Thrombophilia during pregnancy without maintenance therapy and preventive treatment in most cases leads to an unfavorable outcome. Although many modern medical sources call thrombophilia a mild risk factor for pregnancy loss, our experience suggests the opposite. The disease provokes repeated miscarriages, delays in fetal development and even fetal death, and promotes placental abruption. In our clinic, patients with this diagnosis are not uncommon. Our happy mothers tell each other that we carry out a natural birth and, under our supervision, the pregnancy ends with the birth of a healthy baby. Pregnancies with a complicated medical history are managed by the chief physician of the clinic, Marine Isakovna Amyan.
According to statistics, thrombophilia during pregnancy is the cause of recurrent miscarriage in 17% of cases when women come to us with the problem of spontaneous miscarriages. The most dangerous thing in this case is that miscarriages occur during the period of 10-12 weeks, during which time most women are not registered at the antenatal clinic, and some women with irregular cycles may not even know that they are pregnant.
Thrombophilia during pregnancy
Amyan Marine Isakovna - associate professor, candidate of medical sciences, chief physician, obstetrician-gynecologist at Diamed Shchelkovskaya
Nowadays, 1-2 miscarriages are considered normal. This is associated with poor ecology, overwork, and poor nutrition. A woman experiences miscarriage twice, gets pregnant again, and can you imagine how the uterus wears out? A woman with her sixth pregnancy came to see me,” Marine Isakovna Amyan, chief physician of the clinic on Shchelkovskaya, obstetrician-gynecologist, gynecologist-endocrinologist, gives an example from her practice. Only one of her pregnancies resulted in childbirth.
The family planned a second baby and could not bear it. Svetlana, that was the patient’s name, was in her eighth week of pregnancy at the time of treatment. The woman did not understand what was happening because she did not experience any symptoms before the miscarriages. The pain began already during the process of spontaneous abortion. All previous unsuccessful pregnancies, the woman was observed in the antenatal clinic, she had a confirmed diagnosis of genetic thrombophilia. As well as a complicated medical history: thyrotoxicosis, nodular goiter, myopia, chronic carriage of infections, including HPV. A woman was not registered until she was 12 weeks old, and she did not nurse until that time; miscarriages happened earlier.
Desperate, she turned to our clinic for help. On the advice of a friend, Svetlana came to me with a history of her illness, documents, tests and research. As I already said, it was the eighth week and the critical period was approaching when miscarriages occurred. The woman was noticeably nervous and worried. Based on the research, the picture immediately became clearer; we prescribed an additional examination for the patient, took blood, and performed an ultrasound. Since Svetlana’s miscarriages occurred in the first trimester, we could not hesitate for a minute. And we started treatment on the same day.
The first time we exhaled, as they say, was when the patient entered the second trimester of pregnancy. Next, we were able to gradually prevent the following possible complications:
- intrauterine growth restriction
- placental insufficiency
- high blood pressure
- premature birth
During pregnancy, we constantly measured blood levels, did ultrasound with a prenatal test, and monitored the fetal heart rate. It was hard work between the doctor and the patient. But we managed. Three months ago, Svetlana became a mother for the second time, gave birth to a beautiful girl, and recently she came to us to introduce her to her long-awaited baby.
Thrombophilia as a cause of obstetric complications.
Oksana Mikhailovna Drapkina , professor, doctor of medical sciences:
– We are temporarily finishing our gastroenterology section and giving the floor to our distinguished guest, Professor Alexander Davidovich Makatsaria. Alexander Davidovich will make a presentation on the topic “Thrombophilia as a cause of obstetric complications.”
Alexander Davidovich Makatsaria , professor:
– Dear colleagues, the term thrombophilia has become widely used in medical and clinical practice since the early 90s, only 20-25 years ago. Thrombophilia was known before, but basically it was known only to a narrow circle of specialists who knew that in 68 a hereditary defect of hemostasis was discovered, which damages the most important anticoagulant link of blood coagulation and, in fact, is a consequence of congenital or hereditary deficiency natural anticoagulant antithrombin III. In the 70s, another defect was discovered - a defect in protein C - the second most important natural anticoagulant, the deficiency of which also predisposes to thrombosis and thrombotic complications. But since the beginning of the 90s, since the discovery of the Leiden mutation, and then the prothrombin mutation, and a little earlier - since the discovery of antiphospholipid syndrome, and a little later - since the discovery of the role of hyperhomocysteinemia in the pathogenesis of complications in clinical practice, they began to talk more often about thrombophilia.
