Venous thrombosis is a pathological process characterized by the formation of blood clots – thrombi – in the venous bed. Clot formation can occur in both the deep and superficial venous systems, affecting veins of various sizes. Depending on the size of the clot, the lumen of the vessel is partially or completely blocked, disrupting or stopping the free flow of blood.
Blood clots detached from the vascular wall pose a great threat to human health and sometimes life. They are capable of blocking the feeding arteries of the lungs, intestines, brain and other organs, leading to dysfunction of the latter. This circumstance forces us to pay serious attention to the problems of preventing thrombosis, as well as to develop effective methods for treating venous thrombosis in order to prevent thrombotic complications.
Medical vascular surgeons have in-depth knowledge and experience in diagnosing various forms of venous thrombosis.
Briefly about the treatment method
Removing blood clots (thrombectomy) can be a separate type of treatment, but more often it is a component of it. Vessel thrombosis can form as a result of its narrowing or expansion; a thrombus fragment can be brought from other arteries or the heart. Thrombotic masses in the lumen of blood vessels block blood flow and cause circulatory failure, which can lead to gangrene of an organ or limb. Modern vascular surgery has a number of technologies that make it possible to remove thrombotic masses from vessels.
Size matters
Which blood clot is the most dangerous? The larger the vein and the larger the size of the clot, the higher the chance of thromboembolism. The most dangerous are proximal (located close to the center of the body) blood clots - in the veins of the thigh, pelvis and retroperitoneum. The incidence of embolism in this location is above 50%.
A small peripheral blood clot (for example, in the lower leg) can also become hypothetically dangerous. It also migrates to the pulmonary arteries and disrupts blood flow. Minor embolisms are asymptomatic in 75% of cases, but they still pose a threat to life, albeit a delayed one. Sooner or later, if left untreated, they can lead to circulatory problems and, in some cases, death. Therefore, any identified blood clot in the veins requires active treatment.
Advantages of treatment at the ISC
Our clinic uses both traditional technologies and minimally invasive modern methods to remove blood clots.
- Fogarty catheter thrombectomy is a traditional method of removing blood clots from an artery using a balloon probe. The principle is to pass the probe in a folded state through the thrombus, followed by inflating the balloon and pulling it out along with the thrombotic masses.
- Rotarex is a technology for removing chronic blood clots from the arteries. The principle is based on the splitting of blood clots by a special probe head rotating at high speeds and its simultaneous suction by a special spiral mechanism (presented in the film). The technology opens up unlimited possibilities for treating severe vascular pathology without incisions.
- Aspirex is a similar technology for removing fresh blood clots from arteries and veins. Suitable for the thinnest vessels, does not damage venous valves. A special spiral suction atraumatically removes all blood clots from the vessel if the thrombosis period does not exceed 2 weeks.
Causes of blood clots
Several factors play a role in the mechanism of thrombosis, consideration of which is necessary to understand the essence of the process and determine the principles of treatment of thrombosis. These factors are:
- increased blood clotting;
- slowing down the speed of venous blood flow;
- damage to the walls of blood vessels.
High blood clotting can be caused by hereditary and age-related factors, and can also be a companion to certain diseases (autoimmune processes, thrombophilia, acute respiratory infections) and physiological conditions of the body (pregnancy). Increased clotting is also caused by low physical activity, taking oral contraceptives and diuretics.
Disruption of venous blood flow is observed with varicose veins, narrowing of their lumen due to the development of inflammatory processes, as well as with various types of cardiac pathology (heart failure, arrhythmias). A sedentary lifestyle and sedentary work also contribute to a decrease in venous outflow.
Violation of the integrity of the inner lining of blood vessels occurs due to mechanical injuries, including surgical, infectious and inflammatory lesions. Damage to the vascular intima is not a prerequisite for the formation of a blood clot. The first two reasons are often sufficient for this. However, it significantly accelerates the process of thrombus formation.
Indications and contraindications for the treatment method
- Acute arterial embolism - blockage of an artery by a blood clot brought from other places. The most common procedure is open embolectomy with a Fogarty probe through an approach below or above the blockage.
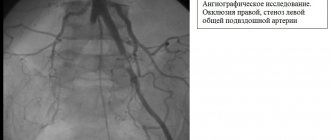
- Arterial thrombosis against the background of atherosclerotic plaques (atherothrombosis). It is dangerous to use a Fogarty probe in this case, as the artery wall may collapse. Rotarex allows you to remove thrombotic masses from an artery affected by atherosclerosis without damaging the vascular wall. In addition, soft atherosclerotic plaques are cut off. After removing the thrombus, angioplasty and stenting of the affected arteries are necessary.
- Removal of blood clots from vascular prostheses. Can be performed from open approaches using various modifications of Fogarty catheters. Most often, blood clots are removed from large vascular prostheses (aorto-femoral) as part of repeated operations.
