Cardiovascular diseases are the leading causes of death among young people (from 25 to 64 years old) in Russia. The main insidiousness of this group of diseases is that they are often asymptomatic, and a person finds out that he has heart problems when it is no longer possible to help him. We talked with EuroMed Clinic cardiologist Olga Aleksandrovna TSURKAN about what cardiac diseases are most common, how they manifest, and what symptoms are recommended to pay attention to.
The heart is a muscular organ that “pumps” blood throughout the body. The heart muscle is called the myocardium, and it constantly works - on average, at rest the heart “pumps” 5 liters of blood per minute, and during intense exercise - more than 15 liters per minute! In order to carry out this work effectively, the coordinated work of the entire system is important: the main muscle (myocardium), atria, ventricles, and blood vessels. The myocardium must be constantly well supplied with nutrients and oxygen. If the functioning of one of the elements of the system is disrupted or the vessels supplying the heart with blood are clogged with cholesterol plaques, cardiac diseases develop.
Hypertonic disease
Hypertension or arterial hypertension (AH) is a very common condition associated with chronic high blood pressure. This disease can develop as a consequence of some other conditions (secondary hypertension), or on its own (primary hypertension).
Blood pressure is the pressure inside blood vessels called arteries. The blood expelled from the heart (about 60 ml) with one contraction stretches the aorta and large arterial vessels from the inside. The walls of the blood vessels expand under the pressure of blood and then narrow again. The strongest pressure on the blood vessels is recorded during heart contraction (systole) - this pressure is called systolic. When the heart relaxes (diastole), the blood pressure in the arteries decreases. This pressure is called diastolic.
In a healthy person, systolic blood pressure ranges from 100–140 mmHg. Art., and diastolic is about 70–80 mm Hg. Art. Normally, pressure numbers can fluctuate depending on a person’s condition: increase during physical or psycho-emotional stress, decrease during sleep.
The reasons why normal blood pressure is disrupted, in most cases, cannot be established. There are certain factors that increase a person's risk of developing hypertension. They can be divided into non-modifiable (which we cannot change) and modifiable.
Non-modifiable causes:
- Age. With age, the walls of large arteries become tougher and more rigid, which increases vascular resistance to blood flow, and therefore increases blood pressure.
- Hereditary predisposition. The genetic factor is considered to be the main factor in the development of essential hypertension. However, the genes responsible for the occurrence of this disease have not yet been discovered.
- Floor. Men are more likely to suffer from arterial hypertension.
Modifiable reasons:
- smoking;
- excess salt in the diet;
- excessive alcohol consumption;
- abdominal obesity (fat deposition in the abdominal area, “beer belly”);
- low physical activity;
- chronic stress;
- increased blood sugar;
- snoring, especially with pauses in breathing;
- changes in the lipid (fat) composition of the blood. The eradication of these “vices” of modern life is the basis for the prevention of not only hypertension, but also all cardiovascular diseases in general.
Symptoms of hypertension
- headache,
- dizziness,
- flashing “flies” before the eyes.
Most often, hypertension is not accompanied by any symptoms and is detected accidentally when measuring blood pressure or after the development of its complications, the most dangerous of which is stroke. Therefore, to prevent the development of hypertension, I recommend regularly measuring your blood pressure; if something worries you, consult a doctor immediately.
Against the background of a sudden increase in blood pressure, a hypertensive crisis may occur. accompanied by pathological changes in the brain and cardiovascular system against the background of autonomic disorders (chills, trembling, sweating, a feeling of a rush of blood to the head, a feeling of lack of air, etc.). The level of blood pressure at which clinical manifestations appear varies from person to person (in one patient it is 240/120, in another - 130/90 mmHg) - it depends on the initial level of blood pressure. If the patient is hypotensive, even a slight increase in blood pressure can cause the clinical picture of a hypertensive crisis.
If a hypertensive crisis is accompanied by intense chest pain, shortness of breath, loss of vision, impaired coordination of movements, vomiting, call an ambulance immediately! Such crises pose a danger to the patient’s life and require immediate reduction of blood pressure in a hospital setting. Complications of a crisis may include myocardial infarction, heart rhythm disturbances, bleeding, strokes, acute encephalopathy, acute renal failure, etc.
What symptoms will help recognize coronary artery disease?
The insidiousness of the pathology lies in the absence of any symptoms in many cases.
