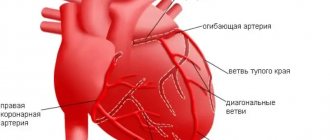
Supraventricular arrhythmia is a disorder of the heart rhythm, the source of which is located above the Hiss bundle. It is also called supravintricular. The pathological focus can be located in the muscular layer of the atria, the mouths of the vena cava or pulmonary veins, or in the atrioventricular node. In addition, this group includes arrhythmias, which are caused by the appearance of abnormal atrioventricular (atrioventricular) pathways. The severity of the disease and prognosis will vary depending on the degree of damage to the conduction system, the age of the patient and many other factors. Treatment is complex, prescribed based on the results of specific tests and various diagnostic methods.
Classification
Supraventricular arrhythmia is a general name for a number of pathologies that manifest as disturbances in heart rhythm. They differ in symptoms and require different treatment regimens. For a more accurate diagnosis, a classification is used that identifies several types of supraventricular arrhythmias:
- extrasystole;
- tachycardia of various types;
- accelerated supraventricular rhythms;
- atrial flutter and fibrillation.
REFERENCE! The most common types of supraventricular heart rhythm disturbances are extrasystole and sinus tachycardia. They can be diagnosed even in a healthy person of any gender and age.
Causes of supraventricular arrhythmia
It was noted above that in the development of arrhythmia the primary role is played by a provoking factor, which can have a functional or organic origin.
Functional reasons:
- autonomic dysfunctions;
- excessive consumption of alcoholic and caffeinated drinks;
- irregular work schedule with insufficient rest;
- hormonal disorders (most often in women and adolescents);
- infectious processes accompanied by high fever.
Organic reasons:
- heart defects;
- myocarditis and endocarditis
- postoperative disorders;
- traumatic heart lesions;
- tumor processes located in the heart area;
- pulmonary heart disease, which developed against the background of pulmonary hypertension.
Some metabolic disorders, such as a lack of potassium, magnesium, and renal failure in the blood, can also contribute to the development of NFA.
The use of cardiac glycosides, sympathomimetics, theophylline and antiarrhythmic drugs in incorrect doses can cause supraventricular arrhythmia.
If the patient has a state of hypoxia, which often occurs with anemia, heart failure and bronchopulmonary pathology, the activity of the heart can be disrupted by the type of arrhythmia localized in the atria.
Types and features
Each type of arrhythmia has different causes; they differ in severity and clinical picture. They are united by the localization of the source of heart rhythm disturbances - it is located above the Hiss bundle. These pathologies can be felt as an acceleration or unevenness of the heartbeat, the appearance of additional beats, a slower pulse and other symptoms.
Supraventricular extrasystole
Extrasystole is an extraordinary contraction of the heart muscle. Its main reason is the appearance of an electrical impulse outside the sinus node, to which the myocardium reacts with excitation. As a result of a decrease in the interval between beats, the heart does not have the opportunity to fully recover. There are two main forms of supraventricular extrasystole:
- atrial - before an extraordinary contraction of the heart, an additional P wave is recorded on the ECG (indicates contraction of two atria);
- extrasystole from the atrioventricular (atrioventricular) junction - there is no additional P wave.
Supraventricular extrasystole can occur even in healthy people. It is caused by emotional stress, excessive stress, caffeine consumption or smoking, as well as poisoning or taking certain groups of drugs. However, it can also be caused by pathologies of the muscular lining of the atria, pulmonary or vena cava, and atrioventricular junction.
In some patients, supraventricular arrhythmias are asymptomatic, and they can only be detected during a routine examination
Supraventricular tachycardia
Supraventricular tachycardia is a condition in which there is an increase in the frequency of heart contractions without disturbing their rhythm. In some cases, the pulse can reach 140-180 beats per minute, which provokes rapid fatigue and wear of the heart muscle. There are several types of tachycardia:
- sinus;
- sinoatrial reciprocal;
- atrioventricular nodal reciprocal;
- atrial;
- tachycardia caused by overexcitation syndrome.
REFERENCE! There are physiological and pathological tachycardias. The first is the body’s reaction to increased adrenaline levels, stress or physical activity, the second is a consequence of diseases of the cardiovascular system.
Sinus tachycardia
Sinus tachycardia is one of the most common manifestations of supraventricular arrhythmias. The heart rate increases to 100 beats per minute or more. Tachycardia, which persists even at rest, without physical activity, is of important clinical significance. The main symptoms are a regular but rapid heart rate, as well as a feeling of lack of air. Tachycardia can occur as a result of anemia or low blood pressure, blood loss, systemic inflammatory diseases, thyroid pathologies, heart or pulmonary failure. This condition is dangerous due to insufficient blood supply to the heart and blood vessels, as a result of which the myocardium experiences increased stress.
Atrial tachycardia
Atrial tachycardias occur less frequently than sinus tachycardias. Their source can be localized in the right (usually) or left atrium. According to the nature of their course, they can be paroxysmal and non-paroxysmal. The first option is paroxysmal - tachycardia occurs against the background of stress or physical exertion, and then the heart rate returns to normal limits. Non-paroxysmal tachycardia can occur in two forms. The first of them is a chronic course that can last for many months and even years. The second is an often relapsing form.