- Removal of blood clots from previously installed stents. Stent thrombosis often requires repeated interventions. It is not possible to use a Fogarty balloon to remove blood clots from stented areas of arteries, as it will rupture against the stent or damage the arterial wall. For such thromboses, it is much more effective and safer to use Rotarex technology.
Wait, who's coming?
How to detect thrombosis at an early stage? More often it “starts” in the veins of the leg and is accompanied by quite tolerable local pain and swelling. In an unfavorable scenario, the blood clot increases in size, involving the veins of the thigh and pelvis. Gradually, massive swelling, redness of the skin, bursting pain, and swelling of the saphenous veins appear. From the moment the first symptoms appear until you see a doctor, it usually takes 5-10 days. The exception is iliofemoral thrombosis, which makes itself felt immediately - with pronounced swelling and noticeable pain.
“Silent” thrombosis (with a complete absence of symptoms) can occur in bedridden patients (after surgery or paralysis) or if a blood clot forms in the pelvic veins (usually this occurs during pregnancy and childbirth, in the postpartum period, when taking oral contraceptives). In such situations, the first sign of disease may be pulmonary thromboembolism “without a clear source.”
Article on the topic
There is a cork in the vessel. Where did the child get thrombosis?
Preparing for treatment
In the case of acute thrombosis, surgery to remove blood clots should be performed according to urgent indications in order to save the limb. The urgency of the operation depends on the degree of circulatory failure and the duration of the disease. Preparation for such an intervention is minimal.
- General blood and urine analysis
- Biochemical blood test (urea, creatinine, electrolytes)
- ECG
- Echocardiography - to identify the causes of thrombosis
- Ultrasound of the arteries of the affected limb and possible aneurysms.
- Installation of a urinary catheter
- Installation of an intravenous line catheter
- Cleansing enema
- Shaving surgical access sites
Thrombectomy techniques
To perform thrombectomy, professional equipment is used, as well as specialists who have undergone special training in this profile. Currently, the following thrombectomy techniques are used in practice:
- traditional,
- endovascular.
The decision to choose one or another method of surgical intervention is made by the doctor. This decision depends on the following factors:
- places where blood clots are located,
- causes of blood clots,
- on the condition of the blood vessels,
- age-related changes in the body.
How the treatment method works
Removal of blood clots using a Fogarty probe
An open thrombectomy using a Fogarty probe is performed through the incision. The incision is usually made below the site of thrombotic blockage of the artery, since the removal of blood clots is easier through the blood flow. If the patient has thrombosis of the aorta or iliac arteries in the abdomen, then the incision is made in the groin area; if thrombosis is in the popliteal artery, then the access is made on the lower leg or foot. After isolating and assessing the condition of the artery, a 3-5 mm incision is made on it, into which the Fogarty balloon probe is inserted in a compressed state. For better elasticity, a metal conductor is installed in the probe, which is removed after passing the probe above the blood clot. A syringe is attached to the probe, through which the balloon is inflated. After this, the surgeon removes the inflated balloon, which pushes the thrombotic masses towards the cut artery. Pressure of the blood above the clot helps the process of removing the clot. After removing the clot, the procedure is repeated to ensure complete removal. Vascular clamps are placed on the artery and the hole in it is sutured with a vascular suture. After this, the wound is sutured layer by layer.
This simple operation helps well with acute blockage of intact arteries by thromboembolism (a blood clot brought from the heart or from larger arteries), however, if thrombosis of arteries affected by atherosclerosis occurs, then thrombectomy with a Fogarty probe becomes impossible or even dangerous, since the probe easily breaks on sharp edges atherosclerotic plaques or can get caught on the plaque and tear it. Therefore, for such cases, we use other methods of removing blood clots.
Removing blood clots with a Rotarex Straube probe
The Rotarex Straube probe allows you to clear the artery of blood clots without resorting to a surgical incision, through a puncture of the artery. At the same time, this probe does not damage the walls of the artery, carefully removing thrombotic masses and freeing the lumen of the vessel. The principle of operation is to crush the clot with a rotating probe head and suck its particles into the lumen of the probe and remove them from the lumen of the vessel into a special bag. The use of Rotarex Straube is possible even in cases of chronic thrombosis due to atherosclerotic and diabetic arterial lesions. The Rotarex Straube probe clears blood clots from the vessel, but does not remove atherosclerotic plaques, therefore, to restore the lumen of the vessels, angioplasty and stenting of narrowed arteries of the leg are performed if necessary. The Rotarex Straube endovascular thrombectomy procedure is performed without incisions, only through a puncture of the artery wall, so the main method of pain relief is local anesthesia. Probe thrombectomy is indispensable when removing blood clots from intestinal arteries with mesenteric thrombosis. Considering the severe general condition of patients with this pathology and the difficulties with access to the mesenteric arteries, thrombectomy with a probe from the initial parts of the superior mesenteric artery is the preferred method of restoring blood circulation in the intestine.