It can develop for years, without the person even realizing that coronary heart disease is present in the body. The first signs of the development of IHD are discomfort in the chest area, panic attacks, and fear of death. Over time, IHD progresses and manifests itself with various symptoms. The clinical picture varies depending on the specific form of the disease. Periods of exacerbation alternate with a stable state. The following signs indicate IHD:
- fatigue, lethargy, weakness and dizziness;
- feeling of short-term lack of air;
- burning and heaviness in the chest;
- nausea;
- during physical activity - discomfort in the chest.
Other symptoms of coronary heart disease: shortness of breath when walking and running quickly, arrhythmia, a sharp increase in blood pressure, excessive sweating and others. Based on the listed signs, one can guess the development of coronary artery disease, but they do not appear simultaneously, but depending on the type of pathology and the degree of its neglect. If you notice two or three of the listed symptoms recurring, do not delay a visit to a specialist.
Coronary heart disease (CHD)
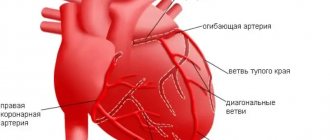
IHD is a disease in which the blood supply to the heart muscle is disrupted, causing it to lack oxygen and nutrients. This usually occurs due to blockage of the main arteries of the heart by atherosclerotic plaques. Over time, they become more and more numerous, and when the lumen of the vessel is blocked by 60% or more, difficulty in blood flow occurs, oxygen starvation develops (hypoxia), which leads to myocardial ischemia and the occurrence of an angina attack, as well as the most dangerous complication of coronary artery disease - acute myocardial infarction.
Angina is a temporary, transient lack of blood supply to the heart muscle (myocardium). An attack of angina occurs when the lumen of the coronary artery, through which the heart muscle is supplied with oxygen, narrows. During an attack of angina, pain occurs that is pressing, squeezing or burning in nature, localized in the middle of the chest, behind the sternum, radiating upward (to the neck, lower jaw, teeth) or to the arms. Most often, pain occurs during physical or emotional stress and goes away with rest.
An attack of angina is a signal that the heart muscle is experiencing a lack of blood supply, the first “bell” that indicates that you need to urgently consult a doctor in order to prevent a more dangerous complication, such as acute myocardial infarction.
Acute myocardial infarction is the death of a section of the heart muscle due to disruption of its blood supply. This can happen due to blockage of the vessel by a thrombus - a blood clot that forms at the site of damage to the atherosclerotic plaque. As a result, blood stops flowing to the heart muscle, and this leads to myocardial infarction - necrosis, tissue death. Subsequently, a scar forms at this site.
Most often, during myocardial infarction, a person experiences acute pain (burning, pressing) behind the sternum or on both sides of the chest, often the pain radiates to the jaw, neck, back under the shoulder blades, and to the upper abdomen. The pain may appear in waves - sometimes intensifying, sometimes weakening. The pain may be accompanied by irregular heartbeat, weakness, cold sweat, decreased blood pressure, a feeling of lack of air, dizziness, fainting, and nausea. This condition lasts from 20 minutes to several hours. The above symptoms may appear in different combinations, not all signs need to be present. In some cases, myocardial infarction can occur without significant pain, with atypical pain sensations (similar to osteochondrosis or gastric ulcer, for example), and can also occur completely asymptomatically.
We must remember that acute myocardial infarction is a dangerous disease with a high mortality rate. Therefore, if you suspect yourself or a loved one has a myocardial infarction, do not delay, call an ambulance immediately.
Unexpected situation
Many people are interested in whether a heart attack can develop in young people, as they say, out of the blue. “Yes, indeed, at a young age, myocardial infarction most often develops without previous heart pain. But, as we said above, if you pay attention in time to developing changes that at first glance are not related to the heart, you can begin to implement preventive measures in time and prevent the development of an attack,” says Galina Lazarenko.
Prevention of flaming motor. How to influence the age of the heart Read more
Heart failure
Heart failure is a pathology in which the heart cannot fully cope with its function, as a result of which other organs and tissues of the body do not receive enough nutrients and oxygen.
Heart failure is expressed as a discrepancy between the needs of the body and the capabilities of the heart. Normally, the heart muscle contracts with a certain intensity and “pumps” a large amount of blood. In heart failure, the organ cannot cope with its function. Most often, this is expressed by shortness of breath, weakness, and swelling. At the initial stage of development of the disease, heart failure manifests itself only during physical activity - when the heart is forced to work more intensely. At this stage, the disease can still be cured completely, so do not ignore even faint hints of symptoms and consult a doctor!