In simple terms, thrombophilia is a hereditary or acquired predisposition to intravascular coagulation, macro, microthrombosis and, as a consequence, microcirculation disorders.
By now it has become known that thrombophilia has become the most important etiopathogenetic factor not only of thrombosis and thromboembolism, but also of the vast majority of pregnancy complications. These include early preembryonic losses, failure of in vitro fertilization, early and late miscarriages, antenatal fetal death, intrauterine growth restriction syndrome, non-developing pregnancy, and stillbirth. All these diseases, all these complications of pregnancy are called fetal loss syndrome, the clinical picture of which is very diverse. It turned out that the most severe forms of gestosis - preeclampsia and eclampsia - can be a consequence of thrombophilia, premature detachment of a normally located placenta. Obstetricians call this disease in a similar way, but if you explain the essence of the disease to a cardiologist or neurologist, then these specialists will call this disease an ischemic stroke or heart attack. It turned out that premature abruption of a normally located placenta occurs very often in patients with thrombophilia; in approximately 80-90% of cases, placental abruption is a consequence of genetic or acquired thrombophilia. Naturally, thrombosis and thromboembolism caused complications of hormonal replacement therapy; complications of hormonal contraception, as a rule, are the result of a hidden hereditary or acquired hemostasis defect predisposing to increased blood clotting.
Thrombophilia influences the occurrence of a number of other systemic syndromes, such as systemic inflammatory response syndrome, metabolic syndrome, disseminated intravascular coagulation syndrome, oxidative stress, and endotheliopathy. One of the manifestations of thrombophilia is antiphospholipid syndrome.
It should be noted that during pregnancy, changes in the functioning of hemostasis occur, therefore a very favorable background is created for the implementation of latent genetic or acquired thrombophilia. But the essence of these physiological changes in hemostasis is that the level of procoagulants - plasma blood clotting factors - increases, the level of natural anticoagulants decreases and the second protective mechanism against thrombosis is somewhat inhibited - this is the fibrinolytic link, fibrinolysis decreases slightly. These changes are very favorable, as I have already said, for the implementation of various forms of thrombophilia.
In general, it should be borne in mind that the course of pregnancy is greatly influenced by genetic thrombophilia, the circulation of antiphospholipid antibodies, and hyperhomocysteinemia. And all these three factors also influence the occurrence of systemic inflammatory response syndrome. Taken together, everything together can be the basis for a number of serious pregnancy complications that pose a threat to the life of the mother.
What is characteristic of thrombophilia? Idiopathic thrombosis is characteristic, recurrent thrombosis is characteristic, especially in people under 50 years of age. A family history of thromboembolic complications is characteristic. This includes, by the way, complications such as strokes, especially ischemic ones, and heart attacks in parents. Thrombosis of unusual localizations: Budd-Chiari syndrome, mesenteric thrombosis, cerebral vein thrombosis. Thrombosis while taking oral contraceptives or hormone replacement therapy drugs. Ovarian hyperstimulation syndrome as a complication of in vitro fertilization. In recent years, another concept has emerged - a new concept. The vast majority of obstetric complications, that is, complications of pregnancy, began to be considered as complications caused by thrombophilia, therefore the presence of such complications as gestosis or preeclampsia, fetal growth restriction syndrome, fetal loss syndrome, premature abruption of a normally located placenta, IVF failures are grounds for testing the patient for the presence of thrombophilia. Thrombophilia is also characterized by the presence of skin necrosis while taking oral anticoagulants, as well as massive obstetric hemorrhage, because thrombophilia can be a kind of precursor to the occurrence of disseminated intravascular coagulation syndrome, the progression of which can lead to severe coagulopathic bleeding.