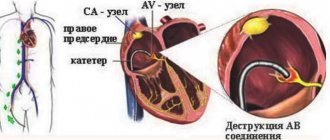
Nodal reciprocal atrioventricular tachycardia
Reciprocal atrioventricular tachycardia is one of the most commonly diagnosed disorders. Its cause is the division of the atrioventricular node into two paths, as a result of which electrical impulses pass from the atria to the ventricles incorrectly. There are several main forms of junctional tachycardia, which differ in the mechanism of occurrence:
- typical option - the impulse moves from the atria to the ventricles along the slow path, and then returns along the fast path;
- atypical variant (fast-slow) - the impulse moves to the ventricles along the fast path, and returns to the atria along the slow path;
- Another atypical option (slow-slow) - in both directions the electrical impulse moves along slow paths.
A typical variant is easily recognized on an ECG. During an attack of arrhythmia, simultaneous excitation of the atria and ventricles occurs; there may be a slight delay between these processes. The P wave becomes invisible because it overlaps the QRS complex. Other options are less common.
IMPORTANT! Nodal atrioventricular tachycardia often has a favorable course. In 15% of cases, there are no concomitant pathologies of the heart or blood vessels, so symptomatic treatment is sufficient.
Atrial flutter
Atrial flutter is a coordinated but significantly accelerated heartbeat. Its speed can reach 250‒350 beats per minute. It is too high, but is partially controlled by the atrioventricular node. It does not allow all impulses to pass through, so the frequency of ventricular contractions reaches 150 times per minute. The main cause of this condition remains acute and chronic diseases of the cardiovascular system, as well as congenital and acquired heart defects. It is rarely diagnosed in patients without organic cardiac pathologies.
Atrial fibrillation
Unlike flutter, fibrillation (flicker) is characterized not only by an increase in heart rate, but also by a change in its frequency. Electrical impulses that can cause excitation of the atria begin to form not only in one area (sinoatrial node), but also in other areas. The result of this process is a disorganized trembling of the walls of the atria, which has nothing to do with normal contractions. Since the muscle walls cannot contract fully, 10% less blood enters the ventricles. This condition is not dangerous for a healthy person, but atrial fibrillation more often occurs against the background of congenital or acquired heart defects, acute or chronic myocardial diseases. With atrial fibrillation, the pulse at rest can increase to 140-160 beats per minute (the norm is from 60 to 80 beats), and during physical activity it can increase even more.
Description of supraventricular arrhythmia
Supraventricular arrhythmia (SVA) is also defined as atrial or supraventricular. The source of the spread of extraordinary contractions is in the atria, that is, above the ventricles, hence the name of the pathology.
The formation of NFA is based on the formation of a pathological focus of trigger activity, which sends periodic extraordinary impulses. In some cases, the electrical signal is transmitted through the atria or in the atrioventricular node via the reentry mechanism, then a cyclic propagation of the impulse is observed, leading to an acceleration of cardiac activity.
The development of supraventricular arrhythmia can occur against the background of cardiovascular diseases, which is typical for old age, or without visible clinical signs during the formation of the body, that is, in children and adolescents.
If the pathology is associated with other cardiovascular disorders, then it is important to undergo regular examinations with a cardiologist. Otherwise, you will have to find out the dangers of supraventricular arrhythmia from your own experience.
Other violations
Supraventricular heart rhythm disorders are a huge group of pathologies that includes various diseases. The most commonly diagnosed of them are extrasystole and tachycardia, but less common disorders are also identified.
- Ventricular preexcitation syndrome is caused by the formation of additional (pathological) pathways that block the conduction of impulses along the normal atrioventricular pathway. There are several types of such pathways, but they all lead to disruption of the processes of normal polarization and depolarization of the ventricles.
- Sinus bradycardia is a decrease in heart rate. It can reach 50-60 beats per minute or less, while it remains correct.
- Sick sinoatrial node syndrome is a typical disorder in which organic damage to this area is observed. As a result, the patient develops persistent bradycardia, and the pulse does not increase even after physical exertion or the use of atropine.
Most pathologies have a benign course. In some cases, they are chronic and require constant monitoring.
Diagnostic and treatment methods
When diagnosing, it is important to take into account the patient's complaints. They may include increased or decreased heart rate, pain in the heart area, headaches, deterioration of well-being and other clinical signs. It is also necessary to take into account diseases of other organs and systems that preceded the appearance of the first symptoms. However, the most important diagnostic method remains electrocardiography (ECG). Based on its results, you can evaluate the frequency and rhythm of heart contractions, as well as the nature of the conduction of electrical impulses. If organic pathologies are suspected, an ultrasound of the heart is prescribed.
Treatment is prescribed individually. In some cases, simple observation and adherence to a physical activity regimen are sufficient. It is possible to prescribe adrenergic blockers or long-acting calcium antagonists, and in some cases surgical intervention is indicated. It is important to remember that a routine examination by a cardiologist can help identify many disorders at an early stage and provide the most gentle therapy possible.
Prevention of supraventricular arrhythmia
There are certain principles for the prevention of rhythm disturbances that apply to all forms of arrhythmia, including supraventricular;
- Proper nutrition should consist of lean meats, fish, and a sufficient amount of plant foods should be included in the diet.
- Physical activity must be at an acceptable level for the patient so that the heart is supplied with sufficient oxygen and nutrients.
- Maintaining blood glucose and total cholesterol levels within normal limits. Also, body weight must correspond to age and physiological norms.
Video Therapy of extrasystoles and supraventricular tachyarrhythmias
4.75 avg. rating ( 93 % score) - 4 votes - ratings