The more advanced the disease, the greater the disruption in all organs and systems that can result from a long-term lack of blood supply and nutrients.
Atrial fibrillation
Atrial fibrillation (or atrial fibrillation) is a disease in which the rhythm of heart contractions is disrupted. Normally, the conduction system of the heart produces an impulse that causes the heart to contract at a certain frequency, in sinus rhythm. With atrial fibrillation, the sinus node stops working, the muscle fibers of the two upper chambers of the heart stop contracting rhythmically, but flutter, tremble, or contract uncoordinated. This leads to an irregular heartbeat, and as a result, blood flows unevenly into the chambers of the heart and can accumulate in them, resulting in the formation of blood clots (thrombi). The blood clot can travel to the brain through the bloodstream and cause a stroke. Uncontrolled atrial fibrillation increases the risk of stroke by about 5 times!
Symptoms of atrial fibrillation: changes in heart rate, shortness of breath, chest pain, weakness, dizziness, fainting. Often, with atrial fibrillation, a person does not feel any changes, and the disease is discovered by chance - during a preventive examination.
The number of diagnosed cases of atrial fibrillation is constantly growing. At the same time, new, modern drugs have now appeared that effectively fight this disease. The main thing is to contact a cardiologist in time.
Nowadays we no longer talk about individual diseases. As a rule, diseases of the cardiovascular system manifest themselves in a complex. It practically never happens that a person has just one thing, just arterial hypertension, for example. This is a single system, and one thing leads to another, each cardiac disease increases the risk of developing another one.
Preventive actions
“First, it is necessary to assess the risk factors when identifying the first signs of metabolic syndrome: increased abdominal circumference, increased blood pressure, increased cholesterol, C-reactive protein, blood sugar. You should immediately contact a cardiologist or endocrinologist. This will allow us to develop an individual plan of preventive measures as early as possible,” says Galina Lazarenko.
It is also worth quitting smoking as early as possible and optimizing physical activity. “All healthy people need moderate-intensity aerobic exercise for 30 minutes a day, 5 times a week, or vigorous-intensity aerobic exercise for at least 20 minutes a day, 3 times a week. Walking 10,000 steps a day every day is required.
Question answer
How can climbing stairs help check your heart health? You can determine the desired intensity of the load by your pulse during training. The maximum heart rate will be equal to the difference between 220 and the patient's age. 60-70% of the obtained value will be the optimal heart rate for moderate-intensity exercise, 75-85% for intense training,” notes the cardiologist.
And, of course, the doctor emphasizes, it is extremely important to normalize nutrition: exclude fast carbohydrates, alcohol, saturated fats (meat with visible fat, for example) from the diet, increase the proportion of foods containing polyunsaturated fats (omega-3 acids - they are contained in sea fish, olive, flaxseed oil), whole grains, vegetables and fruits (at least 5-6 servings per day), reduce salt intake (up to 2-3 grams per day).
Methods for diagnosing the state of the cardiovascular system
Electrocardiogram (ECG) at rest. An ECG measures the heart rate and allows you to assess the condition of the heart muscle and the overall condition of the heart. This is usually a so-called screening examination - that is, one that is recommended to be performed regularly prophylactically, even in the absence of complaints. Unfortunately, it is not very informative due to its short duration, but we can “catch” the most serious pathological changes using an ECG.
If there are complaints or suspicion of diseases, it is recommended to perform more detailed, extensive tests.
ECG with physical activity (treadmill test). This procedure involves continuous ECG recording and blood pressure monitoring under conditions of stepwise increasing dosed exercise on a treadmill until a submaximal heart rate is reached (200 minus age). This makes it possible to identify possible ischemia (oxygen starvation) of the heart muscle, which is not detectable at rest, and to register existing heart rhythm disturbances (most often they lead to sudden deaths in athletes).
The study is carried out on a specially equipped treadmill. During the treadmill test, walking is actually simulated - a familiar type of exercise for any person. This is why most researchers consider the treadmill test to be a more physiological method of stress testing. Adhesive electrodes are attached to the chest and distal extremities to record ECG. Using a computer program, the slope of the track is adjusted, due to which the patient is given a certain physical activity with a gradual further increase. Simulates walking uphill. Along with the ECG, blood pressure is measured at certain intervals.