What are the criteria for thrombophilia? The criteria for thrombophilia are the presence of Leiden mutation, prothrombin mutation, the presence of antiphospholipid syndrome, hyperhomocysteinemia, deficiency of antithrombin III, protein C, protein S. Combined forms of thrombophilia may also exist, which is extremely unfavorable for the treatment (00:09:16) of any disease.
According to our data, we have been dealing with this problem for a long time, and we were among the first in the world to introduce this knowledge into clinical practice. According to the generalized data from the world literature and our data, thrombophilia is a very common cause of complicated pregnancy. This is approximately 75% of cases of fetal loss syndrome. This is 80% of cases of premature abruption of a normally located placenta. This is practically the vast majority of cases of venous thromboembolism. Of course, all these data had a very great influence on changing the tactics of pregnancy management, especially the tactics of managing a second pregnancy, if the previous ones were accompanied by serious complications.
It should be noted that thrombophilia is not only thrombosis. Thrombotic complications of thrombophilia cannot explain all pregnancy complications. There is also the concept of non-thrombotic forms of thrombophilia. Such a clear example of this is the effects of antiphospholipid antibodies and the effects of hyperhomocysteinemia.
It should also be noted that pregnancy and the state of thrombophilia are characterized by a pro-inflammatory status. In general, hypercoagulation, thrombosis and inflammation – these concepts are interdependent. Thus, where there is thrombosis, there is always inflammation. Where there is inflammation, hypercoagulation and thrombosis always occur.
The presence of hyperhomocysteinemia is such a clear example of the nonthrombotic effects of thrombophilia. Hyperhomocysteinemia can also cause thrombosis, but it also causes a number of non-thrombotic effects of thrombophilia. This includes the risk of giving birth to children with fetal malformations, congenital malformations, spontaneous abortions, stillbirth, preeclampsia, placental abruption, fetal growth restriction syndrome, etc.
In the diagnosis of thrombophilia, a very important role is played by the determination of microparticles in the bloodstream. As a rule, in increased quantities, these microparticles, which take part in the formation of thrombosis, inflammation, and are a manifestation of endothelial dysfunction and impaired angiogenesis. As a rule, this occurs with preeclampsia, gestosis, especially HELLP syndrome, premature abruption of a normally located placenta, fetal growth restriction syndrome, and fetal loss syndrome.
I especially want to focus on antiphospholipid syndrome. The relationship between antiphospholipid syndrome, venous thromboembolism, arterial thromboembolism, fetal loss syndrome, preeclampsia and fetal growth restriction syndrome has been well established in numerous studies.
The thrombotic effects of antiphospholipid antibodies consist of a very large number of diverse effects of antiphospholipid antibodies on the body. Thrombotic effects are caused by cellular damage, induction of apoptosis, inhibition of proliferation, suppression of human chorionic gonadotropin, impaired trophoblast invasion, complement deposition, activation of neutrophils, monocytes, overproduction of tumor-necrotizing factor, and impaired degradation of chemokines.
The nonthrombotic effects of antiphospholipid antibodies are manifested by changes in the adhesive characteristics of the preimplantation embryo, damage to the trophoblast, a decrease in the depth of trophoblast invasion, abnormal formation of the trophoblast as a result of direct binding to antiphospholipid antibodies, impaired syncytium fusion, etc.
Thrombotic effects are also caused by the influence of protein C on the protein C system. It is these effects that constitute the damaging effects of antiphospholipid antibodies on a woman’s body.
I would also especially like to note that antiphospholipid antibodies can cause progesterone deficiency, which itself can cause miscarriage and further fetal loss syndrome. It turns out that antiphospholipid antibodies have an antichoriogonin (00:14:26) effect. And the antichoriogonin effect naturally causes disruption of progesterone production. That is why, when antiphospholipid antibodies are circulating, it is extremely important to prescribe replacement therapy with progesterone drugs (the most acceptable of these drugs is utrogestan) with the simultaneous administration of low molecular weight heparin, the best of which is Clexane.