Then you will find out...
2/3 of venous thrombosis are asymptomatic or with mild symptoms. A person is bothered by moderate pain in the leg and slight swelling, but not so severe as to force him to see a doctor. Of the three cases of thrombosis, one progresses, and two resolve spontaneously.
However, this does not always mean that resolved thrombosis has passed without a trace. Even in this case, irreversible changes occur on the wall and valve of the affected vein, which lead to the development of chronic venous insufficiency. With duplex scanning of blood vessels, doctors often see post-thrombotic changes in the deep veins of the leg in patients who have never been diagnosed with venous thrombosis.
Blood control and nutrition without “greens”. A doctor on how to live with thrombosis Read more
Possible complications during treatment
The following complications are possible when using a Fogarty probe:
- Rupture of the inner wall of the artery with its dissection and secondary thrombosis
- Tearing off the probe head and leaving it in the lumen of the artery
- Perforation of an altered artery wall with a probe with internal bleeding
- Complications associated with access (hematoma, lymph accumulation, wound suppuration)
Such complications are quite rare. Their frequency decreases as clinical experience with thrombectomies accumulates. In our clinic, we have not observed such complications over the past five years.
Complications of Rotarex thrombectomy:
- Dissection of the arterial wall due to rough passage of the probe
- Transfer of pieces of blood clots to small arteries below the site of thrombosis
- Formation of hematoma along the artery
Such complications are usually identified during the operation and are usually corrected immediately.
Prognosis after treatment method
Arterial thrombosis is a complication of various diseases. This means that removing a blood clot (thrombectomy) is an intervention that eliminates complications. Thus, the prognosis after treatment depends on eliminating the causes of thrombosis. If this is thrombosis associated with narrowing of the arteries, then restoration of the lumen by angioplasty and stenting eliminates the causes of thrombosis and provides a good long-term prognosis. If thrombosis or thromboembolism is associated with diseases of other arteries or the heart, then treatment of these diseases is necessary to prevent repeated episodes of blood clot transfer.
Rehabilitation after surgery
After thrombectomy, the patient will be able to return to a full life only after a couple of days. Next, drug treatment is carried out. The attending physician prescribes the following medications to the patient:
- blood thinner tablets,
- drugs that restore veins, blood vessels,
- ointments that prevent the formation of clots,
- vitamin and mineral complexes.
To avoid the development of complications after surgery, you should follow the advice of your doctor:
- maintain an active lifestyle,
- wear elastic clothes,
- maintain proper nutrition,
- carry out physiotherapeutic procedures,
- Avoid visiting bathhouses and saunas for a while.
Observation program after treatment method
After removing blood clots and eliminating the causes of their occurrence, the patient needs to be monitored by a vascular surgeon. While in the hospital, the surgeon evaluates circulatory compensation and blood flow velocity using Doppler ultrasound.
Upon discharge, the patient is prescribed antithrombotic therapy, depending on the causes of thrombosis. These can be drugs such as Plavix, warfarin, aspirin.
A month after discharge, it is necessary to conduct a control duplex ultrasound scan of the arteries to assess the condition of the restored segments and circulatory compensation. It is also necessary to evaluate possible sources of thromboembolism (cardiac cavities, aorta) using echocardiography.
Subsequently, the patient must repeat ultrasound examinations and undergo blood clotting tests (APTT, TV, platelet aggregation) twice a year.
Who to look for?
Venous thrombosis is a multifactorial disease that occurs under unfavorable circumstances. Today it is impossible to say for certain who is at risk of thrombosis and who is not (only in some cases a predisposition to thrombosis can be identified using a coagulogram - a comprehensive analysis of blood clotting indicators).
Article on the topic
Life without traffic jams. Russian scientists against thromboembolism Classic factors that provoke the appearance of blood clots include obesity, air travel, dehydration, long stays in a forced position, pregnancy, varicose veins (deep veins) and taking oral contraceptives.
This is only partly true. These circumstances can indeed lead to the formation of blood clots, but only with a complex effect. For example, if you sit motionless in an uncomfortable position for 9 hours on a plane and refuse drinks for the entire flight, while you suffer from obesity, varicose veins and take contraceptives, the chance of getting off the plane with a blood clot is really quite high. But if the matter is limited to one thing (for example, varicose veins or taking contraceptives), you risk no more than other people.
Surgeries and injuries (especially in combination) are considered truly dangerous factors. Such blood clots are considered clinically induced, so all herbal and post-operative patients are screened for the presence of blood clots.
In 10-20% of patients, thrombosis can serve as the first sign of malignancy. In patients over 50 years of age, when clinically unprovoked thrombosis is detected, an in-depth search for cancer is recommended.
Dissolve the clot. What foods improve blood quality Read more