During the treadmill test, the patient must report the occurrence of pain and other unpleasant sensations. The study ends when a certain heart rate is reached, or due to a deterioration in the patient’s well-being. After stopping the procedure, the cardiogram and blood pressure readings continue to be recorded for about 10 minutes.
The value of any examination is characterized by the sensitivity and specificity of the method, which are quite high for the load treadmill test: according to various authors, the sensitivity of the treadmill test is 80–85%, the specificity is 83–88%.
The results of the treadmill test allow you to choose the most optimal treatment method - conservative or surgical, evaluate the effectiveness of therapy, give recommendations on household and professional physical activity, and create rehabilitation and training programs.
Types of ischemia
Among all forms of IHD, the following are common:
- Angina pectoris - this form is characterized by pressing pain in the sternum, heaviness in the heart. Character of pain: cutting, pressing, squeezing. In some cases, an acute lack of oxygen replaces the attack of pain. Symptoms appear suddenly and disappear after a few minutes.
- Myocardial infarction is long lasting pain of high intensity. There is a feeling of lack of oxygen, possibly cold sweating, severe weakness, and an attack of fear.
- Heart failure is a disordered natural rhythm of the heart, shortness of breath is observed even with mild exercise, weakness, and swelling of the legs.
- Heart rhythm disturbances are another common form of pathology. There are interruptions in the functioning of the heart muscle. The feeling of freezing is replaced by an accelerated heartbeat.
Holter ECG monitoring
This examination is a continuous recording of heart function on an ECG throughout the day - using a special portable device that is attached to the patient. During the study, the patient is recommended to lead a normal lifestyle - for the most accurate result.
A holter is a small device that is attached to the patient’s belt; the sensors are attached to the chest. The procedure itself is automated; the patient does not need to do anything with the device. During Holter monitoring, the patient keeps a diary of activity and rest, and notes his well-being. After the device is removed, the data from the device and from the patient’s diary are entered into a special program in which this information is analyzed and a daily cardiogram is displayed.
Daily monitoring allows you to track the dynamics of a person’s heart over a longer period of time than with a conventional ECG or measuring blood pressure. As a result, we get a much more complete and reliable picture.
24-hour blood pressure monitoring (ABPM).
ABPM is an automatic measurement of blood pressure for a day or more (if necessary) at certain intervals, according to a given program (usually every 15 minutes during the day and 30 minutes at night). A cuff for measuring blood pressure is placed on the patient's shoulder, connected to a portable monitor of small size and weight (about 200 grams), which the patient wears on his belt. Measurements are carried out on an outpatient basis, during the patient’s normal activity. The system provides automatic measurement of pulse, systolic and diastolic blood pressure at set time intervals, on the basis of which average daily blood pressure and pulse values during the day and night are calculated, the degree of nighttime decrease and morning increase in blood pressure, response to physical activity and psycho-emotional stress is determined, the degree and duration of hypertensive load on target organs, variability of pressure and pulse during the day, episodes of hypotension are detected. For a more accurate assessment, the patient is asked to keep a diary in which he describes his well-being and complaints during the examination, his activities, physical activity, indicates the time of taking medications, notes the time of sleep and awakening. The only limitation for the patient during ABPM is the need to relax the arm on which the measurement is being taken for more accurate registration.
The technique is simple, painless and very informative. It increases the accuracy of assessing the true level of blood pressure, especially if the presence of initial, unstable arterial hypertension is suspected.
Ultrasound of the heart. During the examination, the doctor can evaluate the structural features of the heart, the condition of the chambers and valves of the heart, the aorta, the size of the heart cavities and the pressure in them, the thickness of the walls of the heart, the thickness of the myocardium, the contractility of the heart muscle, the speed of intracardiac blood flow.
Ultrasound of the vessels of the head and neck is a screening examination for the presence of atherosclerotic changes in the walls of arterial vessels. An ultrasound will clarify the condition of the arteries and veins supplying the brain, which will allow us to draw conclusions about the risk of developing cardiovascular accidents, as well as see problems in the blood supply to the brain, neck, head and spine.
Vascular ultrasound is especially recommended for men over 40 years of age - unfortunately, in this category of patients there are often changes in the condition of the vessels, which can be determined thanks to this study.
Blood tests
A cardiologist may recommend tests for cholesterol, glucose, and uric acid.