Probably, it should be said about a special form of antiphospholipid syndrome, its catastrophic form - this is the rare, most severe form. Develops in approximately 1% of patients with antiphospholipid syndrome, manifests itself in multiple thromboses of vital organs with the development of multiple organ failure, is a life-threatening condition for the patient, and can underlie a number of emergency conditions such as eclampsia, HELLP syndrome, and hemolytic-uremic syndrome, and septic shock. The circulation of antiphospholipid antibodies in critical conditions is an aggravating factor for the patient. It develops more often in women. Mortality, despite therapy, reaches almost 50%. And it should be noted that optimal therapy has not yet been developed.
Pathological conditions that may be based on catastrophic antiphospholipid syndrome are septic shock, HELLP syndrome, preeclampsia and eclampsia, hemolytic-uremic syndrome, disseminated intravascular coagulation syndrome, systemic inflammatory response syndrome, thrombotic thrombocytopenic purpura.
I would also like to draw the attention of my colleagues to the fact that excessive hypercoagulation from the very beginning of pregnancy, which is always a consequence of hyperthrombinemia, is not only a threat of thrombosis, but it is also a factor that has a significant impact on angiogenesis. Without normal angiogenesis, normal formation of the placenta is unthinkable, therefore anticoagulant therapy is a therapy that is aimed at both preventing thrombosis and preventing angiogenesis.
I would like to make a special comment on this drawing. According to the modern point of view on the pathogenesis of pregnancy complications caused by thrombophilia, it should be noted that complications such as preeclampsia, premature abruption of a normally located placenta, fetal growth restriction syndrome, and fetal loss syndrome develop over a long period of time. There was such a thing as the silent phase of the disease. And this silent phase in the case of thrombophilia lasts a long time, at least a month or two months. It is formed at the time of trophoblast invasion, at the time of pathological trophoblast invasion. The initial genetic or acquired thrombophilia of the mother or fetus affects the remodeling of placental vessels, causes a violation of trophoblast invasion, while the coagulation potential increases, endotheliopathy occurs, there is aggravation of vasoconstriction and activation of the systemic inflammatory response, an abnormal placenta is formed, which results in inadequate fetal growth in the future. -placental and uteroplacental blood flow. The consequence of this can be a wide variety of diseases.
This scheme demonstrates to us the ineffectiveness of therapy at the time of clinical diagnosis of major obstetric complications. Treatment for these conditions is generally ineffective, but prevention is extremely effective. And prophylaxis should be prescribed in risk groups, preferably before the period when trophoblast invasion occurs. The ideal time is the fertile cycle.
The general principles of prevention of thrombotic and non-thrombotic effects of thrombophilia consist of establishing the nature of thrombophilia, specific differentiated prevention, which necessarily includes low molecular weight heparin. Today, Clexane, Hemapaxane, Fragmin, Fraxiparine are used in clinical practice - this is the basic therapy. The second drug for basic therapy is natural progesterone, and then the use of folic acid in cases of hyperhomocysteinemia, the use of a number of drugs, among which the main one is magnesium (Magne-B6 forte).
According to the data we received, in the case where thrombophilia was identified on the basis of a complicated course of the first pregnancy, the use of this therapy, starting from the fertile cycle, allowed us in the vast majority of cases to achieve positive results in the prevention of recurrent fetal loss syndrome, to prevent almost all recurrences. premature placental abruption, prevent severe gestosis, and the occurrence of preeclampsia.
Taking into account thrombophilia and its proper prevention have a miraculous effect on preventing recurrent complications of pregnancy.
I would like to say a few words about the use of magnesium preparations, but first of all, I would like to note the risk groups for developing magnesium deficiency during pregnancy. These are pregnant women with metabolic syndrome, with polycystic ovary syndrome, with diabetes mellitus, with gestational diabetes. These are young primiparas, pregnant women who received oral contraceptives for more than three months before pregnancy, pregnant women with an unbalanced diet, pregnant women with hypertension, pregnant women receiving diuretics, with the exception of potassium-sparing ones. These are pregnant women experiencing chronic nervous or physical stress, pregnant women with a deficiency of B vitamins, pregnant women with fetal loss syndrome, gestosis, fetal malnutrition, a history of premature birth, premature abruption of a normally located placenta or thrombosis. The latter indicates that magnesium is indicated in almost all cases where a history of complications was caused by thrombophilia.
