level of glycated hemoglobin (HbA1c). It reflects the blood sugar concentration over the past week and should not exceed 7%. A single blood sugar test does not reflect the true picture of the course of diabetes.
To achieve the target sugar level, all non-drug measures should be used (diet, exercise, weight loss), and in case of their insufficiency, specific drug therapy as prescribed by an endocrinologist.
Other drugs
Diuretics (diuretics)
They have two areas of application: in low doses to lower blood pressure (most often in combination with other drugs), in high doses to remove fluid from the body in congestive heart failure. They tend to increase blood sugar, so they are used in extreme cases for diabetes.
Antihypoxants
Antihypoxants are drugs that reduce oxygen starvation of the heart muscle at the molecular level. One such drug is trimetazidine. It is not included in standard treatment regimens for coronary artery disease and can be used as an additional remedy. Not registered in the US Pharmacopoeia.
Nonsteroidal anti-inflammatory drugs (NSAIDs)
A large-scale study in the United States revealed a detrimental effect of this class of drugs on the prognosis of patients with myocardial infarction. In this regard, medications such as diclofenac and ibuprofen are not recommended for use in people after a heart attack or similar conditions.
Flu vaccination
Recommended for all people with diseases of the cardiovascular system.
Prevention measures
Measures to prevent IHD include:
- proper nutrition. Avoid consuming saturated fats, which increase cholesterol levels. The diet should include as many polyunsaturated fatty acids as possible, which have an antiatherogenic effect and prevent the development of cardiovascular diseases. Useful foods for the cardiovascular system - ocean fish, seafood, vegetable oils (sesame, olive, rapeseed);
- active lifestyle. Physical activity improves blood circulation, normalizes blood pressure, and prevents weight gain;
- blood pressure control;
- giving up alcohol and smoking;
Also, do not forget about timely diagnosis. to visit a cardiologist not when pain in the heart appears, but regularly (once a year). This is especially important if you are at risk of developing coronary heart disease.
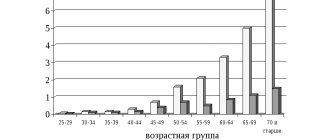
Prevalence of the disease
In Russia, about 5.1-5.3% of the population suffers from ischemic heart disease.
At the same time, coronary heart disease remains the main cause of mortality and disability in the population. Worldwide, deaths from pathologies of the cardiovascular system account for a third of diagnosed cases. In Russia, this figure is higher and amounts to 57%, of which 29% are deaths due to myocardial ischemia. Myocardial ischemia mainly affects people over 40 years of age. In young and middle age, coronary heart disease is more often detected in men; with increasing age, the ratio of cases evens out.