These indicators reflect the state of metabolism in the body: fat, protein, carbohydrate. Deviations from the norm for these indicators may indicate an increased risk of stroke or heart attack.
Symptoms that you should pay attention to
First of all, the pressure level. Increased blood pressure is always a sign that you need to see a doctor. Signs such as headaches, redness of the skin, tinnitus, and dizziness can indirectly indicate high blood pressure.
Chest pain, especially associated with walking and physical activity. Chest pain can also appear with increased blood pressure or stress. Such pain most likely indicates heart disease. The pain syndrome can be either constant or appear only during exercise, and subside with rest.
Shortness of breath is another fairly common symptom of heart problems.
It is important to understand that heart disease is often asymptomatic or with mild symptoms. And with age, the risk of their development increases significantly. Therefore, any man over 40 years of age and woman over 50 years of age should regularly visit a cardiologist for preventive care. Come at least once a year, perform an ECG, and see if everything is in order.
Most heart diseases, “caught” at the initial stage, are successfully treated. The contrast between how simple the prevention of cardiovascular diseases is and how serious the consequences they can have is simply amazing!
Why is it necessary to visit a cardiologist and do an ECG during pregnancy? Pregnant women who are registered at the antenatal clinic are sent for an ECG several times during pregnancy, and are also often recommended to consult a cardiologist. In addition, blood pressure is monitored at every doctor’s visit. What is this connected with? Pregnancy is always stressful for the body. During pregnancy, the load on the entire body and, in particular, on the heart increases. The volume of circulating blood increases, and the heart rate increases. This can provoke the development of hypertension, heart defects, and rhythm disturbances. Therefore, it is important to constantly monitor the woman’s condition in order to stop the disease in time and prevent the development of serious complications. It often happens that these conditions appear during pregnancy and disappear after childbirth.
Provoking factors
There are a number of factors that can provoke the development of a heart attack in young people. “In addition to those factors that can influence the development of atherosclerosis, it is important to talk about conditions that are not associated with the growth of plaque in the vessels of the heart, but can provoke heart problems in young people. These are factors that reduce the supply of oxygen to the heart. For example, iron deficiency anemia or dysfunction of the thyroid gland (hyperthyroidism),” says Galina Lazarenko.
In addition, she also calls the development of inflammation in blood vessels after viral diseases a provocateur. The list also includes:
- The presence of bad habits: smoking and alcohol can be provoking factors for sudden blood clots, drugs can provoke spasm of the heart vessels and lead to a heart attack.
- The use of oral contraceptives by a woman, which can cause sudden thrombosis in blood vessels, including the heart, with a certain predisposition to increased thrombosis.
“Work pressure” is a harmful myth
There is an officially permitted maximum upper limit for blood pressure: 140/90 mmHg. Art. - this is the limit after which hypertension is already diagnosed.
But there is a widespread myth among the people that there is so-called working pressure - it can be above this limit, but it is believed that if a person feels well, then there is nothing to worry about, there is no need for treatment. This is a dangerous misconception!
The risk of complications from hypertension is equally high, regardless of whether you feel unpleasant symptoms or not! Yes, hypertension is often asymptomatic. But the risks of hypertensive crisis, stroke, heart attack, etc. remain. Therefore, the main indicator for prescribing treatment is the results of measuring blood pressure, and not the patient’s well-being. High blood pressure must always be reduced - this is the only way to avoid complications and serious consequences of hypertension.
Another common misconception is that medications to normalize blood pressure cannot be taken constantly, but only during episodes of high blood pressure. This is wrong. Arterial hypertension is a chronic disease. And in order for the patient’s condition to remain stable, medications must be taken as prescribed by the doctor - regularly. Agree, it’s not such a big price to pay for good health and reducing the risk of stroke and other complications - take a pill once a day!
Extrasystole - what is it? Extrasystole is one of the types of heart rhythm disturbances. Quite a lot of people are diagnosed with extrasystole on the ECG; this disorder is quite common. Only a doctor can determine how serious this is. Most likely, if you have been diagnosed with extrasystole, this is not a reason to panic; even a completely healthy heart can cause such a rhythm disturbance. But it is important that such arrhythmia can be provoked by serious heart diseases, that is, in this case, extrasystole will be one of the symptoms. That is why you should not ignore such “findings” and definitely need to be examined by a cardiologist.