Signs of magnesium deficiency can be cardiovascular, cerebral, musculo-tetanic, visceral and metabolic causes. Quite a long-term magnesium deficiency is a condition for the onset of magnesium-dependent diseases. In obstetric and gynecological practice, vitamin B6 and magnesium deficiencies are often combined. I would like to note that in our modern life the main cause of magnesium deficiency is an unbalanced diet, eating “fast food”, taking a number of modern non-alcoholic drinks, which contribute to the excretion of large amounts of magnesium. Thus, hypomagnesemia in this case is secondary, actually iatrogenic to the intake of “fast food” and a number of alcoholic tonics. And in all these cases, compensation for magnesium deficiency is required.
I would like to note that such a serious complication of pregnancy as eclampsia is a condition that corresponds to the peak of hypomagnesemia; the maximum level of magnesium can decrease by 9 times. 18% of pregnancy deaths in the United States are associated with hypertensive disorders and eclampsia.
With this I will end my speech and leave time for questions.
Drapkina O.M.:
– Thank you very much, Alexander Davidovich, for your master class lecture. Please tell me, is there any early diagnosis of thrombophilia? If, for example, a married couple is planning a pregnancy, is it somehow possible to predict in advance how it will happen?
Makatsaria A.D.:
– Dear colleague, I have already said that this concept is just being introduced into practice. Approximately 5-10 years ago, in Russia we had limited capabilities for diagnosing thrombophilia; naturally, criteria were not developed for who should be diagnosed with thrombophilia. Today this path has already been passed, a path has been passed that allows us today to identify risk groups. Unfortunately, the diagnosis of thrombophilia, in cases where there is no history indicating the risk of thrombophilia, is not carried out in the world. Therefore, I already said in my report that the presence of a history of obstetric complications is an absolute indication for testing for thrombophilia.
Drapkina O.M.:
- Thanks a lot. We received a message from the city of Cheboksary. “Dear Alexander Davidovich, thank you very much for your work “Thrombosis and thromboembolism in obstetric and gynecological practice.” Dr. Ivanova wrote:
Makatsaria A.D.:
- Thanks a lot.
Drapkina O.M.:
“And we have a few questions.”
Makatsaria A.D.:
– Question: “A 56-year-old woman with hyperhomocysteinemia came to see a cardiologist. How to treat? How long to give, in what doses, what drug? How to evaluate? First, let me assess the presence of hyperhomocysteinemia in any person, but especially in a 56-year-old woman. Hyperhomocysteinemia is one of the very serious factors in the occurrence of thrombosis, the progression of atherosclerosis, and the occurrence of ischemic stroke, so it is imperative to use drugs that will reduce the level of homocysteine in the body and in the bloodstream. The best drug is folic acid. In this case of hyperhomocysteinemia, I would recommend a drug that contains a high dose of folic acid - this is folacin along with drugs of group B. The effect should be assessed no earlier than in a month, in two even better, by determining the level of homocysteine in the body. Since I am an obstetrician-gynecologist, I would like to say that I believe that determining homocysteine levels should become a mandatory measure when planning pregnancy, since this will reduce a number of pregnancy complications that are caused by hyperhomocysteinemia.
“Diploma education...” We do not do this, you can contact the Russian Center for Obstetrics and Gynecology, where we hold events within the framework of the Russian Association of Obstetricians and Gynecologists.
Magnesium supplements are not contraindicated during pregnancy.
Treatment and prevention of thrombophilia at Diamed
Thrombophilia during pregnancy can cause miscarriage. But there are a number of other factors that affect normal pregnancy. You can never look at any one disease in isolation. Only an integrated approach and comprehensive constant monitoring can help you fulfill the most important dream of your life - to become parents. Nothing is impossible for medicine; accurate diagnosis and correct effective treatment programs will definitely help you cope with any ailment. The main thing is to come to the doctor, come to our clinic, and expect that your second or third pregnancy will end successfully. With every miscarriage, you lose health and reduce your chances of having a healthy baby.
If you want to get an appointment with Marine Isakovna, call 8 or leave a request in the appointment form on our website, located at the end of the article. You can also choose the clinic closest to you, where you will receive equally qualified assistance:
- Clinic in Mitino
- Clinic in Tekstilshchiki
- Clinic in Maryina Roshcha
Prevention of thrombophilia
- Drink more fluids and avoid dehydration, which can promote blood clots.
- Move every hour, do not sit still for a long time.
- Be careful with medications after pregnancy. Birth control pills or hormone replacement therapy may increase the risk of blood clots.
- Keep your weight normal. Being overweight or obese increases your risk of developing thrombophilia.
- Don't smoke, this will keep your blood vessels healthy.
Source . The article was prepared based on materials provided by obstetrician-gynecologist, candidate of medical sciences, associate professor of the department of postgraduate training at Tula State University Amyan Marine Isakovna. Doctor of the highest category, Excellent healthcare worker, work experience in the specialty since 1994. Published 45 scientific works, including 5 methodological recommendations, 5 educational electronic disks, 4 methodological manuals, 6 educational manuals, 3 analytical reports. Expert on reproductive health of the United Nations Population Fund. ALSO instructor in emergency obstetric care. Evidence-based methodologist medicine.
Why is diagnosing pregnancy complications important?
There is currently no cure for preeclampsia. Therefore, a number of complications require correct diagnosis and prediction of complications and further correct prevention. We can say that it is correct only if we can find out at least proven risk factors.
In patients with thrombophilia, no matter what complications we talk about, be it a severe form of preeclampsia or recurrent miscarriage, because recurrent miscarriage today has received a slightly different name due to the emergence of antiphospholipid syndrome, and this is fetal loss syndrome, which combines various reproductive losses, starting from early stages, ending with late stages and neonatal death, and so on.
What happens in the body of a woman with thrombophilia?
The reason for thrombophilia is that during pregnancy a third circle of blood circulation is formed - the placental one.
The system that connects mother and fetus does not have its own capillaries, which is why blood flows directly into the vessels of the umbilical cord and placenta. Due to this, the child receives oxygen and nutrients as quickly as possible. But if a woman has problems with blood circulation, then such direct blood flow will strengthen them.
Pregnant women have increased blood clotting. This is necessary so that the expectant mother does not bleed during childbirth. But with thrombophilia, the blood already clots too quickly. A further increase in coagulability leads to the formation of blood clots, especially after 10 weeks. They clog the vessels between the maternal organ and the placenta, and between the fetus and the placenta. As a result, the child does not receive the required amount of nutrients and, most importantly, oxygen.
The consequences may be as follows:
- Miscarriage, stillbirth, fading pregnancy. Such situations are caused by oxygen starvation of the fetus (hypoxia).
- Developmental defects in a child. More often than others, problems arise with the cardiovascular and nervous system.
- Severe toxicosis. The expectant mother suffers from edema, high blood pressure, and in severe cases from eclampsia - severe convulsions that resemble epileptic seizures. To save a woman’s life, doctors have to resort to surgical delivery.
- Detachment of the altered placenta. Placental abruption is often accompanied by severe bleeding, which threatens the life of the expectant mother.
Thrombophilia is not limited only to blockage of placental vessels. Since the coagulability of all blood increases, blood clots can form in any vessels. Pregnant women often develop blood clots in the veins and arteries of the legs. The fact is that the uterus, which has increased in size, puts a lot of pressure on the veins in the groin, and due to the outflow of blood from the placenta, the vessels experience increased stress. This leads to stagnation of blood, deformation of the walls of the veins and, as a result, the formation of blood clots. Unfortunately, during pregnancy, the likelihood of developing blood clots increases by a record 200%. Women diagnosed with varicose veins are primarily at risk.
However, there is another danger - the formation of blood clots in the brain and pulmonary artery. This type of thrombosis is especially dangerous as it can lead to death.
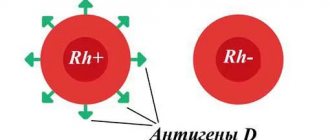
Types of thrombophilias
The types of disease are presented in the table.
| Type of disease | Causes |
| Acquired | Concomitant diseases - polycythemia, heart disease, taking hormonal drugs, past infections |
| Gennaya | Hereditary pathologies and mutations affecting blood clotting. It occurs at the gene level and is expressed by a congenital increase in blood clotting factors. Often found in close relatives |
| Immune | Autoimmune disorders, in which the mother’s body produces antibodies to her own tissues, and alloimmune, manifested by the production of antibodies to fetal tissues |
| Vascular | Atherosclerosis, vasculitis, varicose veins, diabetic vascular lesions |
| Hemodynamic | Disruption of blood flow through vessels caused by decreased blood pressure and increased blood viscosity |
| Hematogenous | Acquired disorders of the hematocoagulant, anticoagulant and fibrinolytic systems |
The disease can develop in severe form. Most often this happens due to congenital pathologies (for example, a tendency to form blood clots).
Another risk factor is age: in women over 35 years of age who are giving birth for the first time or already have many children, thrombophilia, regardless of the type, develops more severely. Provoking factors can be abortions, severe chronic diseases, and recurrent miscarriages.
Dipyridamole and Curantil
If we are talking about aspirin resistance or the inability to reduce platelet aggregation activity with aspirin, we can resort to prescribing an additional drug during pregnancy: Dipyridamole or Curantil, phosphodiesterase inhibitors. They have a different mechanism of action, unlike aspirin. In addition, Dipyridamole has effects on the endothelium, which is also extremely important. The combination of “Aspirin + Curantil” can be used in patients with high platelet activity. This is one of the advantages of the fact that we can use Curantil together with Aspirin. We also use concentrates of natural anticoagulants.
In a rather rare group of patients with genetic thrombophilia, with a deficiency of antithrombin 3, protein C, in whom, in addition to anticoagulant therapy with low molecular weight heparins, it is necessary to use replacement therapy with anticoagulants that they lack genetically - thrombin 3, protein C, and so on.
If we are talking about patients with recurrent miscarriage, there is no question whether to use progesterone drugs or not. Definitely apply. And this was repeatedly voiced at recent international congresses on controversies in obstetrics and gynecology.
Low molecular weight heparins
The general principles for the prevention of thrombotic and non-thrombotic effects of thrombophilia are, of course, the establishment of the nature of thrombophilia and the use of low molecular weight heparin as basic drugs. There are a lot of them today, much more than there are in our country in the world. But among the low molecular weight heparins that are present in our country, these are the well-known Enoxaparin sodium, Clexane, Hemopaxane, Fraxiparin, Calcium Nadroparin, etc.
All of them are low molecular weight heparins. The molecular weight, pharmacological effects, pharmacodynamics, and pharmacokinetics of these drugs may differ.
They are highly effective during pregnancy, do not pass through the placenta, and can be used in patients with thrombophilia to prevent both thrombotic and typical obstetric, non-thrombotic effects of thrombophilia.
Does genetic thrombophilia affect the characteristics of childbirth?
This pathology is not a reason to choose, for example, a cesarean section. The method of delivery is chosen as in other cases.
Taking tests
The number and time of tests is determined by the gynecologist. The result of donating blood from a vein is usually ready the next day (urgent analysis is available).
The state of the blood coagulation system is assessed by:
- hemostasiogram;
- platelet aggregation;
- D-dimer.
Which medical specialist prescribes the course of treatment?
If the gynecologist is sufficiently qualified, no additional consultations are required for treatment.
Does the gynecologist understand hemostasis?
The medical center employs gynecologists, whose level of qualifications and experience in medical practice undoubtedly meet the necessary requirements.
Treatment of thrombophilia
Before therapy, two tasks are set: firstly, it is necessary to eliminate blood clots, and secondly, to remove the cause that led to their formation.
Treatment usually includes:
Also, women who are at high risk of developing blood clots are recommended to wear compression stockings; they support the veins and help maintain their elasticity. It is advisable to lie down with your legs raised and placed on soft support.